Therapeutic Breast Reduction in Upper Quadrant Breast Tumor
A B S T R A C T
Introduction: Breast conserving surgery plus radiation therapy and mastectomy procedures has equal results in terms of survival. Oncoplastic surgery principles along with breast reduction techniques allow for very good aesthetic results in immediate breast reconstruction with local tissues in several well-defined clinical scenarios. Nevertheless, we still find several limitations to their use regarding the location of the tumor or the need for inconvenient skin resections out of the standard markings of breast reduction. We present a case where traditional breast reduction techniques were inadequate and technical modifications of standard markings and pedicle design were developed to avoid the need to undergo a mastectomy.
Methods: We present a patient diagnosed with breast cancer where the clinical characteristics of the tumor (location, skin excision needed) precluded the use of traditional oncoplastic breast reduction techniques. Modifications to the traditional breast reduction techniques were used to cope with the oncological resections needed.
Results: A good global symmetry and aesthetic result were achieved. Scar pattern obtained was considered relatively camouflaged and patient satisfaction was high.
Conclusion: Breast reduction procedures can be the solution for the treatment of breast cancer. The location of the tumor in the superior quadrants outside standard markings and the need to include skin in the tumor resection can be sidetracked by using enlarged NAC pedicles with modifications to classic skin markings without compromising oncologic safety. The final aesthetic results obtained are considered very good and the patient is very satisfied.
Keywords
Breast cancer, therapeutic breast reduction mammaplasty, oncoplastic surgery
Introduction
About one hundred years after Halsted’s mastectomy, the first papers on the use of reduction mammoplasty techniques after excision of benign lesions, to promote complete excision while maintaining natural breast contour, were written [1, 2]. From here to its adaptation to breast cancer scenario was a short step. Current oncoplastic surgery combines oncologic principles with plastic surgery techniques enhancing cosmetic outcomes. The reconstruction must guarantee tumor excision, correction or reconstruction of tissue defect and symmetrisation of contralateral breast [3-5]. The possibility of performing tumorectomies followed by radiation therapy without compromising oncologic safety has allowed women to maintain their breasts and spare them the psychological, physical and social burden of having to undergo a mastectomy [6-9].
Criticism to oncoplastic surgery suggested that oncological results were being postponed for cosmetic outcomes, and that it was difficult to determine the re-excision site in a positive margin examination. Giacalone proved that oncoplastic procedures promoted bigger specimen, wider margins, and decreased need of re-excision, not compromising oncological treatment [4].
The role of breast reduction techniques in breast cancer surgery is now well established but still evolving. The multitude and versatility of the techniques described, namely regarding pedicle options and excisional skin pattern designs, allows for its application in several case scenarios [9, 10]. Nevertheless, we still find several limitations to their use in the literature regarding the location of the tumor or the need for skin resection if it didn’t fall within the standard markings of breast reduction (inverted T or vertical scar techniques) [6, 11-14]. We present in this article a case where traditional breast reduction techniques were inadequate and specific technical modifications of standard markings or pedicle design that were developed to avoid the need to undergo a mastectomy procedure.
Materials and Methods
We present a patient treated at our institution that was diagnosed with breast cancer and considered eligible for breast conserving surgery in the oncology board meeting. Classic indications for this included unifocal disease, small tumor mass, generous remaining breast volume after extirpation and the patient’s desire [5, 8-10]. In our practice, the preferred method for breast conserving surgery is the use of breast reduction techniques, due to their versatility and possibility of adaptation to various scenarios [15]. Classic indications for therapeutic breast reduction procedures comprise large breasts (C-cup or larger), the location of the tumor to be preferably in the lower quadrants and the need not to excise skin outside the borders of breast reduction patterns (inverted T or vertical scar) [8, 11, 12]. However, regardless of these indications, in this case the authors create a modification to the standard techniques allowing to still be treated in a conservative way.
The case we present is about a 42-year-old woman with a third-degree ductal carcinoma, in the Bloom and Richardson scale. The tumor was located in the central part of the upper pole of the left breast, directly above the NAC, and was in close proximity to the skin so that breast surgeons had to excise it with margins. Skin marks were drawn on the patient before surgery, allowing for a correct pre-surgical planning, in the presence of both plastic and breast surgeons. This multidisciplinary approach allowed for breast surgeons to use the breast reduction pattern markings to access the tumor, simultaneously obtaining wider resection margins and easier access if necessary. The tumorectomy local and the resulting skin defect was too high for the new NAC position to close the wound without compromising the aesthetic result.
