Study on Regulatory Effects of Yam Rice Powder (YRP) and its Ethanol Extract on Blood Sugar and Lipids and Reducing Oxidative Stress of Diabetic Mice/Patient
A B S T R A C T
In the present study, we evaluated the hypoglycemic, hypolipidemic and anti-peroxidative effects of yam rice powder (YRP) derived from Tremella aurantialba on streptozotocin (STZ)-induced diabetic mice and diabetic patients. Diabetic mice were treated with ethanol extract of YRP (EEYR) at three doses or YRP for 30 days. Diabetic patients were treated with ethanol extract solution of YRP (ESYR) for 4.5 months. Results indicated that EEYR administration significantly reduced levels of fasting blood glucose (FBG), serum fructosamine, total cholesterol, total triglyceride and malondialdehyde, and increased glucose metabolism velocities and superoxide dismutase level in the serum compared with diabetic controls (p<0.01). Moreover, ESYR could replace chemical drugs to control the FBG and postprandial blood glucose levels of diabetic patients. Our results suggested that YRP could enhance hypoglycemic, hypolipidemic and antioxidant properties in STZ-induced diabetic mice and diabetic patients. Collectively, YRP might be used as food to prevent or manage diabetes.
Keywords
Diabetes, yam rice powder, fasting blood glucose, glucose metabolism velocity, hypoglycermic effect
Introduction
Yam rice powder (YRP) is prepared by solid-state fermentation of Tremella aurantialba using Chinese yam, rice and corn bran as feedstock. YRP contains biomedicine components, such as polysaccharides and saponins. T. aurantialba, a medical fungus, belongs to the so-called “jelly mushrooms” group that forms a gelatinous fruiting body. It has been proved that T. aurantiable is not poisonous, and it is used as food and medical drugs for thousands of years in many Asian countries due to its beneficial properties as follows, including immuno-enhancing, anti-tumor, anti-hypoglycemic and anti-diabetic activities [1-5]. In our previous research, the extract from T. aurantialba broth (TBE, its main component is saponin) can regulate plasma glucose of type 2 diabetes in rats [6]. Furthermore, we have found that TBE and T. aurantialba mycelium polysaccharides (TMP) can reduce the blood glucose level (BGL) of the alloxan-induced diabetic mellitus rats, while TBE possesses stronger abilities to decrease the levels of total cholesterol (TC) and triglyceride (TG) in serum and enhance antioxidant capability [7].
Chinese yam is the leading form of food staple for millions of people in tropical and subtropical countries. It is a tuber of Dioscorea polygonoides. In China, the cultivation of yam has a long history for both edible and medical purposes. Yam is not only a common food regarded as a tonic but also has been used for more than 2,000 years in traditional Chinese medicine for the treatment of diabetes, diarrhoea, asthma and other ailments (Chinese Pharmacopoeia, 2005 edition). Saponins or sapogenins, namely diosgenins, have been reported to be the active components of many yam species [8]. There are several reports showing the hypoglycemic effect of diosgenin in normal and diseased states [9-11]. In the present study, we investigated the anti-diabetic effects of YRP and its ethanol extract. Our findings provided valuable insights into the mechanism underlying the anti-diabetic effects of YRP.
Materials and Methods
I Chemicals and Raw Materials
YRP was kindly gifted by Zhenjiang Yemaikang Food-Biological Sci-Technology Co., Ltd. and kept at room temperature under dry conditions. Streptozotocin (STZ) was purchased from Sigma-Aldrich (Shanghai, China). The diagnostic kits for fructosamine, TC, TG, superoxide dismutase (SOD) and malondialdehyde (MDA) were obtained from Rongsheng Biotechnology Co., Ltd. (Shanghai, China). The insulin determination kits were supplied by Shanghai Juchuang Medical-Tech Co., Ltd. (Shanghai, China).
II Animals
ICR mice, weighing 17.12 ± 1.51 g, were purchased from the Central Animal House, China Pharmaceutical University (Nanjing, China). The animals were housed in the steel cages at an ambient temperature of 22±2 °C in a photoperiod-controlled room (light/dark 12/12 h) with a relative humidity of 45% to 55%. The animals were fed on a normal commercial chow diet consisting of 4.5% corn oil, 23% casein, 31.9% corn starch, 30.4% sucrose, 5.3% cellulose, 1.2% vitamin complex and 3.7% mineral mixture. Water was freely available. This animal experiment was approved by Institutional Animal Care and Use Committee, Jiangsu University (ID: UJS-IACUC-2018051601). All animal-related operations were conducted in conformity with the institutional guidelines of the School of Medicine, Jiangsu University, China.
III Extract of YRP
Briefly, 500 g YRP was soaked in 6 L 50% ethanol in a 50-L stainless steel extractor tank for 24 h with continuous stirring at 150 rpm. Subsequently, the mixture was filtered with Whatman No. 1 filter paper. The filtrate was then centrifuged at 5,000 rpm at 20 °C. The supernatant was collected and concentrated under reduced pressure with a rotary evaporator to yield ethanol extract of YRP (EEYR).
IV Ethanol Solution of YRP
Briefly, 25 Kg YRP was soaked in 300 L 50% ethanol in a 500-L stainless steel extractor tank for 24 h with continuous stirring at 150 rpm. Subsequently, the mixture was filtered with Whatman No. 1 filter paper. The filtrate was centrifuged at 4,000 rpm at 20°C. The supernatant was collected and concentrated to 50 L to remove ethanol under reduced pressure. The concentrated liquid was set to 250 L and named as ethanol extract solution of YRP (ESYR). ESYR was sub-packaged into 450-mL food-grade plastic bottles at 400 mL per bottle and then autoclaved at 80°C for 80 min.
