An Anchor Flap as a Novel Method for Large Forehead Defects Reconstruction
An Anchor Flap as a Novel Method for Large Forehead Defects Reconstruction
A B S T R A C T
Background: Extensive forehead defects remain a challenge in reconstructive surgery. The choice of reconstruction method is a significant clinical problem, not only for cosmetic reasons but also because of possible complications. The anchor flap provides a promising solution for large (7 cm diameter) skin defects reconstruction in the temple area. In this article, we describe a novel method for extensive forehead defects reconstruction.
Methods: We present a method for reconstruction of forehead skin defect with an Anchor flap after tumor resection. A 78-year-old female patient who received oncologic reconstruction in the present study were included.
Results: There were no early or late complications during the two years of the follow-up period. The flap survived without partial or complete necrosis, infection, or other complications. The aesthetic outcome was very satisfying and well documented.
Conclusion: The Anchor flap enables to achieve tension-free frontotemporal defect closure after tumor resection, with satisfactory clinical and aesthetic results. This method is a reliable reconstructive surgical technique for the reconstruction of extensive forehead defects.
Keywords
Oncologic reconstruction, soft-tissue defect, anchor flap, tumor resection, local flaps of the face
Question: Can use of an anchor flap be an optimal treatment strategy for extensive forehead defect reconstruction?
Findings: An extensive forehead defect after tumor excision was reconstructed with a rotated anchor-like shaped random flap with a pedicle as a shank and skin arms originating in the left preauricular area. Due to naturally occurring excess skin in the preauricular area, reconstruction did not cause distortion, occurring in local flaps due to tension forces. The high survival rate of the flap was due to broad flap pedicle. The postoperative scar at the donor site is inconspicuous and provides the acceptable cosmetic result of the donor area.
Meaning: Repair the skin defects in the temporal region with the use of an anchor flap is a highly effective method that allows achieving a satisfactory aesthetic effect. It can be an optimal treatment strategy for extensive forehead reconstruction.
Introduction
Extensive forehead defects remain a challenge in reconstructive surgery. Mainly the temple area is an essential aesthetical face unit. The anchor flap development provides a promising solution for broad skin defects coverage in the temple area. Considering both, type of the tumor and its localization, the authors had to designate the maximal safe surgical margins, without face distortion and to ensure the most pleasing aesthetic effect. The local flap utilization within the forehead, including temples, is limited due to lack of excessive skin around.
Furthermore, displacing a large flap of the skin from the adjacent area can lead to eyebrow lift and hairline displacement. Unsatisfactory aesthetic effects of flap reconstruction in this area have determined us to invent alternative solutions. The “anchor flap’’ resembles a shank and arms of an anchor. It’s a random, rotation skin flap with a pedicle as a shank and skin arms originating in the preauricular area. In this article, we presented the method and results of using the anchor flap in the extensive forehead defect reconstruction after squamous cell cancer incision.
Methods
A 78-year-old woman was admitted to the Department of Plastic, Reconstructive, and Aesthetic Surgery with a tumor located on the left side of the forehead, involving the temple and adjacent area (Figure 1A). The lesion was growing gradually for a few years. The patient had a history of kidney transplantation and arterial hypertension. The clinical examination showed a well-demarcated, pedunculated, ulcerated tumor. The lesion was 4 x 4 cm in size. The detailed examination didn’t reveal any relevant abnormalities as lymphadenopathy. Basic laboratory tests were normal. The patient was qualified for surgical treatment. The tumor was excised under local anaesthesia with 1% lidocaine, with a 10-15mm margin of normal skin. The final oval defect was 5,5 x 5 cm in size. According to this, the authors planned rotated anchor-like shaped random flap with a pedicle as a shank and skin arms originating in the left preauricular area. This method has not been described in the literature so far (Figures 1B & 1D).
Figure 1: A) Squamous cell carcinoma of the left temporal region; B) Status after tumor excision and reconstruction with the use of anchor flap; C) Long-term follow up. D) Pictures that shows surgical technique: rotation skin flap with a pedicle as a shank and skin arms originating in the preauricular area. The flap is shifted towards the skin defect.
