Journals
Treatment of Pulmonary Hypertension in POEMS Syndrome with Autologous Stem Cell Transplantation
A B S T R A C T
POEMS, a rare paraneoplastic syndrome, can cause pulmonary hypertension (PH). PH, diagnosed through echocardiogram in patients with POEMS, is known to improve after autologous stem cell transplantation (ASCT). However, similar accounts of PH, diagnosed through right heart catheterization (RHC), the gold standard diagnostic test for PH, do not exist. We report the case of a 65-year-old female who presented with dyspnea and burning pain in feet. Physical examination was unremarkable, while basic investigations revealed an elevated protein-albumin gap. This prompted further tests that led to the diagnosis of POEMS syndrome. Echocardiogram was additionally obtained and raised concern for PH. RHC was hence performed and confirmed the diagnosis of PH secondary to POEMS syndrome. The patient was treated with ASCT following which her dyspnea got better and repeated RHC revealed improved hemodynamics. This report highlights the first case of PH secondary to POEMS syndrome, which demonstrated improvement in hemodynamics, measured by RHC, following ASCT.
Keywords
Pulmonary hypertension, POEMS syndrome, autologous stem cell transplantation
Introduction
POEMS is a rare paraneoplastic syndrome that occurs secondary to a plasma cell dyscrasia (PCD) and is characterized primarily by polyneuropathy, organomegaly, endocrinopathy, monoclonal gammopathy and skin changes (Table 1). Along with affecting various other organs, POEMS is associated with significant pulmonary morbidity. In addition to changes in lung function such as restriction and decrease in diffusing capacity, patients with POEMS can also be affected by, WHO Group V Pulmonary Hypertension (PH) [1, 2]. Management of patients with POEMS syndrome is aimed at treating the underlying PCD. This has historically been achieved successfully through different treatment modalities such as chemotherapy and radiotherapy. These methods of treatment, have in various cases, also been associated with improvement in PH seen with POEMS syndrome [3, 4]. Autologous stem cell transplantation (ASCT) is another viable option for treating PCD [5]. However, due to poor pulmonary function being a relative contraindication for the procedure, patients with POEMS may often be precluded from undergoing ASCT.
Table 1: Diagnostic criteria for POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal protein, Skin changes). Diagnosis requires the presence of both mandatory majors, at least 1 other major and 2 minor criteria.
|
MANDATORY MAJOR CRITERIA |
Polyneuropathy |
|
Monoclonal plasma proliferative disorder |
|
|
OTHER MAJOR CRITERIA |
Sclerotic bone lesions |
|
Castleman disease |
|
|
Elevated serum Vascular Endothelial Growth Factor (VEGF) levels |
|
|
MINOR CRITERIA |
Papilledema |
|
Organomegaly (splenomegaly, lymphadenopathy etc.) |
|
|
Extravascular volume overload (pleural effusion, peripheral edema etc.) |
|
|
Skin changes |
|
|
Endocrinopathy (adrenal, thyroid, pituitary etc.) |
|
|
KNOWN ASSOCIATIONS |
Thrombocytosis |
Of note, rare accounts of ASCT being used to manage PH associated with POEMS syndrome do exist. However, PH in these patients was diagnosed and monitored through echocardiogram (ECHO), which is known to be less precise and accurate than right heart catheterization (RHC) [6]. We thus report the first case of a patient with POEMS syndrome and associated PH, diagnosed through RHC, who demonstrated an improvement in her PH after undergoing ASCT.
Case Description
A 65-year-old female with no prior medical history was evaluated in the clinic for worsening pain in bilateral feet over the past one year. She described the pain as burning in nature, radiating from toes to her ankles with no associated weakness, neurological deficits or correlation with activity. On questioning, she also endorsed swelling in lower extremities (LE) and new onset of shortness of breath (SOB) on moderate exertion (NYHA Class III). She further denied experiencing any concurrent chest pressure, dizziness or syncope with her symptoms. On cardiovascular examination, the patient was noted to have normal heart sounds with no jugular venous distension. Lung auscultation was remarkable for equal air entry in all lung fields with no added sounds. She was, however, noted to have 1+ pitting edema bilaterally on her LE with no tenderness to palpation and preserved sensory and motor function. An additional exam also revealed Raynaud’s changes in the fingers of her upper extremities along with inguinal lymphadenopathy.