V Preparation of Animal Diet Containing YRP (ADYP)
The ADYP was composed of 98.3% normal commercial chow diet and 1.7% YRP. Additionally, 5% water was added to ADYP to prepare the chow diet. The diet was dried at 60 °C and then ADYP was sterilized by cobalt 60 irradiation at a dose of 35 kGy.
VI Induction of Diabetes in Experimental Animals
Mice were intraperitoneally injected with a freshly prepared solution of STZ in 0.1 mol/L citrate buffer (pH = 4.5) kept on ice at a dose of 160 mg/kg body weight (bw). Since STZ injection can provoke fatal hypoglycemia as a result of the massive reactive release of pancreatic insulin, mice were also orally given 5 mL/kg bw of a 20% glucose solution after 6 h. After 8 days, fasting blood was drawn from the tail vein, followed by the determination of fasting blood glucose (FBG) levels. The mice with FBG levels exceeding 11 mmol/L were considered diabetic mice and selected for further study. All mice were not treated with insulin in this study.
VII Experimental Design
A total of 70 mice (10 normal mice and 60 STZ-induced diabetic mice) were evenly divided into seven groups. In the blank control group (BC), untreated mice were fed on a normal commercial chow diet and intragastrically administered an equivalent volume of 1% carboxylcellulose solution as blank control. In the negative control group (NC), STZ-induced diabetic mice were fed on a normal commercial chow diet and intragastrically administered an equivalent volume of 1% carboxylcellulose solution as the negative control. In the positive control group (PC), STZ-induced diabetic mice were fed on a normal commercial chow diet and intragastrically administered metformin at a dose of 150 mg/kg bw as the positive control. In the low-dose group (EEYR-LD), STZ-induced diabetic mice were fed on a normal commercial chow diet and intragastrically administered 7 mg/kg bw EEYR. In the middle-dose group (EEYR-MD), STZ-induced diabetic mice were fed on a normal commercial chow diet and intragastrically administered 14 mg/kg bw EEYR. In the high-dose group (EEYR-HD), STZ-induced diabetic mice were fed on a normal commercial chow diet and intragastrically administered 28 mg/kg bw EEYR.
In the YRP group (YRP), STZ-induced diabetic mice were fed on a diet containing YRP and intragastrically administered an equivalent volume of 1% carboxylcellulose solution. EEYR was dissolved in 1% carboxylcellulose. All tested animals were administered once every day for 30 consecutive days. At the end of the experimental period, the mice were anaesthetised with ketamine following a 12-h food deprivation, and blood samples were drawn from the orbital sinus. The blood was collected in a heparin-coated tube and centrifuged at 4,000×g for 15 min at 4°C to obtain serum samples. These serum samples were stored at -70°C prior to the determination of insulin, fructosamine, TG, TC and MDA levels, as well as SOD activities.
VIII Effect of FBG Level
After mice fasted for 6 h, FBG levels were determined using a blood glucose meter (ACCU-Check blood glucose meter, Roche Diagnostics, Shanghai, China) before grouping and on 10th, 20th and 30th day.
IX Oral Glucose Tolerance Test (OGTT)
After 12-h fasting on the day of animal sacrifice, FBG levels of all mice were determined using a blood glucose meter. Glucose (2 g/kg) was orally administered, and BGLs were monitored using a blood glucose meter at 0, 30, 60 and 120 min.
X Analytical Methods
The polysaccharide and saponin contents of YRP, EEYR and ESYR were determined by the colorimetric method [12, 13]. The insulin, fructosamine, TC, TG, SOD and MDA levels in the serum of diabetic mice were determined using their corresponding colorimetric assay kits according to the manufacturer’s instructions.
XI Hypoglycemic Effect of ESYR on Diabetic Patients
The study was approved by Henan Medical Ethics Committee and conducted in the Songxian People's Hospital of Henan Province, China. A total of 100 volunteer diabetic patients, including 21 females and 79 males, were selected as research subjects. The average age of these patients was 53.5 years, and the average diabetes time was 6.2 years. All diabetic patients were orally administered some hypoglycemic drugs before clinical trials. The experimental time was 6.5 months, of which the YRP administration period was 4.5 months and the observation period was 2 months. When all patients took ESYR, the hypoglycermic drugs were administered at the half dose during the first 15 days and were completely stopped in the following 4 months. All patients took ESYR on an empty stomach in the morning at a dose of 80 mL per day. The determination indices were FBG and postprandial blood glucose (PBG) at regular intervals during the trial period.
Results and Discussion
I Biomedical Component Analysis of YRP, EEYR and ESYR
EEYR and ESYR were extracted from YPR with 50% ethanol. Regression equation of polysaccharide analysis was as follows: C = 1.399A+0.003, R2 = 0.998. C is the polysaccharide concentration, and A is the absorbance. R2 (0.998) showed that there was a better linear correlation between 0.1 and 0.8 mg/mL polysaccharide concentration. Quantitative analysis indicated that the contents of YRP, EEYR and ESYR were up to 6.164 mg/g, 78.3 mg/g and 6.34 mg/mL, respectively. Regression equation of saponin analysis using ginsenoside R1 as standard reagent was as follows: C = 3.0695A+0.0107, R2 = 0.994. C is the saponin concentration, and A is the absorbance. R2 (0.994) showed that there was a better linear correlation between 0.1 and 0.5 mg/mL of ginsenoside R1 concentration. Quantitative analysis indicated that the contents of YRP, EEYR and ESYR were up to 0.842 mg/g, 25.6 mg/g and 2.57 mg/mL, respectively. In view of the high contents of polysaccharides and saponins of YRP, we studied the possibility of using YRP as a hypoglycermic food.
