A Rare Case of Metastatic Mucinous Breast Carcinoma as a First Presentation of Colon Cancer in a Male Patient: Case Report and Review of the Literature
A Rare Case of Metastatic Mucinous Breast Carcinoma as a First Presentation of Colon Cancer in a Male Patient: Case Report and Review of the Literature
A B S T R A C T
The majority of breast tumors are primary; however metastatic tumor to the breast from extramammary sites has an incidence of 0.5 to 3% and can be misinterpreted clinically as a primary breast tumor. We report a case of metastatic mucinous breast carcinoma as a first presentation from colon cancer in a male patient who hasn’t had any bowel symptoms. The immunohistochemical study helped in suspecting the diagnosis, which was then confirmed by CT scan abdomen and pelvis and endoscopic biopsy of the colonic lesion. Management of such patients usually by palliative chemotherapy due to the aggressive nature of the disease however, surgical intervention may be indicated in symptomatic patient or risk of tumor ulceration as in our patient.
Keywords
Mucinous, breast cancer, metastasis, colon cancer
Introduction
Tumors of the breast are either primary or metastatic disease to the breast. The majority are primary tumors while metastatic spread to the breast from extramammary sites has an incidence of 0.5 to 3% [1]. A contralateral breast carcinoma constitutes the most commonly seen metastasis in breast followed by metastasis from hematopoietic neoplasms, malignant melanoma, sarcoma, lung, prostate, ovary and gastric