Given the non-specific physical exam findings, further diagnostic tests were ordered to determine the etiology of the patient’s presenting complaint. EMG of the LE was performed and confirmed demyelinating peripheral neuropathy. Concurrently, basic blood tests were obtained with a protein albumin gap elevation to 5.2 g/dL on comprehensive metabolic panel and thrombocytosis to 508,000/µL on complete blood count, being noted. To further investigate the increased protein-albumin gap, serum protein electrophoresis (SPEP) was performed and proved to be remarkable for the IgA band and lambda restriction. In light of the neuropathy, Raynaud’s changes, inguinal lymphadenopathy and positive SPEP results, suspicion for monoclonal gammopathy and possible POEMS syndrome arose. For this reason, vascular endothelial growth factor (VEGF) levels were obtained and were found to be elevated to 6227 pg/mL. Concurrently, bone marrow biopsy (BMB) was performed with pathology revealing hypercellular marrow along with atypical megakaryocytic hyperplasia and lambda-restricted plasma cells, that comprised 15% of cellularity. Following confirmation of PCD and neuropathy, on BMB and EMG respectively, diagnosis of POEMS syndrome was made and further affirmed through PET scan, which demonstrated sclerotic foci in the patient’s spine and pelvic bones.
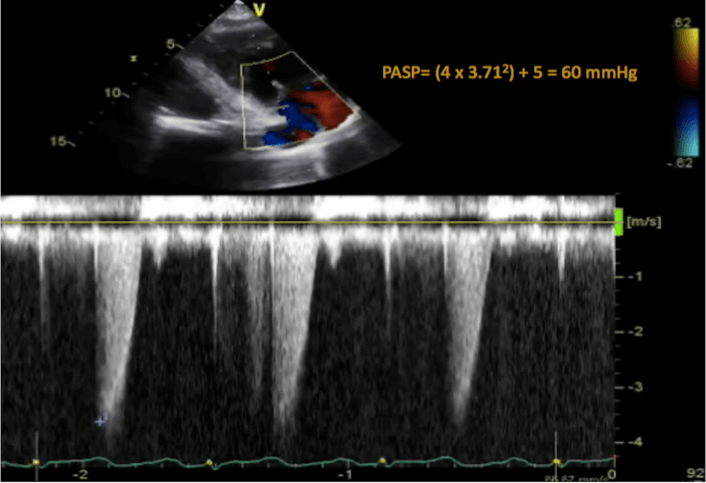
Given complaint of SOB and LE edema along with the known high prevalence of PH in patients with POEMS syndrome, an ECHO was subsequently performed; the results of which were notable for elevated pulmonary artery (PA) systolic pressure (PASP) to 60 mm Hg with no valvular abnormalities and normal biventricular size and function (Figure 1). Concern for PH thus increased, leading to right heart catheterization (RHC) being performed (Table 2). Results of RHC revealed hemodynamic measurements consistent with vasoreactive pre-capillary PH. To further delineate the etiology of PH, pulmonary function tests were obtained and were notable for normal lung volumes and spirometry with moderately reduced diffusion capacity to 32%. Simultaneously, a computed tomography (CT) scan of the chest was performed and was found to have no parenchymal changes. Due to no other identifiable cause for PH on the aforementioned extensive workup, the patient was diagnosed with WHO Group V PH secondary to POEMS syndrome.
Figure 1: Tricuspid regurgitation signal on echocardiogram showing a peak velocity of 3.71 m/s and pulmonary artery systolic pressure (PASP) of 60 mm Hg.
Table 2: Hemodynamic parameters obtained during right heart catheterization before and after autologous stem cell transplant.
|
|
RHC BEFORE ASCT |
RHC AFTER ASCT |
|
RA PRESSURE (mm Hg) |
5 |
3 |
|
RV PRESSURE (mm Hg) |
73/6 |
45/5 |
|
PA PRESSURE (mm Hg) |
70/20 |
45/15 |
|
MEAN PA PRESSURE (mm Hg) |
42 |
27 |
|
PA WEDGE PRESSURE (mm Hg) |
8 |
8 |
|
PA PRESSURE AFTER NO (mm Hg) |
42/11 |
- |
|
MEAN PA PRESSURE AFTER NO (mm Hg) |
27 |
- |
|
PVR (woods units) |
7 |
3.8 |
|
CARDIAC OUTPUT (L/min) (FICK) |
4.9 |
5 |
|
CARDIAC INDEX (L/(min-m^2)) (FICK) |
2.84 |
2.95 |
RA: Right Atrium; RV: Right Ventricle; PA: Pulmonary Artery; PVR: Pulmonary Vascular Resistance; RHC: Right Heart Catheterization; ASCT: Autologous Stem Cell Transplant.