II Effect of EEYR and YRP on the BW
STZ-induced diabetic mice showed a significant decrease in bw during the 30-day period (NC group) compared with the BC group (p<0.01). In contrast, the bw of diabetic mice treated with metformin, EEYR or YRP for 30 days was significantly increased compared with the NC group (Table 1, p<0.01). The significant reduction in total bw of animals could be attributed to the lipid consumption of adipose tissue and the destructive metabolism of amino acids in muscle tissue.
Table 1: Effect of YRP on the body weight of diabetic mice (g).
|
Group |
0 |
10d |
20d |
30d |
|
BC |
18.98±2.63 |
20.66±2.50 |
23.02±2.57 |
24.84±1.90 |
|
NC |
18.56±2.74 |
18.80±2.25 |
18.88±1.65** |
19.08±1.78** |
|
PC |
18.88±2.81 |
20.29±2.45 |
21.53±2.48## |
23.12±2.59## |
|
EEYR-LD |
18.76±2.85 |
19.77±3.06 |
20.63±3.11 |
21.57±3.16** |
|
EEYR-MD |
18.67±2.70 |
19.88±2.79 |
21.06±2.67 |
22.02±2.53**## |
|
EEYR-HD |
18.77±2.98 |
20.49±3.02 |
22.32±2.86## |
23.52±2.10## |
|
YRP |
18.79±2.97 |
19.56±2.70 |
20.67±2.52 |
22.54±2.29**## |
a Values are expressed as
means ± SD (n = 10); * As compared with BC group: p<0.05, ** As compared
with BC group: p<0.01; # As compared with NC group: p<0.05, ##
As compared with NC group: p<0.01.
III Effect of EEYR and YRP on the FBL and Blood Fructosamine in Diabetic Mice
An abnormal increase of FBG is the key index for the identification of diabetes. Therefore, lowering the FBG of diabetic patients can decrease their complications [14]. The conventional therapies for diabetes have many shortcomings, such as side effects and a high rate of secondary failure. Dietary treatment of diabetes is characterized by safety and non-toxic side effects, and it has received extensive attention in recent years. Table 2 presents the FBG trends of mice in all groups over 30 days. Compared with the BC group (normal control mice), STZ-induced diabetic mice (all experimental groups) exhibited significantly increased FBG levels (p< 0.01) after 8 days of STZ injection. Before administration, no difference in FBG levels among all experimental groups was observed. During the entire administration period, the FBG levels of the two groups (BC and NC) were not significantly changed (p>0.05). After 20 days of administration, the FBG levels of EEYR-MG, EEYR-HG, PC and YRP groups were significantly decreased compared with the NG group. After continuous treatment for 30 days, the FBG levels of PC, EEYR-LG, EEYR-MG, EEYR-HG and YRP groups were significantly decreased (p<0.01) from 20.33 to 15.82 mmol/L, from 20.38 to 18.30 mmol/L, from 20.34 to 17.00 mmol/L, from 20.39 to 14.79 mmol/L and from 20.34 to 15.49 mmol/L, respectively. Obviously, the EEYR showed hypoglycemic effects in a dose-dependent manner.
Table 2: Effect of EEYR and YRP on the blood sugar levels of diabetic
mice (mmol/L).
|
Group |
0 |
10d |
20d |
30d |
|
BC |
6.12±0.25 |
6.18±0.21 |
6.24±0.19 |
6.27±0.11 |
|
NC |
20.31±2.70** |
20.63±2.59** |
21.01±2.83** |
21.20±2.93** |
|
PC |
20.33±2.67** |
18.46±2.65** |
17.11±2.86**## |
15.82±3.08**## |
|
EEYR-LD |
20.38±2.64** |
20.18±2.76** |
19.23±2.70** |
18.30±2.87**## |
|
EEYR-MD |
20.34±2.68** |
19.46±2.63** |
18.02±2.50**# |
17.00±3.44**## |
|
EEYR-HD |
20.39±2.65** |
18.00±2.68** |
16.46±3.38**## |
14.79±2.56**## |
|
YRP |
20.34±2.61** |
18.51±3.34** |
16.98±3.05**## |
15.49±3.05**## |
a Values are expressed as means ± SD (n = 10); *
As compared with BC group: p<0.05, ** As compared with BC group: p<0.01; #
As compared with NC group: p<0.05, ## As compared with NC group:
p<0.01.
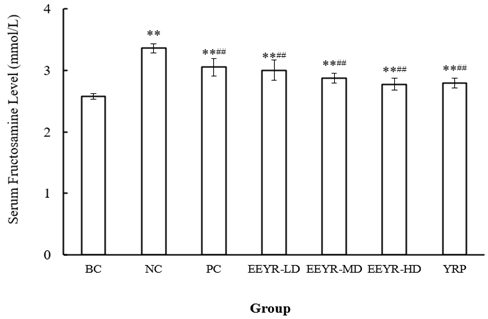
The fructosamine is the non-enzyme glycation product of serum protein. The higher BGLs, the higher blood fructosamine levels. The serum fructosamine level is an effective indicator for blood glucose level in the past 1-3 weeks from the time point of analysis. After administration for 30 days, the serum fructosamine levels of the NC group (3.362±0.073 mmol/L) were significantly higher than those of the BC group (2.579±0.030 mmol/L) (p<0.01) (Figure 1). The serum fructosamine levels of all EEYR groups and the YPR group were lower than those of the NC group (p<0.01). The results further proved that EEYR and YRP possessed hypoglycemic effects.
