Journals
Total Cyst Excision of Type I Choledochal Cyst 2 Years After Roux-en-Y Hepatocholangiojejunostomy: Report of a Case
A B S T R A C T
Background: Choledochal cysts are rare congenital or acquired cystic dilation of the intra- or extrahepatic bile ducts. It is well known that choledochal cyst is a precancerous lesion and cancer usually occurs at the site of bile stasis, irritation, and inflammation. Case presentation: We present a rare case of cyst excision of type I choledochal cysts after Roux-en-Y Hepatocholangiojejunostomy about two years ago. A 17-years-old girl visited our hospital complaining of transient epigastric pain. History study revealed that she had undergone Roux-en-Y Hepatocholangiojejunostomy for cholecochal cyst (type I) without cyst excision 2 years ago in local hospital because of severe adhesion of the cyst to the portal vein and pancreas. In our department,the patient underwent total cyst excision and postoperative pathological study revealed fibrous wall tissue, confirming the diagnosis of choledochal cyst. The patient has no recurrence to date and has recovered well. Conclusion: This case shows that proper surgical management is necessary for patients with congenital choledochal cyst.
K E Y W O R D S
Total cyst excision, type I choledochal cysts, Roux-en-Y, Hepatocholangiojejunostomy
Background
Choledochal cysts are rare congenital or acquired cystic dilation of the intra- or extrahepatic bile ducts [1]. It is a relatively rare disease that the incidence of this pathology in Asian populations is 1:1000 and it is lower in western countries (1:100 000 to 1:150 000) [2-3]. It is well known that choledochal cyst is a precancerous lesion and cancer usually occurs at the site of bile stasis, irritation, and inflammation [4-5]. The incidence of cancer in patients with primary choledochal cyst is 9.9%, whereas the incidence of cancer development after cyst excision is only 0.6% indicating the necessity of cyst excision [6]. Herein, we present a case who complained of abdominal pain after Roux-en-Y hepatocholangiojejunostomy without cyst excision. We resected the total cyst to prevent cancer occurrence and relieve the abdominal pain of the patient.
Case Presentation
A 17-year-old girl visited our hospital complaining of right upper quadrant abdominal pain lasting for 1 week. The pain was constant and was not associated with nausea, constipation, or diarrhea. Two years ago, in local hospital, the patient had undergone Roux-en-Y hepatocholangiojejunostomy without choledochal cyst excision due to severe adhesion of the cyst to the portal vein and pancrease. The patient had no history of diabetes mellitus, hyperlipidemia, and hypertension. She did not take any medications. Physical examination showed the body temperature was 36.8°C with pulse 65 beats/min. The respiration rate was 18/min and blood pressure were 99/64 mm Hg. The patient was uncomfortable but not in acute distress. She did not look so sick, with no sclera icterus or jaundice. Bowel sound was normal, and there was neither tenderness nor muscle rigidity. Initial laboratory findings including white blood cell count, hemoglobin, platelet count, total bilirubin, aspartate transaminase, alanine transaminase, alkaline phosphatase was normal. Ultrasound of the abdomen reveled a hilar cystic mass of 7.4 cm×6.8 cm, with clear margin, containing liquid with multiple mobile echo groups (stone formation) (Figure 1). Magnetic resonance cholangiopancreaticography (MRCP) showed slight dilatation of the hilar bile duct and a large, cystic, mass-like lesion of 7.3 cm×5.3 cm in size with stone formation . Compression of the cyst to the pancreas head without pancreatic duct dilation was also found. (Figure 2)
Operation was scheduled for total cyst excision. After general anesthesia, an incision was made via the previous upper right quadrant scar. Underneath the scar, there was a severe adhesion so adhesiolysis was performed. Abdominal exploration revealed that the Roux-en-Y hepatocholangiojejunostomy was in retrocolic state. After retraction of the bile drainage loop and descending part of the duodenum,a huge choledochocyst with multiple nourish blood vessels was exposed(Figure 3 A and B). Kocher maneuver was performed to further expose the cyst. Cyst fluid was aspirated for amylase analysis with high level 627U/L,indicating the existence of pancreatiobiliary reflux. Further exposure showed that the proximal stump of the cyst is left as a blind end under the hepatic hilum and the distant end of the cyst had grew into pancreas head. Transverse Incision Technique was used to resect the cyst. A transverse incision was made on the anterior wall and we found the stones in the cyst just as the reported of ultrasound and MRCP (Figure 3 C). The transverse incision over the anterior wall was enlarged toward the left and behind in order to dissect the medial and posterior cyst wall from the hepatic artery and portal vein. Then the proximal edge of the posterior wall were retracted upward to aid in the dissection of the proximal parts of the cyst. For the distal end of the cyst, there was severe adhesion with pancreas and portal vein, injury to the portal vein and pancreas is possible if attempts are made to remove the entire posterior wall of the cyst especially because adhesions have formed between this wall and the portal vein and pancreas, so Lilly Technique was used, anterolateral part of the cyst can be resected and then resection or fulguration of the mucosal lining can follow, leaving a narrow rim of the posterior cyst wall on the portal vein and pancreas. At last, sutured bleed point using no damaging sutures because the wound was too easy to bleed.
