Video Assisted Anal Fistula Treatment (VAAFT) for Treating a Complex Posttraumatic Anal Fistula: Case Report
A B S T R A C T
Introduction: Anal fistula is an abnormal pathway that connects the anorectal tract to the perianal skin. The Park’s classification describes four different types of anal fistulas depending on their links with the sphincter apparatus. In this paper, we report an interesting case of post-traumatic complex trans-sphincteric fistula treated with VAAFT procedure.
Case Presentation: A 60-year-old-male patient, from an accidental fall, developed a gluteal abscess with a high trans-sphincteric anal fistula and a secondary tract leading to a large second abscess located in the right ischiorectal fossa. An abscess incision was done, and a draining seton was placed in another Institution. The patient came to our Hospital and underwent surgery using Video Assisted Anal Fistula Treatment (VAAFT) procedure.
Conclusions: VAAFT is an effective and safe procedure for complex anal fistula, even when they have a post-traumatic origin.
Keywords
Case report, gluteal abscess, complex anal fistula, VAAFT procedure
Introduction
An anal fistula is an abnormal tract between the anorectal area and the perianal skin. It represents the chronic manifestation of an acute infection, such as an abscess. Aetiology includes infections, Crohn’s disease, tuberculosis, malignancy and trauma. The incidence is 9 per 100.000 persons per year in the Western populations [1]. The Park’s classification is, still now, the most widely adopted all over the world. Based on the relationships that the fistula acquires with the anal sphincter apparatus, anal fistulas are classified as inter-sphincteric, trans-sphincteric, supra-sphincteric, and extra-sphincteric. They can also be classified as simple or complex. Normally, simple fistulas involve only the internal sphincter (inter-sphincteric) or they have a superficial trans-sphincteric course, meanwhile, complex fistulas are those that traverse more than 30% of the external sphincter, the anterior ones in a female, any fistulas with multiple tracts, recurrent fistulas, and finally, those originated after local irradiation or associated to the Crohn’s disease [2].
Complex fistula is challenging for surgeons because of the risk of faecal incontinence and high rates of recurrence. Classical fistulotomy has a 90% success in uncomplicated inter-sphincteric fistulas with a few postoperative complications, but the risk of faecal incontinence is higher if the fistulotomy is performed in the case of medium or high trans-sphincteric fistulas. Minimally invasive methods, like the anal plug or fibrin glue, are associated with a low incidence of incontinence but a high recurrence rate [3]. We are reporting an interesting case of post-traumatic complex trans-sphincteric fistula treated with VAAFT procedure.
Case Report
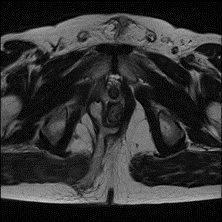
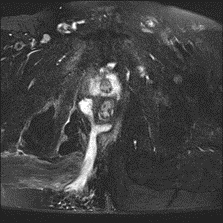
This work has been drawn up according to the SCARE (Surgical Case Report) criteria [4]. A male patient 60 years old, suffering from arterial hypertension and glaucoma, suffered severe trauma on his right gluteus without any fractures. Six months later, as a result of persistent high temperature and severe pain on the right buttock, an ultrasound was performed, which demonstrated the presence of a fluid collection of 4 cm in diameter, 2 cm deepest. Subsequently, an FNA was done which tested positive for methicillin-resistant -haemolytic staphylococcus. Antibiotic therapy with Linezolid was unsuccessfully administered by his General Practitioner. Following the onset of diarrhoea and haematochezia, he underwent colonoscopy which demonstrated an eroded papule in the distal rectum (multiple biopsies were performed on). No other clinical findings were found. Biopsies showed many lymphoplasmacytic and granulocytes infiltrations into the removed mucosal fragments and focal cryptitis. The MR investigation showed a right gluteal abscess and a high trans-sphincteric fistula with two internal orifices, respectively, located at 6 and 9 o’clock close to the dentate line. The main tract (63 mm long and 11 mm thick) was detected toward the right gluteal skin (Figures 1-3).