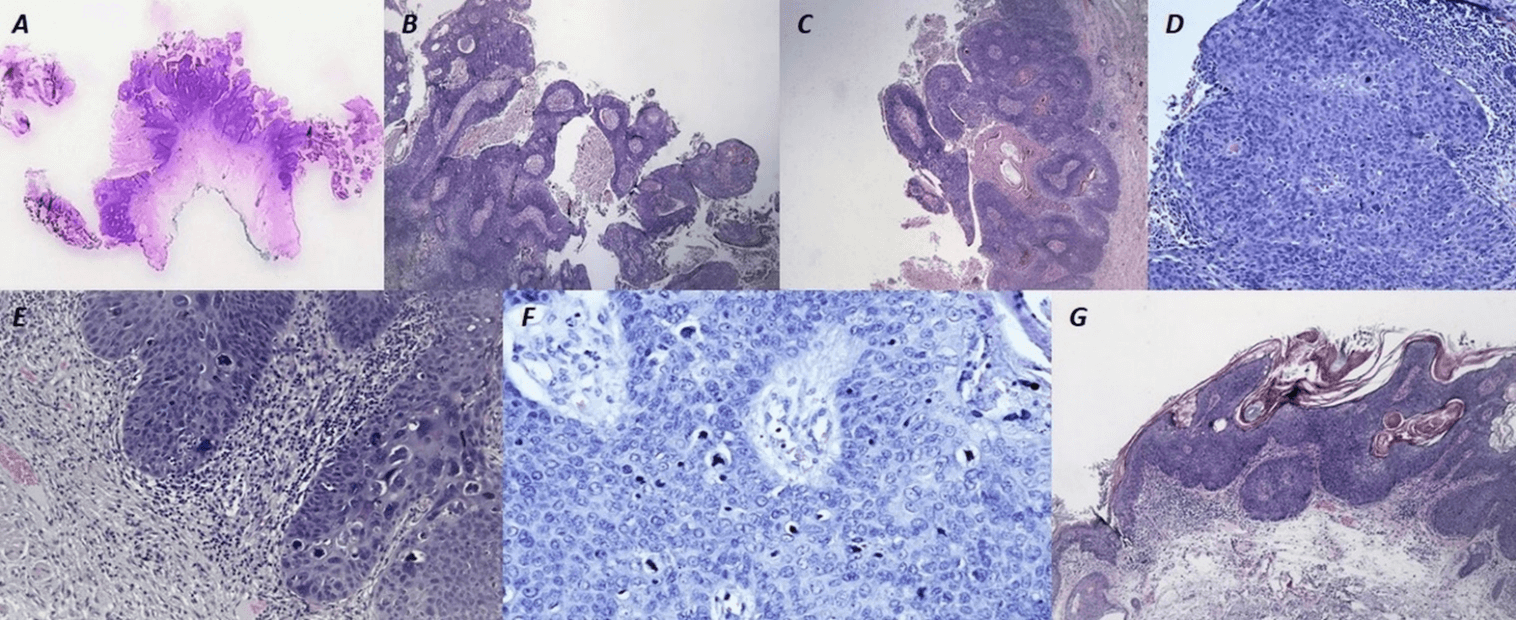
Figure 2: Photographs of microscopic slides. A) Large skin fragment with exophytic, papillary, disintegrating tumor; B) Lesion composed of multiple finger-like projections with fibrovascular cores covered by malignant squamous epithelium with limited surface keratinization. HE, 2x; C) Mainly intact basement membrane of malignant squamous epithelium of the lesion. HE, 2x; D) Full epidermal thickness marked keratinocyte atypia including nuclear hyperchromasia, polymorphism, numerous typical mitotic figures, and individual cell dyskeratosis. HE, 10x; E) Marked keratinocyte atypia, hyperchromasia and multinucleation. HE, 10x; F) Tripolar atypical mitosis in cancer cell. HE, 20x; G) Focus of cancer microinvasion under the basement membrane. HE, 4x.
The excised large skin fragment with exophytic, papillary, disintegrating tumor was sent for histopathological examination (Figure 2A). The surgical margins were preserved. The lesion manifested microscopically as multiple finger-like projections with fibrovascular cores covered by malignant squamous epithelium with limited surface keratinization (Figure 2B). The basement membrane of the malignant squamous epithelium was mainly intact (Figure 2C). There was full epidermal thickness marked keratinocyte atypia, including nuclear hyperchromasia, polymorphism, numerous typical mitotic figures (Figures 2D & 2E) and a few atypical mitotic figures (Figure 2F). Focally there were signs of micro invasion (Figure 2G). Based on microscopic examination and clinical data, the diagnosis of papillary squamous cell cancer with micro invasion, pT2NXMX, was made.