Following the diagnosis of PH, the patient was started on vasodilator therapy with sildenafil 20 mg thrice daily. After the initiation of sildenafil, during follow-up evaluation, the patient reported improved exercise tolerance and was further noted to have preserved right ventricular function on ECHO. Two weeks following the repeated ECHO, the patient was admitted to the hospital and successfully underwent ASCT for the treatment of her PCD.
Following ASCT, the patient was monitored closely as an outpatient and continued to do well. Repeat VEGF levels obtained four months after transplant were noted to be elevated to 795 pg/dL with a remarkable decline relative to those obtained prior to transplantation. Due to the persistently increased VEGF levels, BMB was however performed again and revealed decreased cellularity of lambda restricted plasma cells to 5%. At the same time that these repeat studies were performed, the patient reported remarkable improvement in her dyspnea on exertion (NYHA Class II) and LE edema. ECHO was hence repeated and revealed PASP to 42 mm Hg. In light of overall progress noted on ECHO and symptoms, sildenafil was discontinued and RHC was repeated a week after stopping the medication (Table 2). While hemodynamic parameters on repeat RHC were still consistent with mild pre-capillary PH, they did demonstrate a marked improvement from those obtained prior to ASCT. After the repeated evaluation, the patient was restarted on the same dose of sildenafil as before and had since then continued to do well, such that she has returned to work and is independent with activities of daily living.
Discussion
PH can occur in 27-48% of patients with POEMS syndrome [1, 3, 7]. Pathogenesis of PH in these patients is however still unclear. It is postulated that the overexpression and production of inflammatory cytokines is likely the cause of plexiform lesions and subsequent vasculopathy noted in PH associated with POEMS syndrome [2, 8-10]. VEGF, a key pro-inflammatory cytokine in POEMS syndrome, is known to cause endothelial proliferation, activation of smooth muscle cells and dysfunction of the vascular endothelium in patients with idiopathic pulmonary arterial hypertension (PAH). It is for the same reasons that it is implicated in causing PH in patients with POEMS syndrome [8, 11-15]. Another factor that supports this hypothesis is the improvement in PH in patients with POEMS syndrome who were treated with the anti-VEGF antibody, bevacizumab [16, 17]. Idiopathic PAH, characterized by remodeling of the distal pulmonary arteries and subsequent increase in pulmonary vascular resistance, is more often than not relatively incurable, such that most patients warrant lifelong treatment with PAH-specific pulmonary vasodilatory medications. PH associated with POEMS, however, appears to be a form of the disease outside this norm; with reports of cases demonstrating resolution of PH after treatment of the underlying PCD with radiotherapy or chemotherapy [3, 4].
Another modality utilized to treat PCD is ASCT, which has also been demonstrated to be successful in managing patients with POEMS syndrome [5]. While ASCT has been validated to be a potential therapeutic option for POEMS syndrome, there are rare accounts of it being used to treat PH associated with this syndrome. Furthermore, the cases in the past that detailed improvement in PH with ASCT, all used ECHO to diagnose and monitor these patients [6]. Unlike ECHO, RHC is known to be more accurate in detecting changes in hemodynamics and is hence the gold standard for diagnosis of PH [18, 19]. It is thus important to note that our case is the first to report the use of ASCT to successfully manage both POEMS syndrome as well as associated PH, that was diagnosed through RHC. As demonstrated in our case, ASCT did not only help to treat the underlying PCD but also led to the improvement in the patient’s PH and associated symptoms. While the patient’s hemodynamic parameters did improve remarkably after transplantation, the PH did not resolve completely and she still required low dose pulmonary vasodilator therapy. It is our hypothesis that this is likely due to her incomplete response to ASCT with residual disease and PCD, which was still evident on repeat BMB and led to the subsequently elevated VEGF levels and persistent PH.
