Term Pregnancy in a Woman with Incomplete Transverse Vaginal Septum- An Interesting Case
Term Pregnancy in a Woman with Incomplete Transverse Vaginal Septum- An Interesting Case
A B S T R A C T
Transverse vaginal septum is a rare Mullerian duct anomaly presenting for the first time in pregnancy and labor. A 24-year-old primigravida presented at 39 weeks gestation. Speculum examination revealed a thick transverse vaginal septum with a pinpoint opening in the upper aspect. Elective cesarean section was done followed by digital perforation and dilatation of the septum. The postoperative period was uneventful. At six week follow up there was no restenosis or scarring of the vagina. To avoid complications like obstructed labor and laceration of vagina prophylactic cesarean section is advocated when the thickness of the septum cannot be ascertained on clinical examination.
Keywords
Transverse vaginal septum, Mullerian anomalies
Introduction
A transverse vaginal septum is an uncommon anomaly of the female genital tract and results from the incomplete vertical fusion of the Mullerian ducts and the urogenital sinus. It can be either complete or incomplete. Incomplete transverse septum can be asymptomatic and diagnosed for the first time in pregnancy [1].
Case Presentation
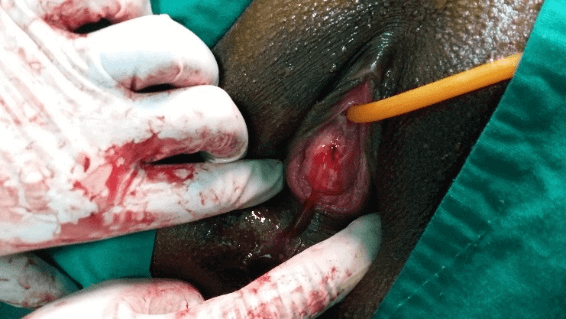
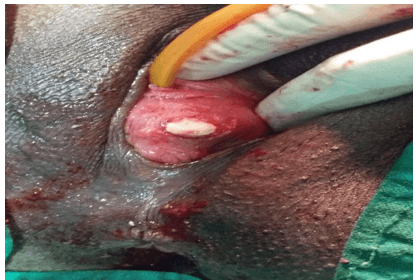
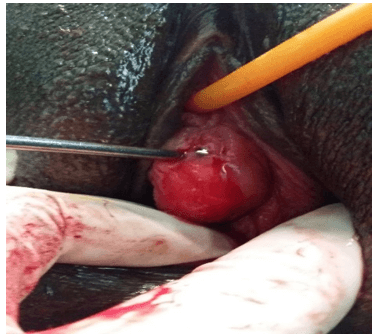
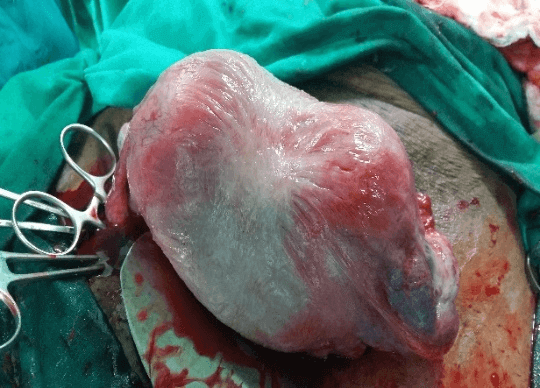
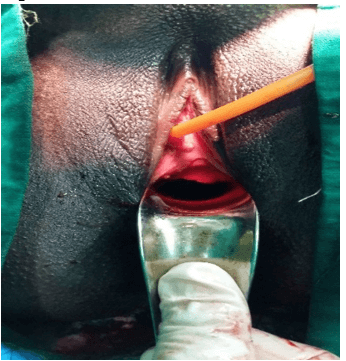
Our case was a 24-year-old Primigravida who presented at 39 weeks of gestation. Speculum examination revealed a thick transverse vaginal septum with a pinpoint opening in the upper aspect. There was no history of dyspareunia, dysmenorrhea, foul-smelling discharge, or infertility. The decision for elective cesarean section was taken. Intraoperatively the uterus was arcuate, and seepage of blood was visualized through the small vaginal opening (Figures 1 & 4). A finger was introduced into the cervix through the uterine incision onto the tiny opening in the transverse vaginal septum which was further dilated easily by blunt stretching probably because it was incomplete and normal anatomy was restored (Figures 2, 3 & 5). The postoperative period was uneventful. She was advised for regular intercourse to maintain the patency of the vagina. At six weeks follow up there was no restenosis or scarring of the vagina.
