Journals
Trapped thrombus in patent foramen ovale with pulmonary embolism and homonymous paracentral scotoma
A B S T R A C T
A 37-year-old female presented with persistent dyspnea and syncope. Computed-tomography scan detected saddle pulmonary embolism, and echocardiogram revealed extensive thrombus crossing the interatrial septum and prolapsing across the mitral valve into the left ventricle. Consequently, the patient was treated with surgical extraction of the thrombus and pulmonary embolectomy.
She was discharged after un-eventful hospital stay save a dark grey spot in her central vision, which was diagnosed as homonymous paracentral scotoma caused by pre-operative cerebral infarction.
K E Y W O R D S
Impending paradoxical embolism, pulmonary embolism, homonymous paracentral scotoma
Abbreviations
PFO: patent fossa ovale ,PE: pulmonary embolism , PA: pulmonary artery, LV: left ventricle, CPB: cardiopulmonary bypass, LA: left atrium
Introduction
Trapped thrombus in a patent fossa ovale (PFO), also referred to as thrombus-in-transit or impending paradoxical embolism, is a rare complication of pulmonary embolism (PE) [1].
The reported short-term mortality rate in this scenario ranges from 14% to 21% therefore, urgent triage and treatment is mandatory [1-3]. Treatment options include anti-coagulation therapy, thrombolysis or surgery. Few studies have examined outcomes for each approach; consequently, the best choice has not been settled and is prone to individual assessment [3, 4].
Case Report
A 37-year old female presented to the hospital following an episode of syncope. She reported new and increasing shortness of breath and leg cramps starting 2 weeks prior.
The physical examination was unremarkable except morbid obesity (body mass index; 57 kg/m2). Enhanced CT scan detected saddle PE with extension into bilateral branch pulmonary arteries (PAs). Lower limb Doppler studies revealed near occlusive acute deep vein thrombosis in the right.
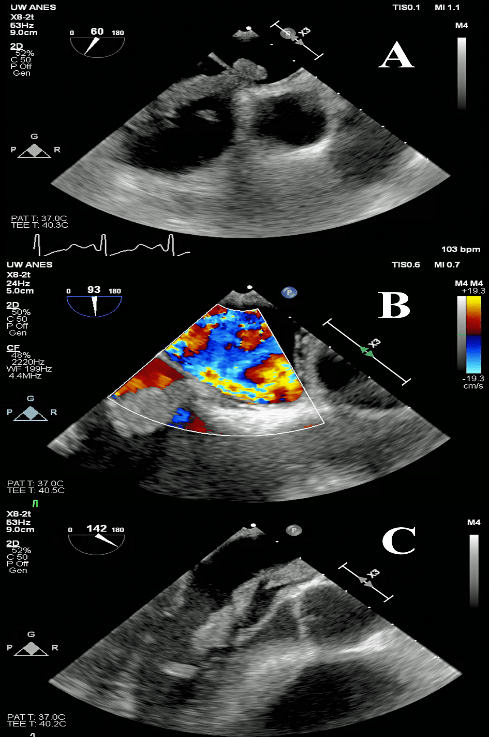
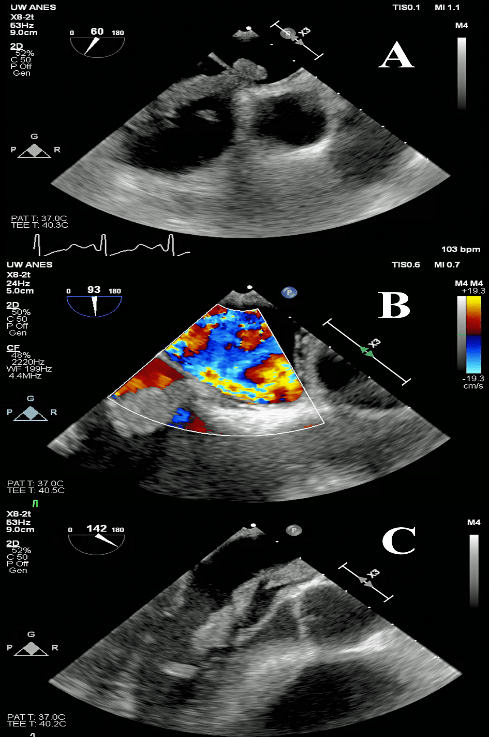
She was hemodynamically stable; however, transthoracic echocardiogram revealed right ventricular strain and 8-cm long mass inside the cardiac cavity. The highly-mobile mass crossed the interatrial septum and prolapsed across the mitral valve into the left ventricle (LV). This was deemed to be a thrombus-in-transit lodged within the atrial septum, with both atrial components (Figure 1). There was no visible flow across the septum by color flow. The patient was urgently operated within 24hrs of diagnosis. Thrombolytic therapy was not pursued as the patient was judged a very reasonable operative candidate.
Procedure and Outcome
The operation was conducted through a median sternotomy, and cardiopulmonary bypass (CPB) was established via a central aortic and bicaval venous cannulation. Cardiac arrest was induced by cold blood cardioplegia, and the right atrium was opened.