Patients with POEMS syndrome have high morbidity and mortality with those who have concurrent PH being predisposed to worse outcomes and survival. The median survival of patients with PH secondary to POEMS syndrome was reported to be 54 months by one study while another reported a hazard ratio for the survival of 3.99 in these patients [7, 20]. However, swift treatment of the underlying PCD is associated with better outcomes, such that patients who are treated with ASCT have improved survival, with one study reporting a 5-year overall survival of 94% in patients with POEMS syndrome treated with ASCT [21]. While ASCT has been proven to be a life-prolonging treatment option for POEMS syndrome, our case demonstrates that in patients with PH secondary to POEMS syndrome, it may assist in doing so by also treating the associated PH. Thus, in patients with POEMS syndrome and PH, who are appropriate candidates for transplantation, we propose that ASCT be strongly considered as a treatment option.
Article Info
Article Type
Case ReportPublication history
Received: Wed 05, Aug 2020Accepted: Wed 26, Aug 2020
Published: Mon 31, Aug 2020
Copyright
© 2023 Jean M. Elwing. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.04.18
Author Info
Humna Abid Memon Jean M. Elwing
Corresponding Author
Jean M. ElwingDepartment of Pulmonary Critical Care Medicine, University of Cincinnati, Cincinnati, Ohio, USA
Figures & Tables
Table 1: Diagnostic criteria for POEMS (Polyneuropathy, Organomegaly, Endocrinopathy, Monoclonal protein, Skin changes). Diagnosis requires the presence of both mandatory majors, at least 1 other major and 2 minor criteria.
|
MANDATORY MAJOR CRITERIA |
Polyneuropathy |
|
Monoclonal plasma proliferative disorder |
|
|
OTHER MAJOR CRITERIA |
Sclerotic bone lesions |
|
Castleman disease |
|
|
Elevated serum Vascular Endothelial Growth Factor (VEGF) levels |
|
|
MINOR CRITERIA |
Papilledema |
|
Organomegaly (splenomegaly, lymphadenopathy etc.) |
|
|
Extravascular volume overload (pleural effusion, peripheral edema etc.) |
|
|
Skin changes |
|
|
Endocrinopathy (adrenal, thyroid, pituitary etc.) |
|
|
KNOWN ASSOCIATIONS |
Thrombocytosis |
Table 2: Hemodynamic parameters obtained during right heart catheterization before and after autologous stem cell transplant.
|
|
RHC BEFORE ASCT |
RHC AFTER ASCT |
|
RA PRESSURE (mm Hg) |
5 |
3 |
|
RV PRESSURE (mm Hg) |
73/6 |
45/5 |
|
PA PRESSURE (mm Hg) |
70/20 |
45/15 |
|
MEAN PA PRESSURE (mm Hg) |
42 |
27 |
|
PA WEDGE PRESSURE (mm Hg) |
8 |
8 |
|
PA PRESSURE AFTER NO (mm Hg) |
42/11 |
- |
|
MEAN PA PRESSURE AFTER NO (mm Hg) |
27 |
- |
|
PVR (woods units) |
7 |
3.8 |
|
CARDIAC OUTPUT (L/min) (FICK) |
4.9 |
5 |
|
CARDIAC INDEX (L/(min-m^2)) (FICK) |
2.84 |
2.95 |
RA: Right Atrium; RV: Right Ventricle; PA: Pulmonary Artery; PVR: Pulmonary Vascular Resistance; RHC: Right Heart Catheterization; ASCT: Autologous Stem Cell Transplant.