Figure 1: Low transverse vaginal septum with a central aperture through which blood escapes.
Figure 2: Finger inserted into the aperture of septum from above through cervix.
Figure 3: Dilator inserted through the aperture in the septum from vaginal side.
Figure 4: Arcuate uterus associated with incomplete vaginal septum.
Figure 5: Postoperative vagina with no residual septum left.
Discussion
Transverse vaginal septum is a disorder of vertical fusion of uterovaginal anomalies which was first described by Delaunay in 1877. The incidence ranges from 1:2100 to 84000 [2, 3]. It belongs to class II of AFS (American Fertility Society) classification, V3 subgroup of ESHRE (European Society of Human Reproduction and Embryology)/ ESGE (European Society for Gynecological Endoscopy) consensus [4]. The etiology is unknown but, in a few cases, female sex-limited autosomal recessive transmission is noted. There are two theories proposed regarding the formation of transverse vaginal septum. First, the failure in the fusion of caudal end of the Mullerian duct and sinovaginal bulb of the urogenital sinus. Second, failure of canalization of the formed vaginal plate which occurs around 5 months of gestation. It is a fibrous membrane of connective tissue containing vascular and muscular elements lined by stratified squamous epithelium on either side.
The septum can be found at any level, but most commonly at the level of the upper and middle third of the vagina [2]. The septum can be classified based upon its distance from introitus, its thickness, and whether it is perforated or not [2, 3]. Depending upon the distance from introitus, the septum can be classified as low (<3 cm), mid (3-6 cm), or high (>6 cm) and the percentage of their occurrence are 46%, 35%, and 19% respectively [5]. The septum can be thick (>1 cm) or thin (<1 cm) of which thin is more common. The closer the cervix, the thicker is the septum. The septum can be complete (imperforate) or incomplete (perforate). The higher the septum, more likely to be incomplete and vice versa. The complete septum presents usually around menarche with primary amenorrhoea, cyclic abdominal pain, abdominal or pelvic mass (hematometra, hematocolpos, hematosalpinx) [2]. Rarely, it presents before puberty as mucocolpos [6]. In cases of the incomplete septum, menstrual blood escapes through the opening and hence they are predominantly asymptomatic. Occasionally, a patient with infertility can present with prolonged menstrual bleeding, dysmenorrhea, dyspareunia, and foul-smelling vaginal discharge which are found incidentally during routine gynecological examination.
Family history and pelvic examination are important for diagnosis. But, if the patient presents in labor, the incomplete septum is falsely considered to be an undilated external os. Ultrasonography is the key tool used for initial diagnosis to demonstrate the features of obstruction, presence of endometriosis, and other uterine and genitourinary anomalies. MRI is the standard technique used for diagnosing uterovaginal anomalies and also used for assessing location and thickness of septum and complete delineation of complex genital tract anomalies. Often, the transverse septum is associated with genitourinary, gastrointestinal tract, renal and cardiac defects. Bicornuate uterus, septate uterus, bilateral tubal atresia are less commonly associated and association with arcuate uterus has not been documented yet. The differential diagnosis for transverse vaginal septum includes imperforate hymen, vaginal atresia, vaginal aplasia, absent cervix.