Histological findings revealed fibrous wall tissue, confirming the diagnosis of choledochal cyst devoid of malignancy with stone formation (Figure 4).
Figures
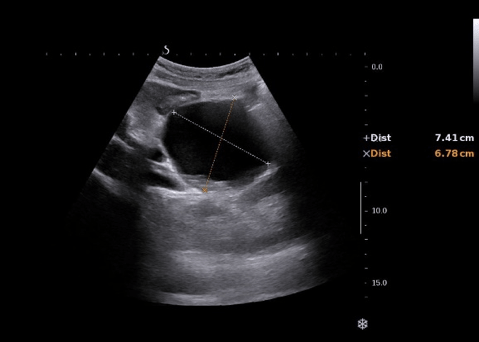
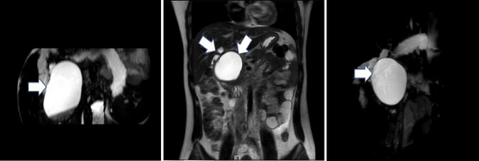
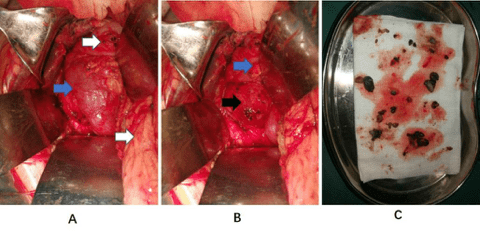
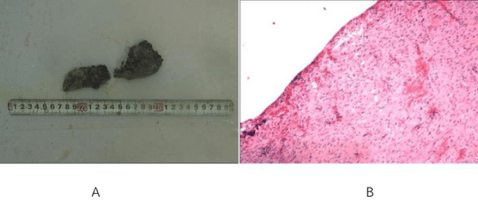
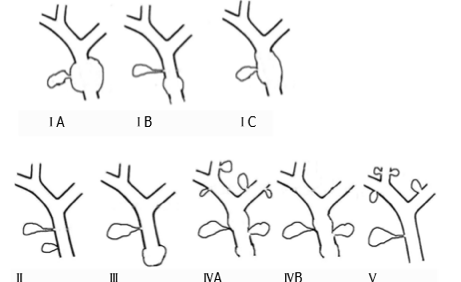
Figure legends
Fig. 1: Ultrasound :Hilar cystic mass of 7.4 cm×6.8 cm, with clear margin, containing liquid with multiple mobile echo groups.
Fig. 2: (MRCP) showed little dilatation of the hilar bile duct and a large, cystic, mass-like lesion of 7.3 cm×5.3 cm in size with stone formation . There was also compression of the pancreas head without pancreatic duct dilation.
Fig. 3: blue arrows : duodenum; white arrows : bile drainage loop ; black arrow: the huge cyst .A: After retraction of the bile drainage loop, the duodenum could be seen B: After retraction of the duodenum, we found the huge cyst with multiple nourish blood vessels. C: The stones in the cyst just as the reports of ultrasound and MRCP.
Fig. 4: A: Gross specimen after resection. B: Histological findings: fibrous wall tissue, no lining epithelium from the resected tissue.
Fig. 5: Types of biliary cysts according to Todni classification.
Discussion
The classical triad of jaundice, right upper quadrant mass, and abdominal pain is present in only a minority of choledochal cyst patients (0–17 %) [7]. It is more commonly seen in children than in adults, and 85 % of children have at least two features of the triad at presentation, compared with only 25 % in adults [8]. Other presenting features of choledochal cysts are cholangitis, pancreatitis, and biliary peritonitis from cyst rupture. For this case, the presentation is abdominal pain without jaundice or right upper quadrant mass.
