Wilkie’s Syndrome: Case Report
Wilkie’s Syndrome: Case Report
A B S T R A C T
Superior mesenteric artery (SMA) syndrome (known as Wilkie's syndrome) is a rare cause of upper gastrointestinal obstruction. A 34-year-old woman presented with nonspecific symptoms of postprandial fullness and important weight loss. After screening for other pathologies, it was diagnosed Wilkie’s syndrome. Within this case it was briefly reviewed the diagnostic study and treatment options including a description of the selected approach, a robotic duodenojejunostomy.
Keywords
Wilkie's syndrome, superior mesenteric artery syndrome, robotic surgery weight loss
Introduction
Superior mesenteric artery (SMA) syndrome is one of uncommon causes of small bowel obstruction. In this syndrome, the 3rd part of duodenum will be compressed between SMA at its origin and abdominal aorta due to decreased angulation leading to partial or complete obstruction [1]. In normal anatomy the aortomesenteric angle and aortomesenteric distance is 25°-60° and 10-28 mm, respectively. This is commonly due to loss of fatty tissue as a result of a variety of debilitating conditions [2]. Third part of duodenum courses posteroinferior in relation to SMA. In general population, the incidence of SMA syndrome ranges between 0.013% and 0.78%. Once a conservative approach fails, usual surgical strategies include Duodenojejunostomy. Robotic Strong's procedure combines both the benefits of a minimal invasive approach and also enchased robotic accuracy and efficacy [1, 2].
Case Report
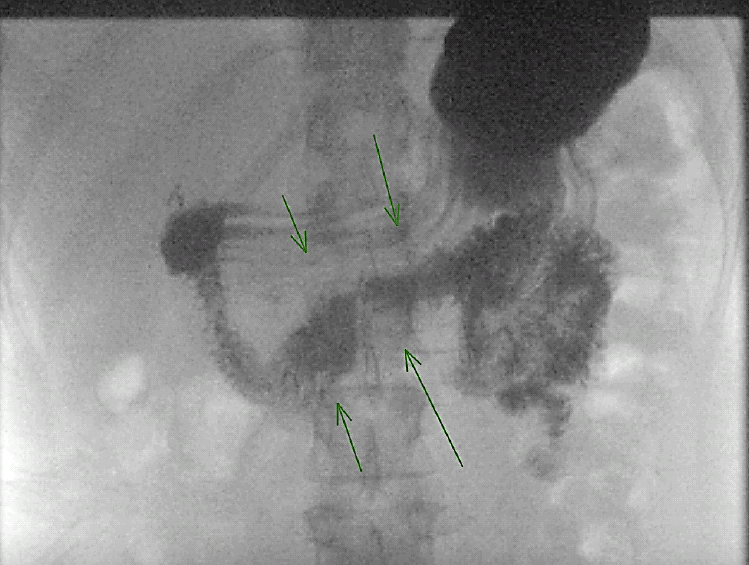
A-34-year-old, female patient, with congenital myasthenia gravis and normal pressure hydrocephalus, had presented postprandial fullness and abdominal distension, accompanied by nausea and weight loss. Abdominal examination was normal, and the work-up showed normal blood tests. Upper gastrointestinal barium study confirmed the extrinsic obstruction of third part of duodenum, with delay in contrast passage (Figure 1).
Figure 1: Filling failure in the third duodenal portion, due to probable extrinsic compression.
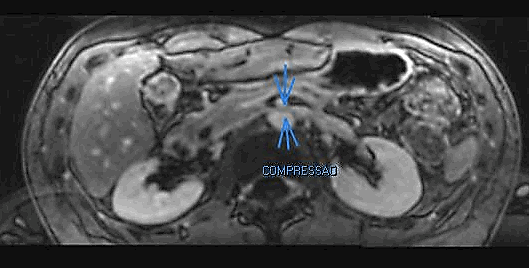
Figure 2: MRI showed a reduced angle between aorta and superior mesenteric artery.
MRI showed a reduced angle between aorta and superior mesenteric artery, measuring 19 degrees, 2 mm distance between the superior mesenteric artery and the aorta (Figure 2). Intraoperatively, a dilated duodenum to the level of D3 was noted. A latero-lateral robotic duodenojejunostomy using 60 mm linear stapler between jejunum and these second portion of the duodenum was performed. Patient recovered with no pain or digestive complaints, accepting liquid diet on the second day after surgery. Robotic surgery herein demonstrated may be considered safe and resolutive, with good visualization of structures, relative short surgical time and fast post-operative recovery.