Figure 1: Effect of EEYR and YRP on serum fructosamine levels in STZ-induced diabetic mice.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p< 0.01. Compared with NC group, # p<0.05, ## p<0.01.
IV Effect of EEYR and YRP on the OGTT and Serum Insulin Levels
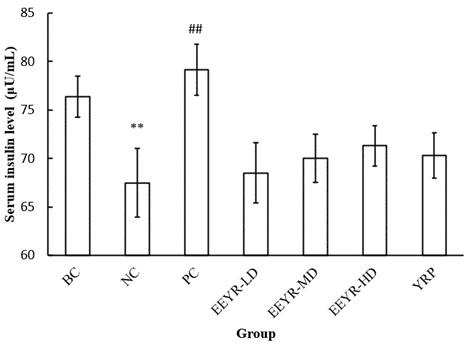
OGTT was performed to evaluate the effects of EEYR and YRP on insulin secretion in mice and blood glucose metabolism velocity, and serum insulin levels were determined. After 2 h of oral glucose administration (2 g/kg), the higher the BGL, the slower the blood glucose metabolism velocity. The slower blood glucose metabolism velocity indicated that the glucose tolerance level was decreased. Table 3 shows that the BGLs of all experimental groups reached the peak values, and no significant differences between experimental groups were found after 0.5 h of oral glucose administration. However, after 2 h of oral glucose administration, the BGLs of PC, EEYR-HG and YRP groups were significantly decreased compared with the NC group (Table 3). Therefore, EEYR-HG and YRP could rapidly reduce serum glucose concentration and improve the glucose tolerance and glucose metabolism velocity of diabetic mice. The analysis of serum insulin levels (Figure 2) displayed that the serum insulin level of the NC group (67.49±3.53 μU/mL) was obviously lower than that of the BC group (76.39±2.13 μU/mL) (p<0.01).
Table 3: Effect of YRP on the glucose tolerance tests of diabetic mice
(mmol/L).
|
Group |
0 |
30 min |
60 min |
120 min |
|
BC |
6.27±0.11 |
8.58±0.44 |
7.38±0.33 |
6.35±0.20 |
|
NC |
21.20±1.93 |
28.81±1.76 |
27.41±1.30 |
26.05±2.16 |
|
PC |
15.82±1.08 |
29.46±2.37 |
26.07±2.30 |
22.23±2.46## |
|
LD |
18.30±1.87 |
30.24±2.91 |
28.18±2.48 |
26.24±2.86 |
|
MD |
17.00±1.44 |
30.41±3.10 |
28.26±2.73 |
25.39±2.60 |
|
HD |
14.79±1.56 |
27.92±3.11 |
25.21±2.20 |
21.86±2.58## |
|
YRP |
15.49±1.05 |
28.68±2.41 |
24.82±2.12 |
21.44±2.47## |
a Values are expressed as means ± SD (n = 10); *
As compared with BC group: p<0.05, ** As compared with BC group: p<0.01; #
As compared with NC group: p<0.05, ## As compared with NC group:
p<0.01.
Figure 2: Effect of EEYR and YRP on serum insulin levels in STZ-induced diabetic mice.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p< 0.05, ## p<0.01.
The result could be explained by that the STZ injection selectively destroyed β-cells in the pancreatic islets and further inhibited insulin secretion by the pancreas. After administration, the serum insulin level of the PC group (79.17±2.62 μU/mL) was significantly higher than that of the NC group, while the serum insulin level of EEYR-LD, EEYR-MD, EEYR-HD and YRP groups was not significantly increased (Figure 2). These results were consistent with our previous findings [15]. Similar results have also been reported earlier by T. aurantialba broth in vivo [16]. The decrease of serum glucose concentration depends on serum insulin levels and glucose metabolism velocity. In view of no significant increase in serum insulin levels after administration of EEYR and YRP, we deduced that EEYR and YRP decreased the FBG levels by increasing glucose metabolism velocity instead of increasing serum insulin levels.
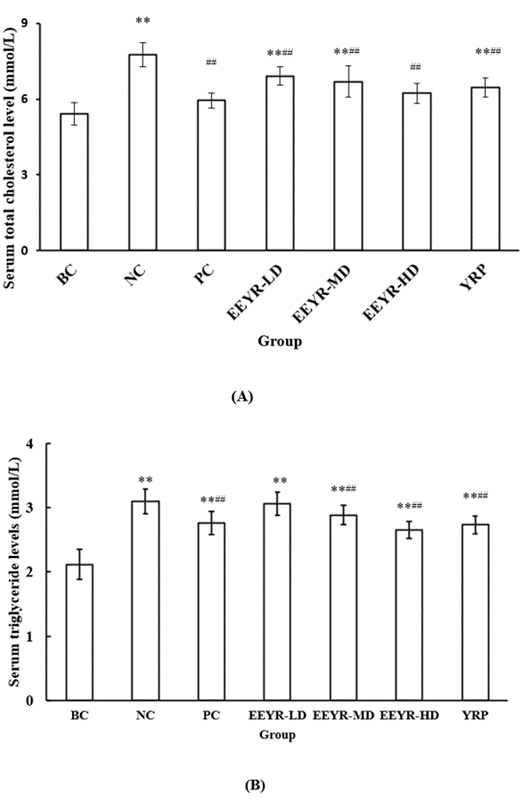
V Effect of EEYR and YRP on the Lipid Metabolism
Under diabetic conditions, abnormal lipid metabolism always leads to the increase of plasma TC, TG, low-density lipoprotein cholesterol (LDL-C) and very-low-density lipoprotein cholesterol (VLDL-C) levels and a decrease of high-density lipoprotein cholesterol (HDL-C) level. Over-high levels of TC, TG, LDL-C and VLDL-C are considered as key risk factors for cardiovascular diseases, such as coronary disease and atherosclerosis [17-21]. However, HDL-C plays a key role in reducing the risk of cardiovascular disease [22, 23]. Figures 3A & 3B present that STZ injection markedly elevated the levels of plasma lipids, including TC and TG, from 5.418±0.454 mmol/L and 2.118±0.231 mmol/L of the BC group to 7.765±0.460 mmol/L and 3.1±0.195 mmol/L of the NC group, respectively (p<0.01). However, the levels of plasma TG and TC were significantly reduced in diabetic mice administered with low, middle and high doses of EEYR and YRP (p<0.01). This finding indicated that treatment of EEYR and YRP for 30 days markedly decreased the serum TC and TG levels in diabetic mice, suggesting that YRP had a beneficial effect on dyslipidemia. Our previous investigation has supported the present result. In the previous study, TBE and TMP can reduce the serum TC and TG levels of alloxan-induced diabetic mice [7]. Therefore, the reduction of FBG levels and serum lipid levels in the EEYR and YRP groups revealed the hypoglycemic and hypolipidemic activities of YRP.