Figure 1: Right gluteal abscess and a high trans-sphincteric fistula with two internal orifices located at 6 and 9 o’clock close to the dentate line (T2 sequence).
Figure 2: T2 FAT sequence.
Figure 3: T2 FAT coronary scan.
The patient underwent a surgical procedure in another Hospital: an incision and drainage of the abscess were performed and two posterior draining setons were placed. As a result of the persistence of severe pain and purulent leakage from the anus and from the external orifices, the patient decided to turn to us. He was admitted to our Department, and the VAAFT procedure was performed under spinal anaesthesia. The patient was placed in the lithotomic position. The seton was removed and the Meinero’s fistuloscope was introduced through the external openings (VAAFT diagnostic phase- The Fistuloscopy) that were communicating with each other. The main tract was 15 cm long (and not 6,3 cm as showed in MR), starting from the sacrococcygeal area, crossing full thickness the right gluteal muscle, and leading behind the anus canal. The internal opening was located at 6 o’clock on the dentate line.
Figure 4: VAAFT intrafistular fibroscopic view.
No secondary internal opening was found (as described by previous imaging). A secondary tract, which ended in a big abscess cavity in the ischiorectal fossa, was detected. The main tract, the secondary tract and the big abscess cavity were cauterized from inside using a monopolar electrode passing through the operative channel of the fistuloscope, always under fibroscopic vision (VAAFT operative phase) (Figure 4). All the necrotic material was removed by the endo-brush, according to the VAAFT procedure. The internal opening was closed both on the internal muscle and on the mucosa layers by some separate stitches in 2/0 vicryl. No postoperative complications were noticed. The postoperative pain was very low (3 of the VAS scale), and the patient was discharged the same day. We gave him a specific brochure, including precise instructions about the home dressing and the external opening management. The one, three, six months and two-year follow-up does not show any fistula recurrence.
Discussion
Complex anal fistulas are challenging for the surgeon because of the high risk of postoperative complications, in particular deterioration in continence levels and a high percentage of recurrence. The successful key points are the correct identification of the internal opening and the course of the main fistula tract not forgetting any possible secondary tracts or abscess cavities. The complete eradication of these infections and the hermetic closure of the internal opening are also essential, just to prevent the passage of faecal material through the fistula pathway [5]. VAAFT technique is a relatively new procedure developed by Dr. Meinero in 2006. The VAAFT kit includes a fistuloscope (manufactured by Karl Storz SE & Co- Tuttlingen, Germany), an obturator, a unipolar electrode, and an endo-brush. VAAFT is performed under spinal or general anaesthesia, and the patient is placed in the lithotomy position. The technique comprises two phases: diagnostic (also named fistuloscopy) and operative. The fistuloscope is connected to a 3000 ml bag of glycine and mannitol 1% solution, which act as a washing liquid.
The diagnostic phase starts by introducing the fistuloscope through the external opening (s) with a glycine-mannitol 1% solution already running. With slow movements, left-right and up-down, it is possible to understand the fistula “anatomy”, which clearly appears on the screen. The main pathway and any possible secondary tracts or abscess cavities can be detected until the end of the fistula tract, which usually is the internal fistula opening. This is one of the most important VAAFT key points. Two stitches are placed on two opposite points of the internal opening edge because correct identification is essential in the subsequent surgical phase. In the operative phase, the fistula pathway, including any possible secondary tracts or abscess cavities, is always completely destroyed, under fibroscopic control, with the unipolar electrode passing through the fistuloscope. Then, the necrotic material is removed with an endo-brush, always under direct vision. With the aid of an anal retractor, the internal orifice is subsequently sutured. In 15% of cases, a linear stapler can be used after pulling the stitches previously put on the internal opening, but only if the patient never underwent surgical procedure before. Otherwise, because of previous surgeries, the internal opening surrounding tissue can be too fibrous and scarred [6].