Discussion
The SMAS is a rare form of intestinal obstruction and is described as compression of the third portion of the duodenum between the angle of the SMA and the aorta, which can lead to acute or insidious symptoms, including epigastric pain, bloating, vomiting, anorexia and weight loss [3, 4]. It occurs mainly due to marked weight loss as consequent of many different diseases, for instance cancer, bariatric surgery, chronic infections, severe burns, etc. It causes reduction in the mesenteric fat tissue surrounding the duodenum and thus shortening the distance and reducing the angle between the SMA and the aorta (38°-65° to 6°-25°). It is this loss of obliquity that results in the compression of the third part of the duodenum as it runs between the superior mesenteric artery and the aorta from right to left [2, 3, 5].
Radiologically, barium meal and CT scan show dilatation of the stomach and proximal duodenum with an abrupt cut-off across its third part, together with a decreased aortomesenteric distance as well as aortomesenteric angle. These findings, in the proper clinical sitting, virtually establish the diagnosis. Thinning out of the fat pad between SMA and aorta, consequently upon weight loss, narrows the aortomesenteric angle and distance, thereby compressing the duodenum and thus producing the clinical manifestations of the syndrome. Other contributory factors include an abnormally low origin of SMA, excessive lumbar lordosis, and hypertrophied or shortened ligament of Treitz or its multiple attachments to the duodenum [5].
The treatment of SMA syndrome is generally conservative and is initially aimed at the correction of hydro electrolytic and metabolic alterations, decompression of the gastrointestinal tract or the placement of a nasogastric tube and recovery of the nutritional state. The use of prokinetics may be effective. Surgical treatment is indicated when either medical treatment fails, or the duodenal dilatation is persistent and progressive [3].
About 50-70% of cases evolve to surgical treatment, consisting of the section of the Treitz ligament (Strong's procedure), duodenojejunal anastomosis (duodenojejunostomy) or gastrojejunal (gastrojejunostomy), being the preferred access by laparoscopy, depending on the experience of the service [3, 4]. Duodenojejunostomy was introduced first in 1910 by Starley. It is the most performed technique, with a success rate of 90%, being chosen by the patient under discussion. Strong's procedure is performed preferably on children and adolescents, but with a lower success rate, and gastrojejunostomy has a higher risk of peptic ulcer [3].
Conclusion
Robotic duodenojejunostomy technique described here, represents a new therapeutic option for the superior mesenteric artery compression syndrome, with the known advantages of minimally invasive surgery. It is a safe and effective procedure, with acceptable surgical time, relatively free of complications and with good patient recovery.
Article Info
Article Type
Case ReportPublication history
Received: Thu 20, Aug 2020Accepted: Mon 31, Aug 2020
Published: Tue 08, Sep 2020
Copyright
© 2023 Vladimir Schraibman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.09.07
Author Info
Vladimir Schraibman Marina Epstein Gabriel Maccapani Franco Milan Sapuppo Marilia Fernandes
Corresponding Author
Vladimir SchraibmanDepartment of General, Gastric and Minimally Invasive Surgery, Albert Einstein Jewish Hospital, São Paulo, Brazil
Figures & Tables
References
- Sara Catarino Santos, Ana Rita Loureiro, Rosa Simão, Jorge Pereira, Luís Filipe Pinheiro et al. (2018) Wilkie's syndrome: a case report of favourable minimally invasive surgery. J Surg Case Rep 2018: rjy027. [Crossref]
- Ali Salem, Labib Al Ozaibi, Suad Mohamed Maher Nassif, Rufaida Abdel Gadir Satti Osman, Nisreen Mohammed Al Abed et al. (2017) Superior mesenteric artery syndrome: A diagnosis to be kept in mind (Case report and literature review). Int J Surg Case Rep 34: 84-86. [Crossref]
- Leandro Cardoso Barchi, Aline Marcílio Alves, Carlos Eduardo Jacob, Claudio José Caldas Bresciani, Osmar Kenji Yagi et al. (2016) Favorable minimal invasive surgery in the treatment of superior mesenteric artery syndrome: Case report. Int J Surg Case Rep 29: 223-226. [Crossref]
- Ramesh Makam, Tulip Chamany, Vamsi Krishna Potluri, Prashanth J Varadaraju, Rajesh Murthy (2008) Laparoscopic management of superior mesenteric artery syndrome: a case report and review of literature. J Minim Access Surg 4: 80-82. [Crossref]
- Yagan Pillay (2016) Superior Mesenteric Artery Syndrome: A Case Report of Two Surgical Options, Duodenal Derotation and Duodenojejunostomy. Case Rep Vasc Med 2016: 8301025. [Crossref]