Figure 3: Effect of EEYR and YRP on serum A) TC and B) TG levels in STZ-induced diabetic mice.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.
The administration of EEYR and YRP significantly decreased serum TG and TC in diabetic mice. Moreover, other researchers have also reported that the administration of TMP to STZ-induced diabetic mice or diet-induced hyperlipidemic mice decreases the serum TC and TG levels compared with controls [4, 24]. The cholesterol-lowering property of EEYR could be attributed to several factors like some components of EEYR and YRP may act as inhibitors for some enzymes such as hydroxyl methyl glutaryl CoA reductase, which participates in cholesterol synthesis; these components reduce the absorption of cholesterol from the intestine or increase the glucose metabolism velocity which in turn inhibits lipid synthesis or reduces lipid peroxidation.
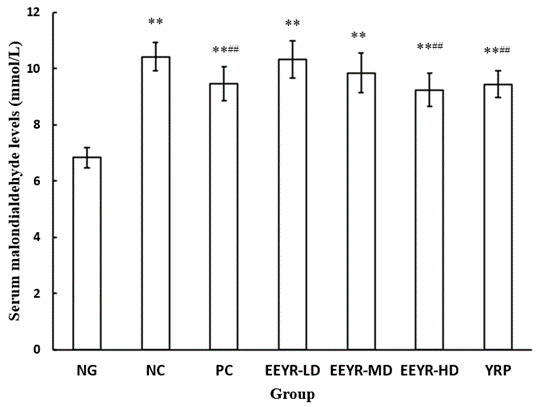
VI Effect of EEYR and YRP on Lipid Peroxidation (LPO)
MDA is one of the major products of LPO. MDA has often been used as a marker of LPO and oxidative stress, and the determination of MDA level can reflect the degree of antioxidant activity [25, 26]. In the present study, the serum MDA level of the NC group (10.43±0.498 mmol/L) was higher than that of the BC group (6.838±0.364 mmol/L) (Figure 4). Administration of EEYR or YRP significantly reduced the serum MDA level with the increase of dosage compared with the NC group (p<0.01). The LPO level in cells is controlled by various internal cellular defense mechanisms, including enzymatic and non-enzymatic scavenger systems. These defense mechanisms are altered in diabetes [27, 28]. The scavenging ability of free radicals may directly determine the extent of tissue injury.
Figure 4: Effect of YRP on the levels of MDA in the plasma of diabetic mice.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.
The increased serum MDA content of STZ-treated animals (NC group) could be attributed to the increased levels of oxygen-free radicals. The increased levels of oxygen-free radicals result in the peroxidation of membrane phospholipids, further changing the permeability, leading to a loss of membrane integrity and finally resulting in their cytotoxic effect [29, 30]. Treatment of EEYR or YRP for 30 days significantly decreased the serum MDA level in diabetic mice compared with the NC group. The reduction of MDA levels could enhance the antioxidant activity of animals. Our previous studies have demonstrated that TBE and TMP have anti-peroxidative properties [7]. Our results were in agreement with Rajesh et al. and Peipei et al., in which the level of lipid peroxides in the plasma of diabetic rats is increased [31, 32].
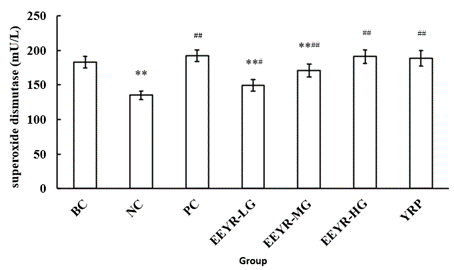
VII Effect of EEYR and YRP on SOD
Excess reactive oxygen species (ROS) is considered as one of the principal reasons for STZ-induced oxidative damage, particularly in the liver and kidney [33]. Cells scavenge ROS by enzymatic and non-enzymatic antioxidant systems. The primary antioxidant enzymes, including SOD, catalase and GSH-Px, play a foundational role in defense against ROS in the body [34]. Intracellular SOD has been shown to play a pivotal role in protecting human leukemic and cancer cells against oxygen free radicals, anticancer drugs and radiation [35]. Figure 5 shows that the SOD level was significantly decreased in the serum of STZ-induced diabetic mice (NC group, 135.16±5.970 mU/L) compared with the BC group (182.86±8.355 mU/L) (p<0.05). After the 30-day treatment of EEYR at different doses or YRP, the serum SOD levels were all significantly increased (p<0.01). The result was consistent with our previous findings [7].