neoplasms. A colon cancer metastasis to breast forms a very small proportion [2]. Metastatic tumors in the breast may be the first presentation of a malignant tumor elsewhere in the body and can be misinterpreted clinically as a primary breast tumor. They are usually seen in patients with disseminated malignancies [1]. This is extremely important as the treatment differs greatly from that of primary breast cancer.
Case Presentation
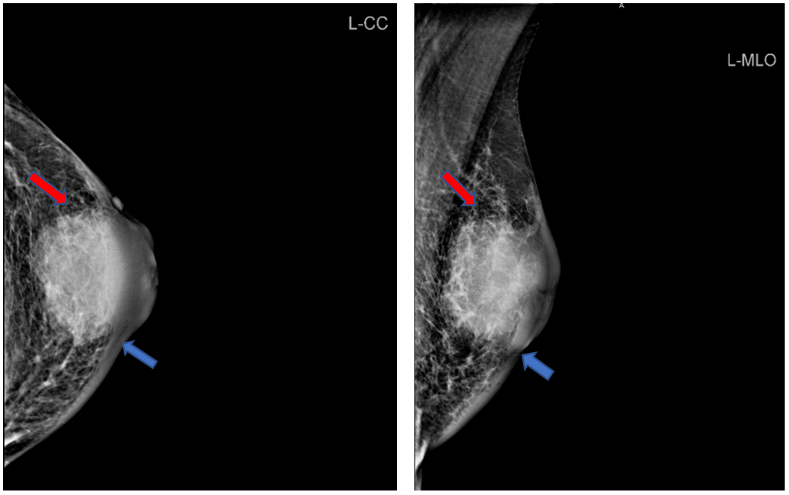
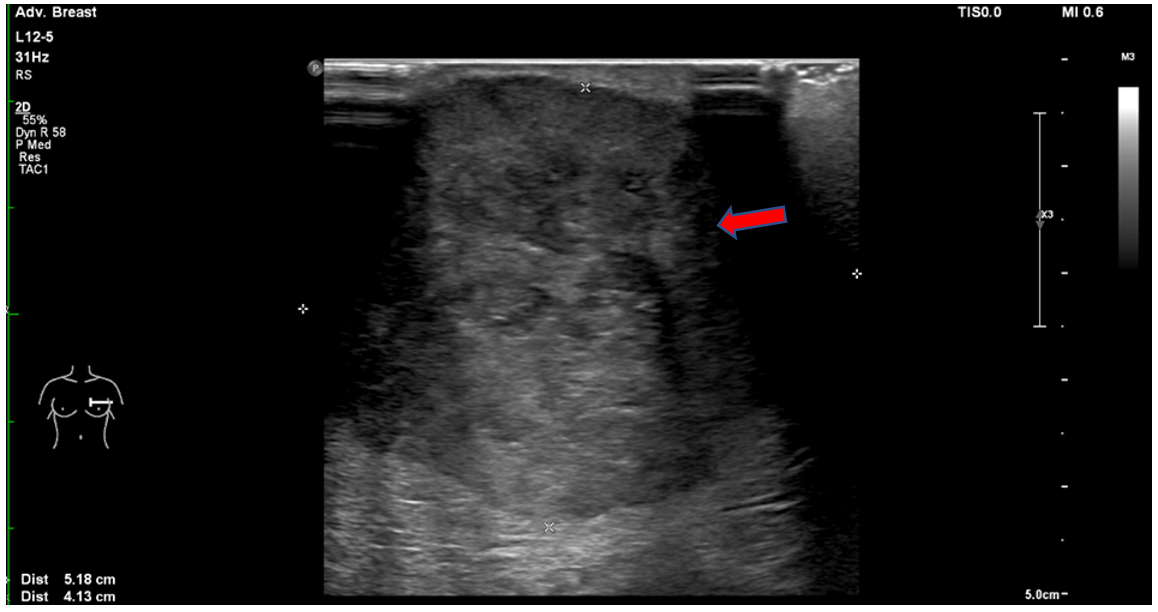
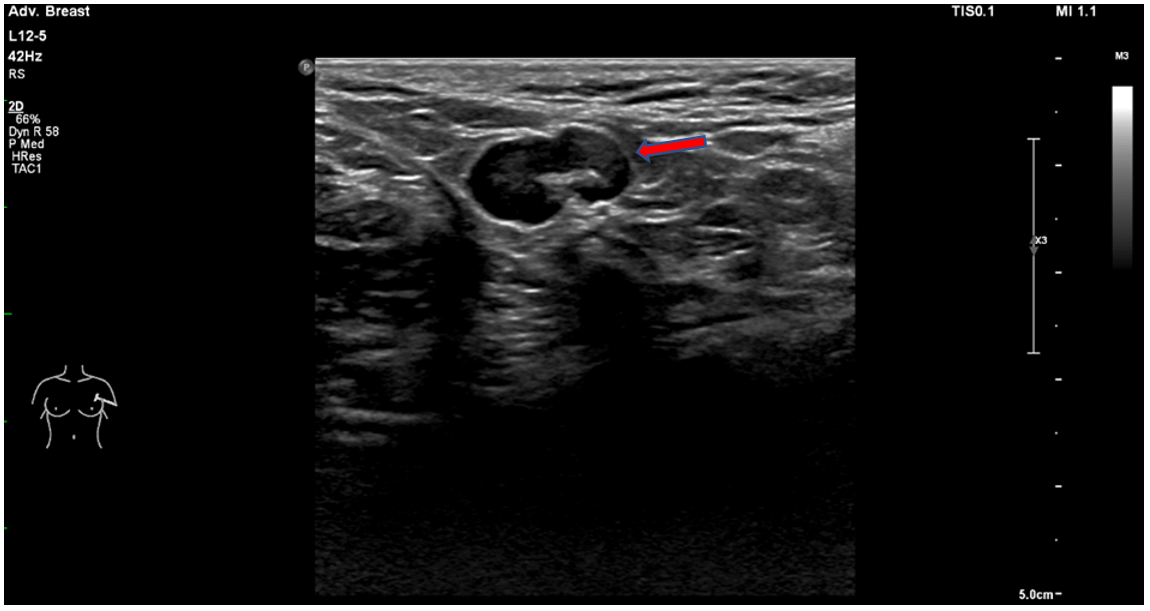
61-year-old gentleman presented with a gradually increasing left breast lump over 9 weeks period. The review of systems was normal and there was no family history of breast cancer. On examination, there was an obvious 5 cm lump in the left breast with overlying thin skin. It was firm in consistency. It was highly suspicious of malignancy. There was a palpable left axillary lymph node. The patient underwent triple assessment of the breast lump. A bilateral mammogram showed on the left side a large irregular high-density lesion around 53 x 49 mm with secondary malignant features of skin thickening and involvement of the dermis (Figures 1 & 2). Left breast ultrasound demonstrated an irregular ill-defined lesion measuring at least 52 x 42 mm in its maximum dimension. The lesion involved the dermis. The imaging appearances were in keeping with a large malignancy (Figure 3). Ultrasound examination of the left axilla demonstrated an equivocal axillary lymph node (Figure 4).