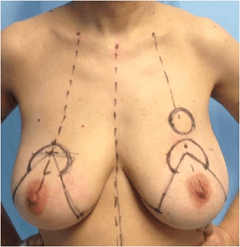
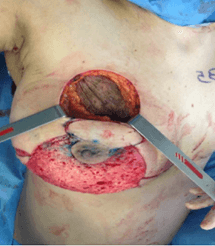
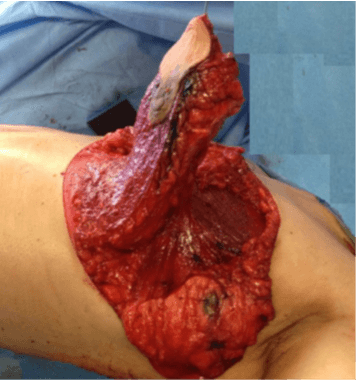
A plan was designed to modify an inferior-based dermoglandular pedicle so that the portion of skin above the original NAC position and below the tumor resection site was preserved. An inferior-based inverted T breast reduction technique was also used in the contralateral breast at the same surgical time as to obtain symmetry (Figures 1, 2 & 3).
Figure 1: Pre-operative skin markings.
Figure 2: After tumor resection in the upper pole.
Figure 3: The large inferior pedicle with dermoglandular extension above the NAC.
Results
A good global symmetry and aesthetic result where achieved, despite an uncommon scar above the new NAC and overall, very good cosmetic result was obtained (Figures 4 & 5). No complications were reported with this modified technique and the pedicle maintained a good vascularization.
Figure 4: One-year post-operative frontal view.
Figure 5: One-year post-operative lateral view.
Discussion
Breast conservative surgery followed by radiation therapy have breast cancer cure rates similar to mastectomy. In large breasts, the remainder parenchyma after tumorectomy can be used to rearrange breast shape in a natural and pleasing way. In our current practice we thereby defend such approach whenever possible. Also, undergoing breast symmetrization procedures in the same surgery allows women to maintain a good image of themselves, avoids postural cervicalgia and spares them the burden of having to be submitted to another operation. Reconstructing breast shape and function in the same surgery when the oncological disease is being treated is our preference. Such approach avoids the burden of dealing with an image of breast amputation which has been proved essential to the woman’s emotional and psychological well-being. Classic markings to perform breast reduction procedures (inverted T pattern, vertical scar pattern) can be used so that breast surgeons can access tumor location and perform tumor excision. When tumor is located in the upper pole: standard inferior NAC pedicles or modified inferior NAC pedicles (inferolateral pedicle, inferomedial pedicle) can be used to cover the defect after tumorectomy.
Sometimes tumor location falls outside the standard markings used in classic reduction techniques and is too close to the skin so that it also needs to be removed with the surgical specimen. We defend that even in such situations, breast reduction procedures can still be performed. Standard breast reduction markings can be modified so as to incorporate the skin that needs to be removed and pre-operative planning can be used to recruit additional skin from other sources to fill in the gap after tumorectomy. A surgical team experienced in breast conservative surgery and reconstruction is a key element in evaluating each case to determine the best course of action.
Conclusion
Breast reduction procedures can be the solution for the treatment of breast cancer. The location of the tumor in the superior quadrants or outside standard markings or even the need to include skin in the tumor resection can be sidetracked by using enlarged NAC pedicles with modifications to classic skin markings without compromising oncologic safety. The final aesthetic results obtained are considered very good and the patient was very satisfied.
In our opinion, it’s not breast volume, tumor location or even the need for skin resection that can predict the possibility of using therapeutic breast reduction procedures. One must evaluate each case individually and determine this possibility alongside team members and the patient’s desire.
Conflicts of Interest
None.
Ethical Approval
This study has been approved by the appropriate ethics committee and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent
All Patients gave their informed consent prior to their inclusion in this study.