Figure 5: Effect of YRP on the SOD activities in the plasma of diabetic mice.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.
VIII Clinical Trials of YRP Hypoglycemic Effects on Diabetic Patients
To explore the hypoglycemic effects of YRP on diabetic patients, FBG and PBG levels of diabetic patients were determined at regular intervals during the trial period (Additional file 1 and Table 4). Figure 6 shows the statistical analysis of FBG and PBG data. The Additional file 1 shows that the FBG levels of 72 diabetic patients and PBG levels of 73 diabetic patients were decreased at various degrees, and the FBG and PBG levels of other 28 diabetic patients were nearly stable compared with their FBG and PBG levels before ESYR administration instead of chemical drug administration. Figure 6 exhibits that the average FBG and PBG levels of 100 diabetic patients were decreased from 8.038 mmol/L and 9.912 mmol/L before ESYR administration to 7.261 mmol/L and 8.498 mmol/L, respectively. During the trial period, a small increase in FBG and PBG levels was found after 15 days of ESYR administration. Although no significant differences in FBG and PBG levels before and after ESYR administration were found and these diabetic volunteers all took other chemical drugs, we believed that the clinical trials confirmed the hypoglycemic activities of ESYR. Because EEYR and ESYR were ethanol extracts of YRP, our findings confirmed that YRP possessed hypoglycemic activities, evidenced by both the animal test and clinical test.
Figure 6: Effect of ESYR on FBG and PBG levels of diabetic patients.
Table 4: The biomedical components
content of YRP, EEYR and ESYR. * The content of saponin was calculated as
ginsenoside R1.
|
Sample |
Polysaccharide |
Saponin* |
|
YRP (mg/g) |
6.164 |
0.842 |
|
EEYR (mg/g) |
78.3 |
25.6 |
|
ESYR (mg/mL) |
6.34 |
2.57 |
Conclusion
Collectively, our study demonstrated the better hypoglycemic effect of YRP on STZ-induced diabetic mice and diabetic patients. Specifically, YRP reduced the FBG and PBG levels in diabetic mice and diabetic patients. YRP decreased serum TC, TG and MDA levels and increased the serum SOD activities in diabetic mice. YRP could not increase the serum insulin levels. The significantly increased PBG level and fairly stable serum insulin level confirmed that YPG decreased the FBG level by increasing glucose metabolism velocity but not insulin sensitivity. Taken together, we showed that YRP could be used as a promising anti-diabetic food in the management of diabetes.
Funding
This work was supported by the grant from the National Natural Science Foundation of China (40773069), Natural Science Foundation of Jiangsu Province (No. BK20160493), Chinese Postdoctoral Science Fund (Grant No. 20080440810), and Nantong Social Development Fund (S2011003).
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 31, Aug 2021Accepted: Thu 16, Sep 2021
Published: Wed 06, Oct 2021
Copyright
© 2023 Zhicai Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JFNM.2021.02.03
Author Info
Quanshan Sun Ling Xu Zhicai Zhang Wenjing Shi Xiaocui Liu Chongyang Ding Huihua Zheng Feng Wang
Corresponding Author
Zhicai ZhangInstitute of Agro-Production Processing Engineering, Jiangsu University, Zhenjiang, P. R. China
Figures & Tables
Table 1: Effect of YRP on the body weight of diabetic mice (g).
|
Group |
0 |
10d |
20d |
30d |
|
BC |
18.98±2.63 |
20.66±2.50 |
23.02±2.57 |
24.84±1.90 |
|
NC |
18.56±2.74 |
18.80±2.25 |
18.88±1.65** |
19.08±1.78** |
|
PC |
18.88±2.81 |
20.29±2.45 |
21.53±2.48## |
23.12±2.59## |
|
EEYR-LD |
18.76±2.85 |
19.77±3.06 |
20.63±3.11 |
21.57±3.16** |
|
EEYR-MD |
18.67±2.70 |
19.88±2.79 |
21.06±2.67 |
22.02±2.53**## |
|
EEYR-HD |
18.77±2.98 |
20.49±3.02 |
22.32±2.86## |
23.52±2.10## |
|
YRP |
18.79±2.97 |
19.56±2.70 |
20.67±2.52 |
22.54±2.29**## |
a Values are expressed as
means ± SD (n = 10); * As compared with BC group: p<0.05, ** As compared
with BC group: p<0.01; # As compared with NC group: p<0.05, ##
As compared with NC group: p<0.01.
Table 2: Effect of EEYR and YRP on the blood sugar levels of diabetic
mice (mmol/L).
|
Group |
0 |
10d |
20d |
30d |
|
BC |
6.12±0.25 |
6.18±0.21 |
6.24±0.19 |
6.27±0.11 |
|
NC |
20.31±2.70** |
20.63±2.59** |
21.01±2.83** |
21.20±2.93** |
|
PC |
20.33±2.67** |
18.46±2.65** |
17.11±2.86**## |
15.82±3.08**## |
|
EEYR-LD |
20.38±2.64** |
20.18±2.76** |
19.23±2.70** |
18.30±2.87**## |
|
EEYR-MD |
20.34±2.68** |
19.46±2.63** |
18.02±2.50**# |
17.00±3.44**## |
|
EEYR-HD |
20.39±2.65** |
18.00±2.68** |
16.46±3.38**## |
14.79±2.56**## |
|
YRP |
20.34±2.61** |
18.51±3.34** |
16.98±3.05**## |
15.49±3.05**## |
a Values are expressed as means ± SD (n = 10); *
As compared with BC group: p<0.05, ** As compared with BC group: p<0.01; #
As compared with NC group: p<0.05, ## As compared with NC group:
p<0.01.