Figure 1: Left cranio-caudal projection. Figure 2: Left mediolateral projection.
Demonstrating a large irregular high-density lesion (red arrow) measuring approximately 53.1 x 49.5 mm with secondary malignant features of skin thickening and involvement of the dermis (blue arrow).
Figure 3: Left breast ultrasound demonstrating an irregular ill-defined lesion involving the dermis measuring at least 52 x 42 mm in its maximum dimension (red arrow).
Figure 4: Equivocal axillary lymph node displaying a compressed hilum and eccentric cortical thickening (red arrow).
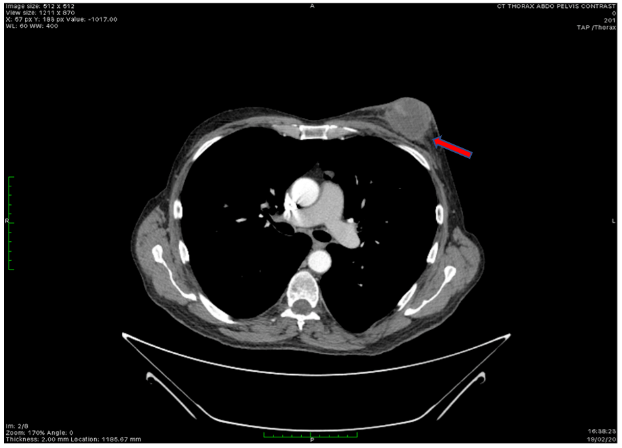
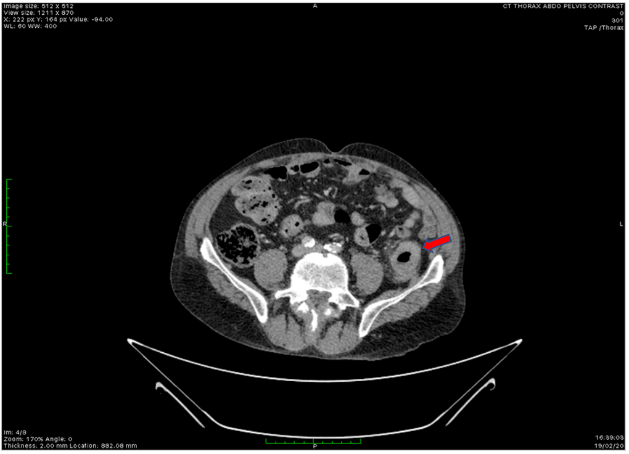
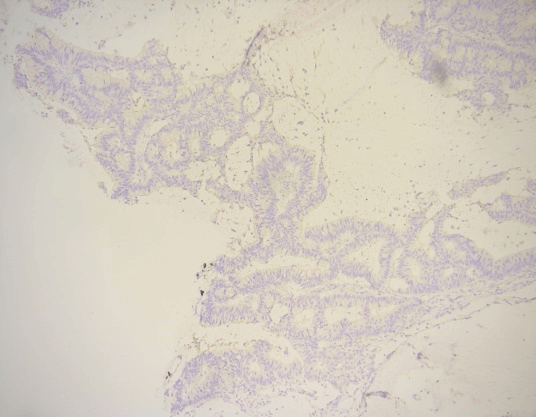
Ultrasound-guided core biopsy of the breast lesion demonstrated infiltration by invasive mucinous carcinoma. ER, PR and Her2 were negative. Ultrasound-guided core biopsy of the left axillary lymph node was normal. Further immunohistochemistry showed staining of the tumor cells for CK 20 and focal moderately strong nuclear staining for CDX2. There was a failure to stain for CK7, TTF-1, or GATA3. These findings raise the suspicion of metastasis to the breast, especially from the gastrointestinal tract. CT scans of chest, abdomen, and pelvis and bone scan were performed. The chest CT scan showed a 5 cm soft tissue mass in the left breast with a thin clear fat plane between the mass and the chest wall musculature (Figure 5). CT scan of the abdomen and pelvis showed focal segmental thickening of the distal descending colon and was considered very suspicious for colonic malignancy (Figure 6). There was no evidence of bony metastases on bone scan.