Alonso-Lej et al. published the first systematic description of choledochal cysts, based on the clinical and anatomic findings in 96 cases in 1959 [9]. They classified choledochal cysts into three types and described the therapeutic strategies for each type. This classification was further refined by Todani and colleagues who included five major types and several subtypes [10]. (Figure 5) Type I cysts are a dilatation of the extrahepatic bile duct. These are the most common type and seen in 75–85 % cases 9. Type I cysts may be further classified as cystic (IA), focal (IB), or fusiform (IC). Type II cysts are diverticulum of the common bile duct. Type III cysts are represented by a cystic dilatation of the intramural portion of the common bile duct known as choledochoceles. Type IVA lesions involve both the intraand extrahepatic portions of the bile ducts, and type IVB lesions are multiple cysts limited to the extrahepatic bile ducts. Type IV-A cysts are the second most common type after type I. Type V cysts synonymous with Caroli disease describe the abnormalities of the intrahepatic bile ducts。For this case,the cyst belong to type I.
The surgical management of choledochal cysts is based on the cyst type and associated hepatobiliary pathology. In general, all bile duct cysts should be excised and bile flow is re-established by mucosa-to-mucosa anastomosis [11]. The treatment of choice of type I bile duct cysts (for this case)in adults is total cystectomy and Roux-en-Y hepatocholangiojejunostomy. The advantages of this procedure include a reduced incidence of anastomotic strictures, stone formation, cholangitis, and intra-cystic malignancy. In this girl, the cause of abdominal pain was that the previous operation was neither standard nor completed. So, it is necessary to complete the standard management with total cystectomy.
Choledochal cyst is rare disease but has a clinical importance because of high incidence of biliary tract cancer, even in an asymptomatic case. The overall risk of cancer has been reported to be 10% to 15% [12]. The importance of complete cyst excision is commonly understood to prevent the development of malignancies and other complications [13]. In one Japanese study, approximately 1% of cases developed to cholangiocarcinoma which was mainly originated from incomplete excision. So, in this case, we tried our best to resect the cyst despite the difficulty and danger.
Three methods for resection of the Choledochal Cyst are common used as we have mentioned in the literature [14]. Distal-End-First Resection Technique is often used in the case of a medium size or small cyst. Transverse Incision Technique is adopted when the cyst is too large. Some patients suffered from recurrent attacks of cholangitis. In these cases, injury to the portal vein is possible if attempts are made to remove the entire posterior wall of the cyst especially when adhesions have formed between this wall and the portal vein, for these cases, Lilly Technique is suitable [14]. For this girl, the cyst is large and there are adhesions between the cyst and portal vein and pancreas, so both Distal-End-First Resection Technique and Lilly Technique were used.
Conclusion
Choledochal cyst is rare disease but has a clinical importance because of high incidence of biliary tract cancer, even in an asymptomatic case. The importance of complete cyst excision is commonly understood to prevent the development of malignancies and other complications. This case shows that proper surgical management is necessary for patients with congenital choledochal cyst.
Funding
None
Authors’ Contributions
Gangshan Liu participate the surgery and wrote the initial draft of the manuscript. Ying Fan performed the surgery and correct the writing of the manuscript. Tianyu Li and Luxin Sun participate the surgery.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
Informed consent was obtained from the patient for the publication of this case report and any accompanying figures.
Competing Interest
The authors declare that they have no competing interests
Article Info
Article Type
Case ReportPublication history
Received 20 March, 2018Accepted 4 April, 2018
Published 11 April, 2018
Copyright
© 2018 Ying Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.10.001
Author Info
Corresponding author
Ying FanDepartment of The Second General Surgery, Shengjing Hospital of China Medical University
Figures & Tables
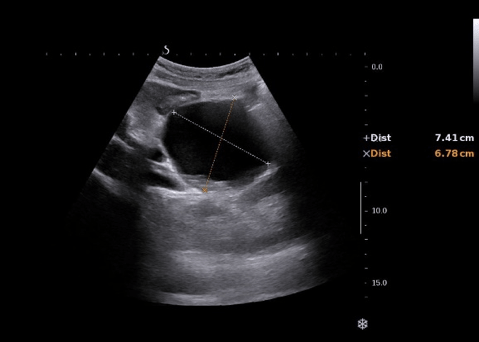
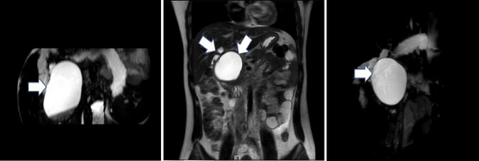
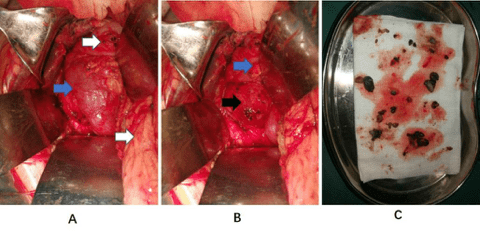
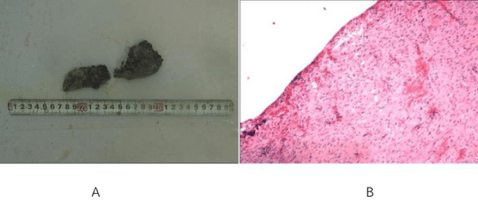
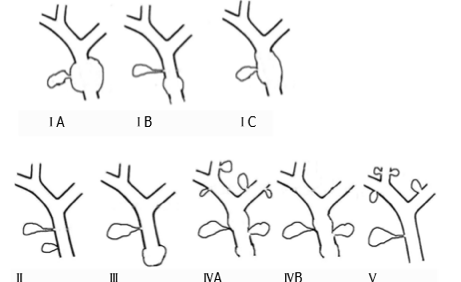
Figure legends
Fig. 1: Ultrasound :Hilar cystic mass of 7.4 cm×6.8 cm, with clear margin, containing liquid with multiple mobile echo groups.