Results
There were no early complications observed at one month after surgery. The flap survived without partial or complete necrosis, infection, or other complications. We found no signs of recurrence or distal metastasis during the 12- months follow up period. The scar as acceptable in the twelfth month postoperatively was regarded. The colour, texture, and thickness of the surgical area were similar to the surrounding tissues leading to a satisfying aesthetic effect (Figure 1C).
Discussion
A skin defect after the surgical procedure is inevitable. Considering the size, histological type, and localization of the skin lesion, age, and comorbidities of the patient and expected aesthetic and functional effects, surgeons may opt for the most popular reconstructive technique as primary closure, skin graft (full-thickness or split-thickness) or skin flap [1-3]. In the case of an isolated skin loss, a skin graft seems to be an excellent choice [4]. In the case of a deep lesion with wide excision of tissues, a subcutaneous pedicle flap fits the needs, mainly according to the depth of the defect, colour of the surrounding skin, presence of skin appendages, and tissue functions [4, 5]. Furthermore, skin flaps are more resistant to external injuries as postoperative radiotherapy is used, for instance, in the therapy of squamous cell carcinomas within the face [6, 7]. Flaps are usually classified as local, regional, distant, or free, depending on their origin, blood supply, complexity, and method of transition [8]. The most commonly used reconstruction methods in the face are local flaps, including V-Y advancement flaps, rotational flaps, nasolabial flaps, forehead flaps, Estlander flap, and Karapandzic flap [9, 10].
Furthermore, according to their blood supply, they may be classified as axial or random flaps [11, 12]. The first-mentioned type includes an axial blood vessel at its base. The second one acquires vascular supply from perforating vessels, thus named random-pattern perforator flap, including facial artery perforator flap commonly used in facial reconstruction [12, 13]. The ‘‘anchor flap’’ designed in our case resembled the shank and arms of an anchor. It’s a random, rotation skin flap with a pedicle as a shank and skin arms originating in the preauricular area. First of all, this rotation flap uses preauricular skin excess, which eliminates distortions occurring in local flaps due to tension forces. Secondly, the shade of the skin from the parotid area is very similar to the colour of the forehead skin, ensuring acceptable aesthetic effect. The part of the anchor flap with hair follicles gives the possibility to rebuild the hairline if necessary. So far, no local flaps allow moving the skin and recreating the hairline simultaneously. Although the lobe is random and rotational, the broad flap pedicle guarantees adequate blood supply with a high survival rate. Finally, it should be emphasized that the postoperative scar at the donor site is practically invisible.
Two papers used the term “anchor flap” in two distinct situations. In our opinion, these flaps were misnamed. The first publication utilized the term “anchor flap” to describe a classic rotation flap for decubital surgery [14, 15]. In the second paper, the flap is named imprecisely, because only the scar after the reconstruction resembled an anchor [16]. Two bilateral rotation flaps recalling inverted T-plasty were used. Only in our case, the flap’s shape resembled an anchor (Figures 2A & 2B). Our innovative anchor flap demonstrates its versatility and highlights its advantages for extensive forehead defects reconstruction.
Conclusion
Repair the skin defects in the temporal region with the use of an anchor flap is a highly effective method that allows achieving a satisfactory aesthetic effect. Due to naturally occurring excess skin in the preauricular area, reconstructing the defect does not cause skin tension that could impede the healing process and distort the operated area. The broad flap pedicle provides adequate blood supply to the flap, which has a significant impact on the survival rate. The skin shade of the parotid area from which the lobe originates is very similar to forehead skin, which provides an excellent aesthetic effect. Furthermore, a fragment of the anchor flap containing the hair follicles allows reconstruction of the hairline if the skin defect involves a piece of the scalp. The postoperative scar at the donor site is inconspicuous and provides the acceptable cosmetic result of the donor area. We conclude that this can be the first choice for closing forehead skin defects, allowing a better aesthetic result, and concealing of scars.
