Successful Treatment of Prepouch Ileitis with Oral Mesalamine in Barnett Continent Ileal Reservoir
A B S T R A C T
Barnett Continent Ileal Reservoir is rarely performed in patients with ulcerative colitis who require colectomy. Prepouch ileitis occasionally occurs in patients with ileal pouches. The role of oral mesalamine in the treatment of prepouch ileitis has not been established. We describe a case in which prepouch ileitis in Barnett Continent Ileal Reservoir was successfully treated with oral mesalamine. This is the first case in the literature showing that mesalamine is safe and effective in the treatment of prepouch ileitis in a patient with a continent ileostomy.
Keywords
Barnett continent ileal reservoir, continent ileostomy, ileal pouch-anal anastomosis, mesalamine, treatment, prepouch ileitis
Introduction
Colectomy is needed when ulcerative colitis (UC) is refractory to medical therapy or colitis-associated neoplasia is developed. Following total proctocolectomy, most patients elect to have ileal pouch-anal anastomosis (IPAA). However, IPAA may not be feasible in some of the patients with conditions such as weak anal sphincter muscles. In these cases, continent ileostomy is a valid option. The two common types of continent ileostomies are a K-pouch or a Barnett Continent Ileostomy Reservoir (BCIR). Pouchitis is the most common long-term complication after IPAA [1]. Some of the patients may also have concurrent prepouch ileitis (PPI) [2, 3]. Antibiotics, budesonide, and biological agents are the main treatment options. The role of oral mesalamine in the treatment of pouchitis or PPI is not clear. There are scant data in the management of pouchitis and PPI in patients with BCIR. Here we report a case in which PPI in BCIR was successfully treated with oral mesalamine.
Case Report
A 65-year-old male patient with a BCIR presented with abdominal pain, liquid bowel movement, and difficulty with intubation. The patient had an IPAA created for UC, which was complicated by refractory cuffitis resulting in pouch failure. Twelve years later, the IPAA was surgically converted to a BCIR. The patient was a former smoker with a history of anxiety, gastroesophageal reflux disease, sleep apnea, and type 2 diabetes mellitus. He had a family history of ulcerative colitis and Crohn’s disease. His medications at presentation included atorvastatin, diazepam, famotidine, insulin, and sodium bicarbonate. Laboratory evaluation showed no gastrointestinal pathogens.
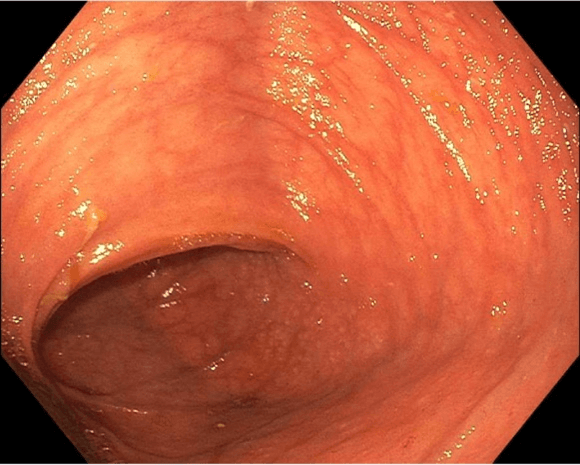
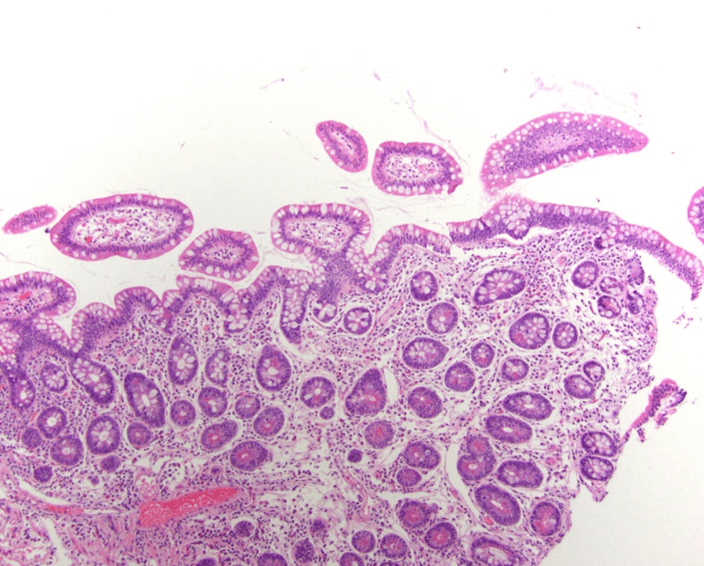
A pouchoscopy (Figure 1) was performed which showed the BCIR with an intact but slightly loose valve. The mucosa of the pouch body appeared normal. The inlet of the pouch was ulcerated, but not angulated or strictured. There was a long segment (35cm) of PPI with edema, erythema, ulcers and was circumferentially distributed. PPI with a pattern of Crohn’s disease was considered. Histologic evaluation of the afferent limb showed moderate to severe active chronic pouchitis with villous atrophy (Figure 2). The patient was started on oral mesalamine, 4.8gram/day. A follow-up pouchoscopy (Figure 3) performed 6 weeks later showed normal pouch mucosa and stable ulcers at the inlet. However, inflammation and ulcers at the long segment of the afferent limb completely resolved. Repeat histologic evaluation of the prepouch ileum showed only minimal active inflammation (Figure 4). The patient’s symptoms were completely resolved at 6- and 10-week follow-ups.