Usually, an advancement flap can be done for the closure of the internal orifice or simply by positioning two or three absorbable stitches either on the internal opening or for the mucosal layer. Since 2006, several studies and systematic reviews were published with variable results, anyway, the success rate reported in the literature is between 76 and 86%. The recurrence rate varies depending on the method used for closing the internal opening (the worst seems to be the mucosal-cutaneous flap). Complications, both in the early and late postoperative time, are minimal. In the 5% of cases, they consist of minimal blood loss from the external opening, itching, local cellulitis and pain, which can usually be reduced with painkillers assumption for a few days. Sometimes, some complications can be related to the spinal anaesthesia, like urinary retention or temporary back pain. None of the studies reported any significant continence worsening or sphincter damages. VAAFT is normally performed in day surgery mode. Even in the case of a more complex fistula, the patient’s hospital stay is very short (0/2 days). The return to work is very fast (from 1 to 11 days) [3, 7].
Conclusion
The main feature of VAAFT is the ability to explore the fistula from the inside, always under direct vision. Thanks to this, no false pathways can be created. All secondary tracts or abscess cavities can be found (which is rather difficult for the other techniques), and this represents the key point of the successful treatment of anal fistulas. As the entire operation is performed from inside, no sphincter damages can be caused, and the incontinence rate is null. The patient’s quality of life is far better than traditional techniques. Finally, the wounds on the patient’s buttocks are very small and require a simply daily dressing that the patient can do by himself at home. The relative cost of the VAAFT kit is largely covered by saving days of patient’s hospital stay and the reduced healing time [3].
Even if more detailed studies are needed in order to definitively assess the cost/benefit ratio, it is our opinion that VAAFT is an effective and safe procedure also for complex post-traumatic anal fistula. It should also be considered that we witnessed an important underestimation of the length of the fistula by the MR where a fistula of 6.3 cm was reported which in reality turned out to be 15 cm at the endoscopic evaluation. It is, therefore, necessary to reconsider the real diagnostic reliability of MR which in this case has really shown an underestimation.
Article Info
Article Type
Case ReportPublication history
Received: Sat 21, Nov 2020Accepted: Mon 07, Dec 2020
Published: Wed 30, Dec 2020
Copyright
© 2023 Marco De Monti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.04.05
Author Info
Ferrario Luca Cestaro Giovanni Meinero Piercarlo Fasolini Fabrizio Marco De Monti
Corresponding Author
Marco De MontiEOC - Beata Vergine Regional Hospital, Department of Surgery, Mendrisio, Switzerland
Figures & Tables


References
- Newman PA, Dixon T (2017) Benign anorectal conditions. Surgery 35: 443-450.
- Whiteford MH (2007) Perianal Abscess/Fistula Disease. Clin Colon Rectal Surg 20: 102-109. [Crossref]
- Garg P, Singh P (2017) Video-assisted anal fistula treatment (VAAFT) in cryptoglandular fistula-in-ano: A systematic review and proportional meta-analysis. Int J Surg 46: 85-91. [Crossref]
- Agha RA, Fowler AJ, Saeta A, Barai I, Rajmohan S et al. (2016) The SCARE statement: Consensus-based surgical case report guidelines. Int J Surg 34: 180-186. [Crossref]
- Meinero P, Mori L, Gasloli G (2014) Video-assisted anal fistula treatment: A new concept of treating anal fistulas. Dis Colon Rectum 57: 354-359. [Crossref]
- Meinero P, Mori L (2011) Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Tech Coloproctol 15: 417-422. [Crossref]
- Emile SH, Elfeki H, Shalaby M, Sakr A (2018) A Systematic review and meta-analysis of the efficacy and safety of video-assisted anal fistula treatment (VAAFT). Surg Endosc 32: 2084-2093. [Crossref]