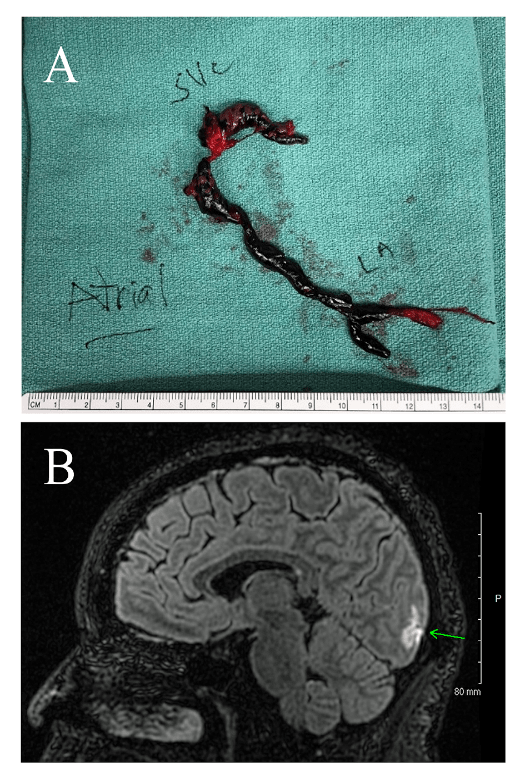
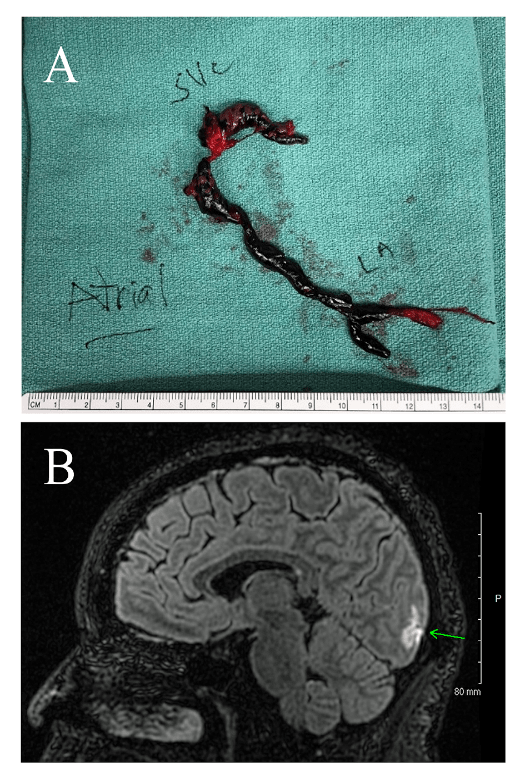
There was a large thrombus extending from the superior vena cava, not from the inferior vena cava, to left atrium (LA) though a PFO. The fossa ovale was incised inferiorly starting just beneath the thrombus allowing carefully removal in one piece (Figure 2A). After removal of intracardiac thrombus, PFO was closed directly. Then the main PA was opened, and a large volume of clot removed from both branch arteries. Embolectomy with a Fogarty catheter was performed to remove distal clots in the lobar arteries. The patient was successfully weaned from CPB on epinephrine at 0.05mcg/kg/min and inhaled nitrous oxide at 40ppm to support right ventricle. Her post-operative course was smooth, and she was discharged on the ninth postoperative day.
Post-operatively she complained of a dark grey spot in her central vision on the right, which she had noticed before admission to the hospital. MRI and examination by an ophthalmologist revealed right homonymous paracentral scotoma, which was attributed to a pre-operative thromboembolic event (Figure 2B). This symptom showed improvement without specific therapy, and at 5 months follow-up her only complaint was related to her vision.
Discussion
In recent systematic reviews of the treatment for thrombus-in-transit In recent systematic reviews of the treatment for thrombus-in-transit [3, 4] the benefits of surgery have been described. Surgical thromboembolectomy and PFO closure significantly reduced composite 30-day and 60-day mortality and systemic embolism; overall mortality at 60-day was 13.9% while the rate for surgery (6.3%) compared favorably to that of thrombolysis (35.7%) and anticoagulation alone (18.5%) [3].
These results are difficult to generalize given the rarity of this clinical scenario as well as a wide range of patient comorbidity; therefore, best treatment for individual patients should be made via thorough discussion including all specialties potentially involved. Decisions must be made quickly however, as the mortality following systemic embolization of a thrombus-in-transit is high, and two-thirds of these patients die within the initial 24hrs following diagnosis [4].
Funding statement and Conflict of interest statement
None.
Article Info
Article Type
Case ReportArticle History
Received Date: 5 October, 2018Accepted Date: 23 October, 2018
Published 14 November 2018
Copyright
© 2018 Kosuke Ujihira. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.03.011
Author Info
Corresponding author
Kosuke Ujihira, Division of Cardio-thoracic surgery, Department of Surgery University of Wisconsin School of Medicine and Public Health, 600 High Land Avenue, Madison, WI 53792, USA;
Figures & Tables