Figure 5: The chest CT scan showed a 5 cm soft tissue mass in the left breast with a thin clear fat plane between the mass and the chest wall musculature (red arrow).
Figure 6: CT scan of the abdomen and pelvis demonstrating focal segmental thickening of the distal descending colon, considered very suspicious for colonic malignancy (red arrow).
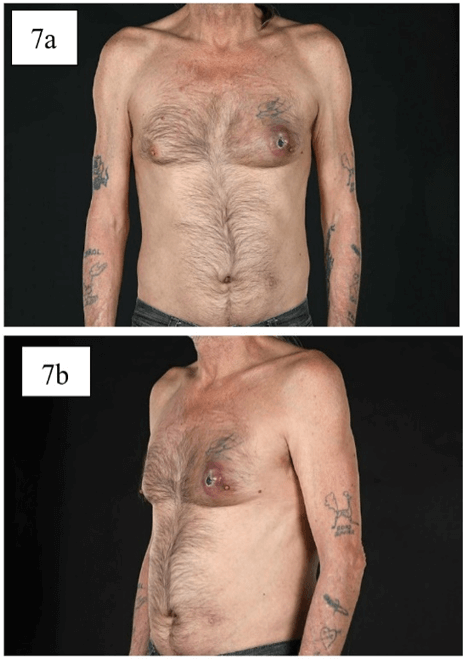
The patient was urgently referred to the colorectal team to clarify the colonic lesion. He underwent a lower GI endoscopy, which showed a lesion in the descending colon but no evidence of obstruction. The biopsy of the colonic lesion was in keeping with a moderately differentiated adenocarcinoma of the colon. In view of primary colonic carcinoma with metastasis to breast, the patient was referred to oncology for palliative chemotherapy. While he was waiting for the colonic investigations and subsequently waiting to see the oncologist, the lesion rapidly increased in size, measuring 10 cm, became painful and threatening to ulcerate the overlying skin (Figures 7A & 7B). In view of his symptoms and after discussion with the patient and oncologist, the decision was made to go ahead with mastectomy.
Figure 7: a) & b) Left breast lump with imminent skin ulceration.
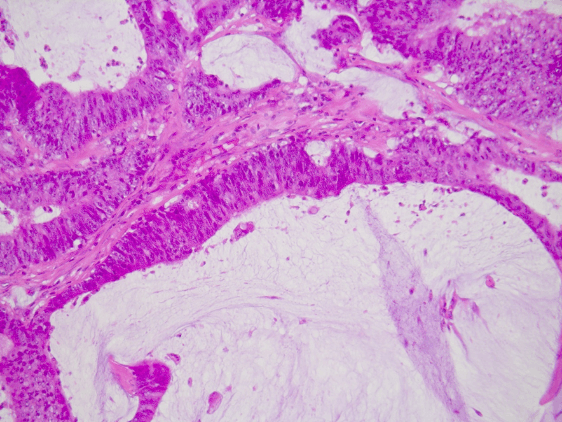
Figure 8: H & E 20X magnification showing pools of acellular mucin with strips of malignant epithelium.