Figure 1: Inflammation and ulcers in the prepouch ileum ulcerated pouch inlet, image from in the index first pouchoscopy.
Figure 2: Pre-treatment histologic evaluation of the afferent limb showed acute and chronic inflammatory changes characterized by diffuse neutrophilic infiltrates, erosion, villous atrophy, and full thickness lamina propria lymphoplasmacytic cell infiltrate.
Figure 3: Endoscopic resolution of inflammation in the afferent limb after treatment.
Figure 4: Post-treatment histologic evaluation of the afferent limb biopsy showed mild residual active inflammation with resolution of the chronic inflammatory infiltrates and restoration of villous architecture.
Discussion
Pouchitis and PPI can occur in patients with ileal pouches including in BCIR. Acute pouchitis is traditionally treated with antibiotics, while chronic pouchitis often requires non-antibiotic regimens, such as budesonide or biological agents. PPI can be an extension of diffuse pouchitis or represents a Crohn’s disease-like condition. Acute or chronic PPI is often more difficult to treat than pouchitis. Often, PPI is treated with biological agents [4, 5]. The role of oral mesalamine in the treatment of pouchitis or PPI is not clear, although small case series demonstrated some efficacy in chronic antibiotic-refractory pouchitis [6]. Mesalamine has been described for the treatment of chronic antibiotic-refractory pouchitis because of its high safety profile [6]. However, to date, the use of oral mesalamine in the treatment of PPI or in the treatment of inflammatory conditions in the continent ileostomy has not been described.
This case report reviews the treatment of prepouch ileitis in BCIR using oral mesalamine. After 6 weeks between the original pouchoscopy and the follow-up pouchoscopy, there was complete resolution of inflammation and ulceration of the prepouch afferent limb on endoscopy and histology, along with the resolution of symptoms. We decided to continue oral mesalamine as long-term maintenance therapy.
Conflicts of Interest
Honoraria: Bo Shen, Abbvie, Janssen, Takeda; Advisory Fees/Rewards: Bo Shen, Abbvie, Janssen, Takeda; Aditya Pokala and Mabel H. Ko: None.
Abbreviation
BCIR: Barnett Continent Ileal Reservoir
IPAA: Ileal Pouch-Anal Anastomosis
PPI: Prepouch Ileitis
UC: Ulcerative Colitis
Article Info
Article Type
Case ReportPublication history
Received: Mon 05, Jul 2021Accepted: Mon 19, Jul 2021
Published: Tue 03, Aug 2021
Copyright
© 2023 Bo Shen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.08.02
Author Info
Aditya Vishnu Pokala Mabel Huai Bin Ko Bo Shen
Corresponding Author
Bo ShenCenter for Inflammatory Bowel Diseases and Division of Colorectal Surgery and Department of Pathology, Columbia University Irving Medical Center/New York-Presbyterian Hospital, New York, USA
Figures & Tables


References
1. Fazio VW, Kiran RP,
Remzi FH, Coffey JC, Heneghan HM et al. (2013) Ileal pouch anal anastomosis:
analysis of outcome and quality of life in 3707 patients. Ann Surg 257:
679-685. [Crossref]
2. Segal JP,
McLaughlin SD, Faiz OD, Hart AL, Clark SK (2018) Incidence and Long-term
Implications of Prepouch Ileitis: An Observational Study. Dis Colon Rectum
61: 472-475. [Crossref]
3. Samaan MA, de Jong
D, Sahami S, Morgan S, Fragkos K et al. (2016) Incidence and Severity of
Prepouch Ileitis: A distinct disease entity or a manifestation of refractory pouchitis?
Inflamm Bowel Dis 22: 662-668. [Crossref]
4.
Segal JP, Rottoli M, Felwick RK,
Worley GH, McLaughlin SD et al. (2018) Biological therapy for the treatment of
prepouch ileitis: a retrospective observational study from three centers. Clin
Exp Gastroenterol 11: 461-465. [Crossref]
5. Syal G, Shemtov R, Bonthala N, Vasiliauskas EA, Feldman EJ et al. (2021) Pre-pouch ileitis is associated with development of Crohn's disease-like complications and pouch failure. J Crohns Colitis 15: 960-968. [Crossref]
6. Shen B, Fazio VW, Remzi FH, Bennett AE, Lopez R et al. (2007) Combined ciprofloxacin and tinidazole therapy in the treatment of chronic refractory pouchitis. Dis Colon Rectum 50: 498-508. [Crossref]