References
- Jian Li, Zhuang Tian, Hao Yi Zheng, Wei Zhang, Ming Hui Duan et al. (2013) Pulmonary hypertension in POEMS syndrome. Haematologica 98: 393-398. [Crossref]
- P Lesprit, B Godeau, F J Authier, M Soubrier, M Zuber et al. (1998) Pulmonary hypertension in POEMS syndrome: A new feature mediated by cytokines. Am J Respir Crit Care Med 157: 907-911. [Crossref]
- Toshikazu D Tanaka, Sonoko Misawa, Michihiro Yoshimura, Satoshi Kuwabara et al. (2018) Reversal of pulmonary arterial hypertension in POEMS syndrome with thalidomide: a case report. Eur Heart J Case Rep 2: yty051. [Crossref]
- Melanie J Brewis, Alistair C Church, Andrew J Peacock, Stephen Thomson, Jane Tighe et al. (2014) Pulmonary hypertension in POEMS syndrome: resolution following radiotherapy. Pulm Circ 4: 732-735. [Crossref]
- Chikako Ohwada, Emiko Sakaida, Chika Kawajiri Manako, Yuhei Nagao, Nagisa Oshima Hasegawa et al. (2018) Long-term evaluation of physical improvement and survival of autologous stem cell transplantation in POEMS syndrome. Blood 131: 2173-2176. [Crossref]
- Satish Chandrashekaran, Angela Dispenzieri, Stephen S Cha, Cassie C Kennedy (2015) Pulmonary Morbidity Improves After Autologous Stem Cell Transplantation in POEMS Syndrome. Respir Med 109: 122-130. [Crossref]
- Angela Dispenzieri (2014) POEMS syndrome: 2014 update on diagnosis, risk stratification and management. Am J Hematol 89: 214-223. [Crossref]
- H Niimi, K Arimura, M Jonosono, T Hashiguchi, M Kawabata et al. (2000) VEGF is causative for pulmonary hypertension in a patient with Crow-Fukase (POEMS) syndrome. Intern Med 39: 1101-1104. [Crossref]
- D S Helmersen, G T Ford, S M Viner, W R Auger (2000) POEMS syndrome: a clue to understanding primary pulmonary hypertension? A review of current insights into the pathogenesis of primary pulmonary hypertension. Can J Cardiol 16: 975-981. [Crossref]
- L Feinberg, D Temple, E de Marchena, R Patarca, A Mitrani (1999) Soluble immune mediators in POEMS syndrome with pulmonary hypertension: case report and review. Crit Rev Oncog 10: 293-302. [Crossref]
- Norbert F Voelkel, Jose Gomez Arroyo (2014) The role of vascular endothelial growth factor in pulmonary arterial hypertension. The angiogenesis paradox. Am J Respir Cell Mol Biol 51: 474-484. [Crossref]
- Watanabe, K Arimura, I Kitajima, M Osame, I Maruyama (1996) Greatly raised vascular endothelial growth factor (VEGF) in POEMS syndrome. Lancet 347: 702. [Crossref]
- Watanabe, I Maruyama, K Arimura, I Kitajima, H Arimura et al. (1998) Overproduction of vascular endothelial growth factor/vascular permeability factor is causative in Crow-Fukase (POEMS) syndrome. Muscle Nerve 21: 1390-1397. [Crossref]
- M Soubrier, C Sauron, B Souweine, C Larroche, B Wechsler et al. (1999) Growth factors and proinflammatory cytokines in the renal involvement of POEMS syndrome. Am J Kidney Dis 34: 633-638. [Crossref]
- Marina Scarlato, Stefano Carlo Previtali, Marinella Carpo, Davide Pareyson, Chiara Briani et al. (2005) Polyneuropathy in POEMS syndrome: Role of angiogenic factors in the pathogenesis. Brain 128: 1911-1920. [Crossref]
- Oddbjørn Straume, Jann Bergheim, Peter Ernst (2006) Bevacizumab therapy for POEMS syndrome. Blood 107: 4972-4973. [Crossref]
- AZ Badros, A Jaccard (2006) Bevacizumab therapy for POEMS syndrome. Blood 107: 4973-4974.
- Micah R Fisher, Paul R Forfia, Elzbieta Chamera, Traci Housten Harris, Hunter C Champion et al. (2009) Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med 179: 615-621. [Crossref]
- Jonathan D Rich, Sanjiv J Shah, Rajiv S Swamy, Anna Kamp, Stuart Rich (2011) Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension: implications for clinical practice. Chest 139: 988-993. [Crossref]
- C Wang, X F Huang, Q Q Cai, X X Cao, M H Duan et al. (2017) Prognostic study for overall survival in patients with newly diagnosed POEMS syndrome. Leukemia 31: 100-106. [Crossref]
- Anita D'Souza, Martha Lacy, Morie Gertz, Shaji Kumar, Francis Buadi et al. (2012) Long term outcomes after autologous stem cell transplantation for patients with POEMS syndrome (osteosclerotic myeloma): a single center experience. Blood 120: 56-62. [Crossref]