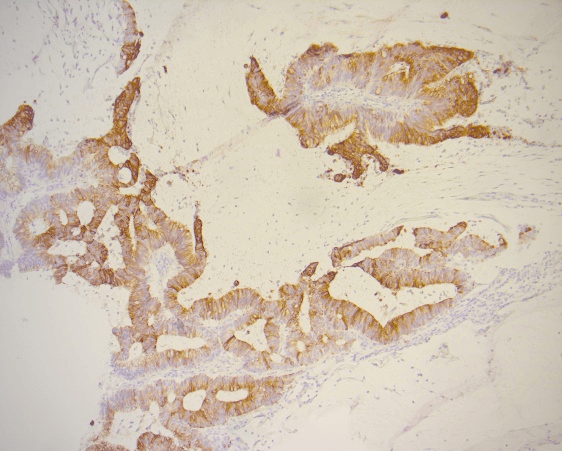
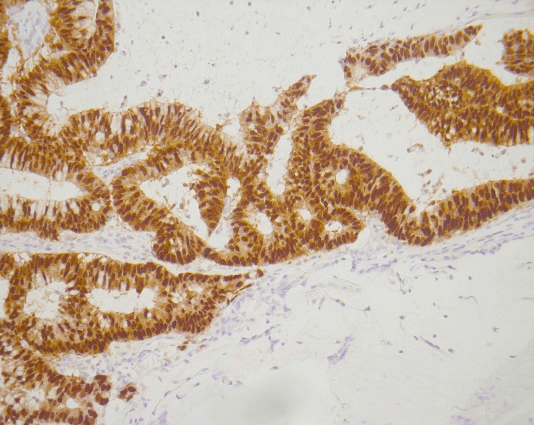
Figure 9: The malignant epithelium is CK 20 positive.
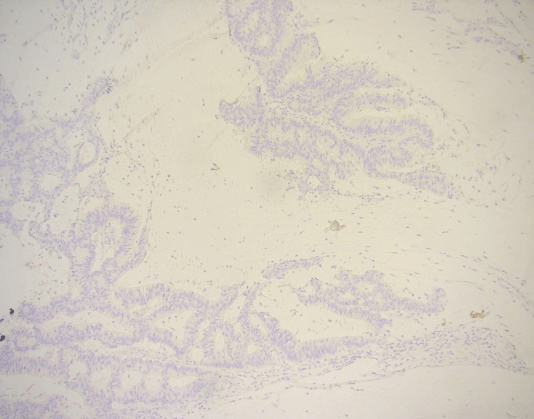
The patient underwent left simple mastectomy and sentinel lymph node biopsy. The histopathological examination of the excised specimen revealed a 130 x 55mm in diameter lesion of moderately differentiated mucinous adenocarcinoma (Figure 8). The carcinoma was CK20 and CDX-2 positive (Figures 9 & 10 respectively). It was negative with CK7 (Figure 11). In addition, it was ER, PR and Her2 negative in the previous core biopsy (Figure 12). These appearances were in keeping with a metastatic colonic mucinous adenocarcinoma. There were smaller tumor deposits in the dermis. All margins were clear. Lymphovascular invasion was present, but the sentinel lymph node biopsy was negative. The gentleman recovered very well from his operation. He was then referred to an oncologist for palliative chemotherapy.
Figure 10: The carcinoma is CDX-2 positive.
Figure 11: The carcinoma is CK 7 negative.
Figure 12: The malignant epithelium is ER negative.
Discussion
Metastatic tumors in the breast from extramammary sites are very rare and constitute 0.5 to 3% [1]. They often occur in the context of polymetastatic disease [3]. A colon cancer metastasis forms a very small proportion [2]. In the published literature 47 cases have been reported; the majority were female with only 4 male patients. The mean age at which breast metastases were detected was 52-year-old. Isolated breast metastases were found in 12 cases and in the majority of cases, breast metastases were diagnosed after a previous diagnosis of colorectal cancer [4, 5]. Zhang et al. reported one case in which the initial presentation was a breast lesion in an 80-year-old female patient with the primary sigmoid tumor that was identified later [6].
To the best of our knowledge, our case is the first case of a male patient who presented with a breast lesion with the primary descending colon tumor that was identified during patient workup. Our patient had no previous cancer history and denied any GI symptoms at the time of presentation. In our case, the breast images’ findings were highly suspicious of malignancy. It is difficult to differentiate between primary or secondary breast cancers radiologically. Core biopsy of the breast lesion showed invasive mucinous carcinoma which, was triple-negative (ER, PR and Her-2). Mucinous breast carcinoma accounts for only 2% of female breast carcinomas and its occurrence in the male breast is extremely rare [7]. Immunoreactivity for ER and/or PR is positive in more than 90% of cases, while HER2 expression is not amplified [7]. Immunohistochemistry can be very helpful in confirming the histological type as well as the tumor origin. According to the literature, the positive immunostaining for CDX2 and CK20 and negative for ER, PR, Her2, GCDP15, BCA, and CK7 are highly sensitive and specific for colonic cancers metastatic to the breast [6].