Table 3: Effect of YRP on the glucose tolerance tests of diabetic mice
(mmol/L).
|
Group |
0 |
30 min |
60 min |
120 min |
|
BC |
6.27±0.11 |
8.58±0.44 |
7.38±0.33 |
6.35±0.20 |
|
NC |
21.20±1.93 |
28.81±1.76 |
27.41±1.30 |
26.05±2.16 |
|
PC |
15.82±1.08 |
29.46±2.37 |
26.07±2.30 |
22.23±2.46## |
|
LD |
18.30±1.87 |
30.24±2.91 |
28.18±2.48 |
26.24±2.86 |
|
MD |
17.00±1.44 |
30.41±3.10 |
28.26±2.73 |
25.39±2.60 |
|
HD |
14.79±1.56 |
27.92±3.11 |
25.21±2.20 |
21.86±2.58## |
|
YRP |
15.49±1.05 |
28.68±2.41 |
24.82±2.12 |
21.44±2.47## |
a Values are expressed as means ± SD (n = 10); *
As compared with BC group: p<0.05, ** As compared with BC group: p<0.01; #
As compared with NC group: p<0.05, ## As compared with NC group:
p<0.01.
Table 4: The biomedical components
content of YRP, EEYR and ESYR. * The content of saponin was calculated as
ginsenoside R1.
|
Sample |
Polysaccharide |
Saponin* |
|
YRP (mg/g) |
6.164 |
0.842 |
|
EEYR (mg/g) |
78.3 |
25.6 |
|
ESYR (mg/mL) |
6.34 |
2.57 |
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p< 0.01. Compared with NC group, # p<0.05, ## p<0.01.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p< 0.05, ## p<0.01.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.
Values are expressed as means ± SD for 10 mice in each group. Compared with BC group, * p<0.05, ** p<0.01. Compared with NC group, # p<0.05, ## p<0.01.

References
1. Ma L, Lin ZB (1992)
Effect of Tremella polysaccharide
on IL-2 production by mouse splenocytes. Yao Xue Xue Bao 27: 1-4. [Crossref]
2. Ukai S, Hirose K,
Kiho T, Hara C, Irikura T (1972) Antitumor activity on sarcoma 180 of the
polysaccharides from Tremella fuciformis Berk. Chem Pharm Bull 20:
2293-2294. [Crossref]
3. Kiho T, Kochi M,
Usui S, Hirano K, Aizawa K et al. (2001) Antidiabetic effect of an acidic
polysaccharide (TAP) from Tremella aurantia and its degradation product
(TAP-H). Bio Pharm Bull 24: 1400-1403. [Crossref]
4. Wang H, Qu WJ, Chu
SD, Li MJ, Tian CP (2002) Studies on the Preventive and Therapeutic Effects of
the Polysaccharide of Tremella
aurantiabla Mycelia on Diet-induced Hyperlipidemia Mice. Acta Nutrimenta Sinica 24: 431-433.
5. Zhang J, Tang Q,
Kordmann MZ, Reutter W, Fan H (2002) Activation of B lymphocytes by GLIS, a
bioactive proteoglycan from Ganoderma lucidum. Life Sci 71: 623-638. [Crossref]
6. Zhang ZC, Zhang KC
(2006) Hypoglycemic and antihyperglycemic activity of Tremella aurantialba broth extract in diabetic mice (II). Natural Product Research Development 18: 613-616.
7. Zhang ZC, Lian B,
Huang DM, Cui FJ (2009) Compare activities on regulating lipid-metabolism and
reducing oxidative stress of diabetic rats of Tremella aurantialba broth's
extract (TBE) with its mycelia polysaccharides (TMP). J Food Sci 74:
H15-H21. [Crossref]
8. Coursey DG (1967)
Yams, an account of the nature, origins, cultivation, and utilization of the
useful members of dioscoreaceae. London: Longmans, Green and Co. Ltd.
244.
9. Cayen MN, Dvornik D
(1979) Effect of diosgenin on lipid metabolism in rats. J Lipid Res 20:
162-174. [Crossref]
10. Prasanna M (2000)
Hypolipidaemic effect of fenugreek. A
clinical study. Phytother Res 32: 34-36.
11. Sharma B,
Balomajumder C, Roy P (2008) Hypoglycemic and hypolipidemic effects of
flavonoid rich extract from Eugenia jambolana seeds on streptozotocin induced
diabetic rats. Food Chem Toxicol 46: 2376-2383. [Crossref]
12. Shen L, Feng Y, Xu
DS, Yuan SY, Zhou D (2007) Colorimetric method determined the content of total
saponins innotoginseng flower extracts.
Chinese Traditional Patent Medicine 29:
1368-1370.
13. Zhang ZC, Wang J,
Liu L, Shun QS, Shi WJ et al. (2019) The optimum conditions and mechanism for
increasing exo-polysaccharide production of Truffles melanosporum by dioscorea
saponins. LWT - Food Science and
Technology 107: 331-339.
14. Kim SH, Hyun SH,
Choung SY (2006) Anti-diabetic effect of cinnamon extract on blood glucose in
db/db mice. J Ethnopharmacol 104: 119-123. [Crossref]
15. Zhang Z, Cui FJ
(2007) Non-enzymatic glycosylation reaction contributes to a rise of blood
glucose in alloxan-induced diabetic rats. Int
J Diabetes & Metabolism 15:
52-59.