Septum needs to be corrected surgically. Although case reports showing success with vaginal dilators are documented, it should be used preoperatively to improve outcomes and postoperatively to prevent strictures. The outcomes expected from surgery are egress of menstrual blood without obstruction and to obtain functional vaginal length. The low, thin and perforate septum can be dealt with transvaginal resection followed by end-to-end anastomosis. While thick, upper and mid vaginal septum can be approached through the abdomino-vaginal method, Z-plasty, push through, and pull through method, using olbert balloon catheter and hysteroscopic resection. Postop complications such as vaginal stenosis and re-obstruction are more common with thick septa which can be prevented with the use of dilators or mold postoperatively until intercourse resumes [3]. Pregnancies have been reported following the excision of the septum with a live birth rate of nearly 94% [7].
In the case of incomplete septum, some may present in labor or pregnancy as in our case scenario. There are three options available. First, expectant management allowing spontaneous dissection of septum or incision late in labor, if septum is thin [8]. Untreated transverse vaginal septum has a risk of significant vaginal lacerations during vaginal delivery or can result in obstructed labor which can further result in rupture uterus. Hence this entity if corrected early, can avoid future complications. Strict vigilance is required while following expectant management. Blanton et al. reported 2 patients with transverse vaginal septa who were allowed trial of labour followed by incision of septum in active labour, resulting in vaginal delivery without complications [1]. Second, incision of the septum before labor with a risk of excess bleeding and restenosis. Third, if the septum is high or thick or cannot be assessed in labor, elective cesarean section is advisable [9].
Conclusion
Spontaneous conception and an uneventful antenatal period have been reported in the literature in women with incomplete transverse vaginal septum. Cesarean section is usually preferred for patients who are diagnosed with transverse vaginal septum diagnosed during pregnancy and labor. Yet, with strict monitoring trial of labor can be tried in a few cases.
Article Info
Article Type
Case ReportPublication history
Received: Fri 17, Jul 2020Accepted: Mon 03, Aug 2020
Published: Mon 17, Aug 2020
Copyright
© 2023 sathiya priya subburaj. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.08.15
Author Info
sathiya priya subburaj Jyotsna sharma HARITHA SAGILI
Corresponding Author
sathiya priya subburajDepartment of Obstetrics & Gynaecology, JIPMER, Puducherry, India
Figures & Tables
References
- Elizabeth N Blanton, Dwight J Rouse (2003) Trial of labor in women with transverse vaginal septa. Obstet Gynecol 101: 1110-1112. [Crossref]
- C E Williams, R S Nakhal, M A Hall Craggs, D Wood, A Cutner et al. (2014) Transverse vaginal septae: management and long-term outcomes. BJOG 121: 1653-1658. [Crossref]
- N Arkoulis, C Kearns, M Deeny, Jrc Telfer (2017) The interdigitating Y-plasty procedure for the correction of transverse vaginal septa. BJOG 124: 331-335. [Crossref]
- Grigoris F Grimbizis, Stephan Gordts, Attilio Di Spiezio Sardo, Sara Brucker, Carlo De Angelis et al. (2013) The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod 28: 2032-2044. [Crossref]
- J A Rock, H A Zacur, A M Dlugi, H W Jones Jr, R W TeLinde (1982) Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet Gynecol 59: 448-451. [Crossref]
- S Ahmed, L L Morris, E Atkinson (1999) Distal mucocolpos and proximal hematocolpos secondary to concurrent imperforate hymen and transverse vaginal septum. J Pediatr Surg 34: 1555-1556. [Crossref]
- F Raga, C Bauset, J Remohi, F Bonilla Musoles, C Simón et al. (1997) Reproductive impact of congenital Müllerian anomalies. Hum Reprod 12: 2277-2281. [Crossref]
- Yusuf Üstün, Yaprak Engin Üstün, Þahin Zeteroðlu, Güler Þahin, Mansur Kamacý (2005) A Case of Transverse Vaginal Septum Diagnosed During Labor. Erciyes Medical Journal 27: 136-138.
- Vani Malhotra, Vandana Bhuria, Smiti Nanda, Meenakshi Barsaul Chauhan, Pushpa Dahiya (2013) Transverse Vaginal Septum in Labor. J Gynecol Surg 29: 207-209.