In our patient, the breast trucut biopsy showed mucinous cancer which was ER, PR and Her2 negative and the immunohistochemistry showed CK7 was negative and CK20 was positive. These were crucial in suspecting the gastrointestinal origin of the tumor as he had no GI symptoms nor any previous history of cancer. Subsequent CT scan, colonoscopy and biopsy from the descending colon confirmed primary colonic cancer. The initial plan was to offer the patient palliative chemotherapy in view of metastatic colonic cancer, and however as the breast lesion was rapidly increasing size and painful and threatening to ulcerate the skin, the decision was taken to perform breast surgery. The management of metastatic breast tumor from colorectal cancer is aimed at toward diagnostic and palliative treatment [1]. Some authors proposed avoidance of surgical excision due to the short life expectancy and risk of seeding to the skin [8]. However, most metastatic breast lumps in the published literature have been excised. This is reasonable if the lump is mistaken for as primary breast cancer or becomes symptomatic as in our case. Unfortunately, the prognosis of patients with metastatic breast tumor of colorectal cancer origin is worse than the general colorectal cancer patients with distant metastases, with a 5-year survival rate of 13.8% due to the highly aggressive nature of breast metastasis from colorectal cancer [4].
Conclusion
When mucinous cancer is noted on breast biopsy in a male patient, then immunohistochemical stains should be performed and detailed clinical history and investigations like CT scan of abdomen and endoscopy of the GI tract should be carried out. This will help to differentiate primary breast cancer from metastatic breast cancer of colonic origin which will help surgeons and oncologists to determine the appropriate further management.
Conflicts of Interest
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 20, Jul 2020Accepted: Thu 06, Aug 2020
Published: Tue 18, Aug 2020
Copyright
© 2023 Zaid Al-Ishaq. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.08.16
Author Info
Zaid Al-Ishaq Meghna Roy B Bickley A Bhatnagar B Isgar T Sircar
Corresponding Author
Zaid Al-IshaqGeneral Surgery Department, Breast unit, New Cross Hospital, The Royal Wolverhampton NHS Trust, Wolverhampton, UK
Figures & Tables
References
- Swei H Tsung (2017) Metastasis of Colon Cancer to the Breast. Case Rep Oncol 10: 77-80. [Crossref]
- Jiten P Kothadia, Rezina Arju, Monica Kaminski, Arvind Ankireddypalli, Sushil Duddempudi et al. (2015) Metastatic colonic adenocarcinoma in breast: report of two cases and review of the literature. Case Rep Oncol Med 2015: 458423. [Crossref]
- C Parrell Soler, A Palacios Marqués, L Saco López, R Bermejo De Las Heras, S Pertusa Martínez (2011) Breast metastatic localization of signet-ring cell gastric carcinoma. ISRN Obstet Gynecol 2011: 426150. [Crossref]
- Tien Chan Hsieh, Chao Wen Hsu (2019) Breast metastasis from colorectal cancer treated by multimodal therapy: Case report and literature review. Medicine 98: e18016. [Crossref]
- Emine Ozlem Gur, Coşkun Onak, Emine Ebru Bayar, Ayşe Yazıcı, İbrahim Kokulu et al. (2020) Rectum mucinous adenocarcinoma metastasis to bilateral breast in a male patient: A case report. Breast J 26: 517-519. [Crossref]
- Shun Zhang, Tao Du, Xiaohua Jiang, Chun Song (2016) Breast metastasis of primary colorectal cancer: A case report. Int J Clin Exp Med 9: 22517-22523.
- Mitsuaki Ishida, Tomoko Umeda, Yuki Kawai, Tsuyoshi Mori, Yoshihiro Kubota et al. (2014) Mucinous carcinoma occurring in the male breast. Oncol Lett 7: 378-380. [Crossref]
- Ludger Barthelmes, James S Simpson, Anthony G Douglas Jones, Helen M Sweetland (2010) Metastasis of primary colon cancer to the breast – leave well alone. Breast Care 5: 23-25. [Crossref]