16. Su BN, Xie H, Wang
CQ, Liu CH, Han JX et al. (2004) Effects of fermented liquid of Tremella aurantialba to blood sugar and
glucose tolerance of rabbits. Edible
Fungi of China 23: 41-43.
17. Akindele AJ,
Otuguor E, Singh D, Ota D, Benebo AS (2015) Hypoglycemic, antilipidemic and
antioxidant effects of valproic acid in alloxan-induced diabetic rats. Eur J Pharmacol 762: 174-183. [Crossref]
18. Emordi JE, Agbaje
EO, Oreagba IA, Iribhogbe OI (2016) Antidiabetic and hypolipidemic activities
of hydroethanolic root extract of Uvaria chamae in streptozotocin induced
diabetic albino rats. BMC Complement and
Altern Med 16: 468. [Crossref]
19. Ktari N, Mnafgui K,
Nasri R, Hamden K, Bkhairia I et al. (2013) Hypoglycemic and hypolipidemic
effects of protein hydrolysates from zebra blenny (Salaria basilisca) in
alloxan-induced diabetic rats. Food Funct
4: 1691-1699. [Crossref]
20. Moodley K, Joseph
K, Naidoo Y, Islam S, Mackraj I (2015) Antioxidant, antidiabetic and
hypolipidemic effects of Tulbaghia violacea Harv. (wild garlic) rhizome
methanolic extract in a diabetic rat model. BMC
Complement and Altern Med 15: 408. [Crossref]
21. Rangika BS,
Dayananda PD, Peiris DC (2015) Hypoglycemic and hypolipidemic activities of
aqueous extract of flowers from Nycantus arbor-tristis L. in male mice. BMC Complement Altern Med 15: 289. [Crossref]
22. Weng Y, Yu L, Cui
J, Zhu YR, Guo C et al. (2014). Antihyperglycemic, hypolipidemic and
antioxidant activities of total saponins extracted from Aralia taibaiensis in
experimental type 2 diabetic rats. J
Ethnopharmacol 152:
553-560. [Crossref]
23. Xiong WT, Gu L,
Wang C, Sun HX, Liu X (2013) Anti-hyperglycemic and hypolipidemic effects of
Cistanche tubulosa in type 2 diabetic db/db mice. J Ethnopharmacol 150:
935-945. [Crossref]
24. Zhang W, Zhao JJ, Wang
JS, Zhu XL, Zhang M et al. (2010) Hypoglycemic activity of polysaccharides
extracted from Tremella Aurantialba
myceliain experimental type 2 diabetic rats. Natural Product Research and Development 22: 49-53. (in Chinese).
25. Janero DR (1990)
Malondialdehyde and thiobarbituric acid-reactivity as diagnostic indices of
lipid peroxidation and peroxidative tissue injury. Free Radic Biol Medicine 9:
515-540. [Crossref]
26. Abuja PM, Albertini
R (2001) Methods for monitoring oxidative stress, lipid peroxidation and
oxidation resistance of lipoproteins. Clin
Chim Acta 306: 1-17. [Crossref]
27. Bagri P, Ali M,
Aeri V, Bhowmik M, Sultana S (2009) Antidiabetic effect of Punica granatum
flowers: effect on hyperlipidemia, pancreatic cells lipid peroxidation and
antioxidant enzymes in experimental diabetes. Food Chem Toxicol 47:
50-54. [Crossref]
28. Wohaieb SA, Goldin
dv (1987) Alterations in free radical tissue defense mechanism in
streptozotocin-induced diabetes in rat. Effect of insulin treatment. Diabetes 36: 1014-1048. [Crossref]
29. Elekofehinti OO,
Adanlawo IG, Fakoya A, Saliu JA, Sodehinde SA (2012) Effects of Saponin from
Solanum anguivi Lam Fruit on Heart and Kidney Superoxide Dismutase, Catalase
and Malondialdehyde in Rat. Curr Res J
Biol Sci 4: 530-533.
30. Esterbauer H (1996)
Estimation of peroxidative damage. A critical review. Pathol Biol (Paris) 44:
25-28. [Crossref]
31. Gupta RK, Kesari
AN, Diwakar S, Tyagi A, Tandon V et al. (2008) In vivo evaluation of
anti-oxidant and anti-lipidimic potential of Annona squamosa aqueous extract in
Type 2 diabetic models. J Ethnopharmacol
118: 21-25. [Crossref]
32. Yin P, Zhao S, Chen
S, Liu J, Shi L et al. (2011) Hypoglycemic and hypolipidemic effects of
polyphenols from burs of Castanea mollissima Blume. Molecules 16:
9764-9774. [Crossref]
33. Vinothiya K,
Ashokkumar N (2017) Modulatory effect of vanillic acid on antioxidant status in
high fat diet-induced changes in diabetic hypertensive rats. Biomed Pharmacother 87: 640-652. [Crossref]
34. Phull AR, Majid M, Haq IU, Khan MR, Kim SJ (2017) In vitro and in vivo evaluation of anti-arthritic, antioxidant efficacy of fucoidan from Undaria pinnatifida (Harvey) Suringar. Int J Biol Macromol 97: 468-480. [Crossref]
35. Yamaguchi
S, Sakurada S, Nagumo M (1994) Role of intracellular SOD in protecting human
leukemic and cancer cells against superoxide and radiation. Free Radic Biol Med 17: 389-395. [Crossref]