Article Info
Article Type
Case ReportPublication history
Received: Tue 31, Aug 2021Accepted: Wed 15, Sep 2021
Published: Fri 29, Oct 2021
Copyright
© 2023 Augusta Cardoso. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.10.01
Author Info
Augusta Cardoso Gustavo Coelho Joana Esteves Horacio Costa
Corresponding Author
Augusta CardosoPlastic, Reconstructive Craniomaxillofacial and Microsurgery Unit, Centro Hospitalar de Vila Nova de Gaia, Portugal
Figures & Tables


References
1. Veronesi U, Cascinelli N, Mariani L, Greco M, Saccozzi R et al. (2002) Twenty-year
follow-up of a randomized study comparing breast-conserving surgery with
radical mastectomy for early breast cancer. N Engl J Med 347: 1227-1232.
[Crossref]
2. Kaviani A, Sodagari N, Sheikhbahaei S, Eslami V, Nejad NH et al. (2013) From radical
mastectomy to breast-conserving therapy and oncoplastic breast surgery: a
narrative review comparing oncological result, cosmetic outcome, quality of
life, and health economy. ISRN Oncol 2013: 742462. [Crossref]
3. Heil J, Gondos A,
Rauch G, Marmé F, Rom J et al. (2012) Outcome analysis of patients with primary
breast cancer initially treated at a certified academic breast unit. Breast
21: 303-308. [Crossref]
4. Giacalone PL, Roger P, Dubon O, El Gareh N, Daures JP et al. (2006) Lumpectomy
vs oncoplastic surgery for breast-conserving therapy of cancer. A prospective
study about 99 patients. Ann Chir 131: 256-261. [Crossref]
5. Hamdi M (2013)
Oncoplastic and reconstructive surgery of the breast. Breast 22:
S100-S105. [Crossref]
6. Botteri E, Bagnardi V, Rotmensz N, Gentilini O, Disalvatore D et al. (2010) Analysis of
local and regional recurrences in breast cancer after conservative surgery. Ann
Oncol 21: 723-728. [Crossref]
7. Pusic A, Thompson
TA, Kerrigan CL, Sargeant R, Slezak S et al. (1999) Surgical options for the
early-stage breast cancer: factors associated with patient choice and
postoperative quality of life. Plast Reconstr Surg 104: 1325-1333. [Crossref]
8. Losken A, Styblo
TM, Carlson GW, Jones GE, Amerson BJ (2007) Management algorithm and outcome
evaluation of partial mastectomy defects treated using reduction or mastopexy
techniques. Ann Plast Surg 59: 235-242. [Crossref]
9. Crown A, Handy N,
Rocha FG, Grumley JW (2018) Oncoplastic reduction mammaplasty, an effective and
safe method of breast conservation. Am J Surg 215: 910-915. [Crossref]
10. Losken A, Hart AM,
Chatterjee A (2017) Updated Evidence on the Oncoplastic Approach to Breast
Conservation Therapy. Plast Reconstr Surg 140: 14S-22S. [Crossref]
11. Munhoz AM, Montag E, Arruda EG, Aldrighi C, Gemperli R et al. (2006) Critical
analysis of reduction mammaplasty techniques in combination with conservative
breast surgery for early breast cancer treatment. Plast Reconstr Surg
117: 1091-1107. [Crossref]
12. Munhoz AM, Aldrighi
CM, Ferreira MC (2007) Paradigms in oncoplastic breast surgery: a careful
assessment of the oncological need and esthetic objective. Breast J 13:
326-327. [Crossref]
13. Veronesi U, Salvadori B, Luini A, Greco M, Saccozzi R et al. (1995) Breast
conservation is a safe method in patients with small cancer of the breast.
Long-term results of three randomised trials on 1,973 patients. Eur J Cancer
31A: 1574-1579. [Crossref]
14. Kosasih S, Tayeh S, Mokbel K et al. (2020) Is oncoplastic breast conserving surgery oncologically safe? A meta-analysis of 18,103 patients. Am J Surg 220: 385-392. [Crossref]
15. Andresen C, Cardoso A, Cunha C, Morais J, Coelho G et al. (2019) Therapeutic breast reduction are doctors and patients satisfied? Eur J Plast Surg 42: 251-258.