Fig. 2: (MRCP) showed little dilatation of the hilar bile duct and a large, cystic, mass-like lesion of 7.3 cm×5.3 cm in size with stone formation . There was also compression of the pancreas head without pancreatic duct dilation.
Fig. 3: blue arrows : duodenum; white arrows : bile drainage loop ; black arrow: the huge cyst .A: After retraction of the bile drainage loop, the duodenum could be seen B: After retraction of the duodenum, we found the huge cyst with multiple nourish blood vessels. C: The stones in the cyst just as the reports of ultrasound and MRCP.
Fig. 4: A: Gross specimen after resection. B: Histological findings: fibrous wall tissue, no lining epithelium from the resected tissue.
Fig. 5: Types of biliary cysts according to Todni classification.
References
1. De Wilde VG, Elewaut AG, De Vos MM, Hendrix RF, Barbier FE (1991) Choledochal cysts in the adult. Endoscopy 23: 4-7.
2. Kim SH, Kim HW, Kang DH, Kim MD, Lee JH, et al. (2012) A case of intrahepatic cholangiocarcinoma associated with type iv choledochal cyst. Korean J Gastroenterol 60: 123-127. [Crossref]
3. Franko J, Nussbaum ML, Morris JB (2006) Choledochal cyst cholangiocarcinoma arising from adenoma: case report and a review of the literature. Curr Surg 63: 281-284. [Crossref]
4. Tsuchiya R, Harada N, Ito T, Furukawa M, Yoshihiro I (1977) Malignant tumors in choledochal cysts. Ann Surg 186: 22-28. [Crossref]
5. Todani T, Watanabe Y, Fujii T, et al (1985) Carcinoma arising from the bile duct in choledochal cyst and anomalous arrangement of the pancreaticobiliary ductal union. 6: 525-535.
6. Lee SE, Jang JY, Lee YJ, Choi DW, Lee WJ, et al (2011) Choledochal cyst and associated malignant tumors in adults: a multicenter survey in South Korea. Arch Surg 146: 1178-1184. [Crossref]
7. Sherman P, Kolster E, Davies C, Stringer D, Weber J (1986) Choledochal cysts: heterogeneity of clinical presentation. J Pediatr Gastroenterol Nutr 5: 867-872.
8. Lipsett PA, Pitt HA, Colombani PM, Boitnott JK, Cameron JL (1994) Choledochal cyst disease: a changing pattern of presentation. Ann Surg 220 :644-652. [Crossref]
9. Alonso-Lej F, Rever WB Jr, Pessagno DJ (1995) Congenital choledochal cysts, with a report of 2, and an analysis of 94 cases. Surg Gynecol Obstet 108: 1-30.
10. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K (1977) Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 134: 263-269. [Crossref]
11. Chiranjiv Khandelwal, Utpal Anand, Bindey Kumar, Rajeev N. Priyadarshi (2012) Diagnosis and Management of Choledochal Cyst. Indian J Surg 74: 401-406. [Crossref]
12. Okada A, Hasegawa T, Oguchi Y, Nakamura T (2002) Recent advances in pathophysiology and surgical treatment of congenital dilatation of the bile duct. J Hepatobiliary Pancreat Surg 9: 342-351.
13. Singham J, Yoshida EM, Scudamore CH (2010) Choledochal cysts. Part 3 of 3: management. Can J Surg 53: 51-56. [Crossref]
14. Yu Tian, Shuo-Dong Wu, An-Dong Zhu, De-Xing Chen (2010) Management of Type I Choledochal Cyst in Adult: Totally Laparoscopic Resection and Roux-en-Y Hepaticoenterostomy. J Gastrointest Surg 14: 1381-1388. [Crossref]