Acknowledgment
The authors thank the patient for granting permission to publish this information.
Disclosure
The authors has no financial interest to declare in relation to the content of this article.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 26, Sep 2020Accepted: Mon 12, Oct 2020
Published: Wed 21, Oct 2020
Copyright
© 2023 Karolina Pisanko. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.10.08
Author Info
Jundziłł Arkadiusz Karolina Pisanko Malinowski Łukasz Męcińska-Jundziłł Kaja Tomasz Kloskowski Neska-Długosz Izabela Grzanka Dariusz Pokrywczyńska Marta Witmanowski Henryk
Corresponding Author
Karolina PisankoDepartment of Plastic, Reconstructive and Aesthetic Surgery, Ludwik Rydygier Medical College, Bydgoszcz, Nicolaus Copernicus University, Torun, Poland
Figures & Tables

References
- Andreassi A, Bilenchi R, Biagioli M, D'Aniello C (2005) Classification and pathophysiology of skin grafts. Clin Dermatol 23: 332-337. [Crossref]
- Kwon KH, Lee DG, Koo SH, Jo MS, Shin H et al. (2012) Usefulness of v-y advancement flap for defects after skin tumor excision. Arch Plast Surg 39: 619-625. [Crossref]
- Tschoi M, Hoy EA, Granick MS (2009) Skin flaps. Surg Clin North Am 89: 643-658. [Crossref]
- Bhattacharya V (2012) Management of soft tissue wounds of the face. Indian J Plast Surg 45: 436-443. [Crossref]
- Ito O, Yano T, Kawazoe T, Suzuki S (2015) Flexible Curved V-Y Subcutaneous Flap for Facial Skin Defects. Plast Reconstr Surg Glob Open 3: e531. [Crossref]
- Park JS, Ahn SH, Son BH, Kim EK (2015) Using local flaps in a chest wall reconstruction after mastectomy for locally advanced breast cancer. Arch Plast Surg 42: 288-294. [Crossref]
- Mendenhall WM, Hinerman RW, Amdur RJ, Malyapa RS, Lansford CD (2006) Postoperative radiotherapy for squamous cell carcinoma of the head and neck. Clin Med Res 4: 200-208. [Crossref]
- Ebrahimi A, Ashayeri M, Rasouli HR (2015) Comparison of Local Flaps and Skin Grafts to Repair Cheek Skin Defects. J Cutan Aesthet Surg 8: 92-96. [Crossref]
- Lee KS, Kim JO, Kim NG, Lee YJ, Park YJ (2017) A Comparison of the Local Flap and Skin Graft by Location of Face in Reconstruction after Resection of Facial Skin Cancer. Arch Craniofac Surg 18: 255-260. [Crossref]
- Rao JK, Shende KS (2016) Overview of Local Flaps of the Face for Reconstruction of Cutaneous Malignancies: Single Institutional Experience of Seventy Cases. J Cutan Aesthet Surg 9: 220-225. [Crossref]
- Memarzadeh K, Sheikh R, Blohmé J, Torbrand C, Malmsjö M (2016) Perfusion and Oxygenation of Random Advancement Skin Flaps Depend More on the Length and Thickness of the Flap Than on the Width to Length Ratio. Eplasty 16: e12. [Crossref]
- Kim JT, Kim SW (2015) Perforator Flap versus Conventional Flap. J Korean Med Sci 30: 514-522. [Crossref]
- Gunnarsson GL, Jackson IT, Thomsen JB (2014) Freestyle facial perforator flaps-a safe reconstructive option for moderate-sized facial defects. Eur J Plast Surg 37: 315-318. [Crossref]
- Erba P, di Summa PG, Raffoul W, Schaefer DJ, Kalbermatten DF (2011) Tip anchor flap in decubital surgery. Aesthetic Plast Surg 35: 1133-1136. [Crossref]
- Dockery G, Crawford M (2012) Lower Extremity Soft Tissue & Cutaneous Plastic Surgery Second Edition. Elsevier Health Sciences 177-193.
- Leonard AL, Hanke CW (2007) The anchor flap: a myocutaneous, biaxial pattern flap for postsurgical defects of the nasaldorsum and tip. Dermatol Surg 33: 1110-1115. [Crossref]
