The Significance of Inflammatory Markers in the Prognosis of Newly Diagnosed Multiple Myeloma Patients
A B S T R A C T
Objective: To explore the significance of the ratio of neutrophils to lymphocytes (NLR), monocytes to lymphocytes (MLR), and platelets to lymphocytes (PLR) in the prognosis of patients with newly diagnosed multiple myeloma.
Methods: A total of 60 patients with MM who were diagnosed in Jiangning Hospital Affiliated to Nanjing Medical University and Zhongda Hospital Affiliated to Southeast University from August 2011 to March 2020 were retrospectively analysed. According to NLR, MLR, PLR, the patients were divided into the low NLR group (NLR < 3.61) or high NLR group (NLR ≥ 3.61), low MLR group (MLR < 0.33) or high MLR group (MLR ≥ 0.33), low PLR group (PLR < 129.78) and high PLR group (PLR ≥ 129.78). Overall survival (OS) was used as the prognostic evaluation criteria, and Kaplan-Meier survival curve, Log-rank test and Cox regression model were used to carry out univariate and multivariate analysis on clinical and laboratory parameters.
Results: Among the 60 patients, 33 were male and 27 were female, the median age of the patients was 65 years old, 19 were in the high NLR group, 41 were in the low NLR group, 24 were in the high MLR group, 36 were in the low MLR group, 26 were in the high PLR group, and 34 were in the low PLR group. The univariate analysis showed the prognosis was influenced by factors including NLR, PLR, age, ISS stages, hemoglobin (HGB), albumin (ALT). MLR, type of immunoglobulin, white globulin ratio (A/G), gender, β2-microglobulin(β2-MG), lactate dehydrogenase (LDH) and creatinine were not correlated with the total survival time of patients. The multivariate analysis showed that ISS III stages, PLR ≥ 129.78, HGB < 100g/L were independent risk factors influencing the prognosis of MM patients.
Conclusion: ISS III stages, PLR ≥ 129.78, HGB < 100g/L are independent prognostic risk factors in newly diagnosed multiple myeloma patients, which can be used as an economical and effective method for early evaluation of patient prognosis.
Keywords
Multiple myeloma, overall survival, NLR, PLR, MLR
Introduction
Multiple myeloma (MM) is a malignant clonal disease originating from the plasma cell system, which is still incurable at present, and the prognosis of different patients varies greatly. Traditionally, the prognosis in MM is presented as the stage at the time of diagnosis, but clinical progress of myeloma patients and their survival apparently vary. It is noted that the occurrence of tumors is the result of multi-factor and multi-link interactions, and systemic inflammation can promote tumor occurrence and participate in all stages of tumor development [1]. Tumor-related inflammation can be indirectly manifested as changes in complete blood count (CBC). It has been noted that the ratio of neutrophils to lymphocytes (NLR), monocytes to lymphocytes (MLR), and platelets to lymphocytes (PLR) can be used as predictors of survival for many types of cancer [2-4]. However, there are few studies on the prognostic value of NLR, MLR, PLR and other inflammatory markers for newly diagnosed multiple myeloma, and the existing research results are not uniform. Up to now, inflammatory markers have not been confirmed as the prognostic indicators of MM. In this study, we retrospectively analysed NLR, MLR, PLR, and other clinical and laboratory indicators of newly diagnosed multiple myeloma patients, analysed their relationship with overall survival, and discussed the value of inflammatory markers in the prognosis of multiple myeloma patients.
Materials and Methods
I Selection Criteria
All patients were diagnosed in accordance with the 2014 International Myeloma Working Group (IMWG) diagnostic criteria [5]. All are newly diagnosed patients with multiple myeloma, and the following conditions need to be ruled out. 1) Asymptomatic MM patients; 2) Patients with monoclonal immunoglobulinemia (MGUS) of undetermined significance; 3) MM patients treated previously; 4) MM patients during pregnancy; 5) MM patients with mental illness; 6) MM patients with acute and chronic infection; 7) MM patients who have recently taken antibiotics or cytotoxic drugs; 8) MM patients taking steroids before starting first-line treatment; 9) MM patients with other haematological disorders; 10) MM patients with autoimmune diseases.
II Research Objects
We performed a retrospective research of 60 newly diagnosed MM patients between August 2011 to March 2020 in Jiangning Hospital Affiliated to Nanjing Medical University and Zhongda Hospital Affiliated to Southeast University. All of the patients were confirmed by pathological histology and laboratory examination and classification: IgG type 34 cases (56.7%), IgA type 9 cases (15%), light chains type 11 cases (18.3%), IgD type 4 cases (6.7%), no secretory type 2 cases (3.3%); the International Staging System (ISS): There were 4 cases (6.7%) in stage I, 19 cases (31.7%) stage II, and 37 cases (61.7%) in stage III.
III Study Design
The trained hematologist will consult the data of the patients meeting the enrollment time and criteria, fill in the designed form, and record the age of onset, gender, admission time, disease stage, classification, laboratory examination and treatment plan of the patients. We follow up with patients until May 26, 2020. Overall survival (OS) was defined as the period between the date of diagnosis and the date of death from any cause or the month of last follow-up. The OS of the death of patients with follow-up is the time of death.
IV Observation Indexes
The gender, age, ISS stage, type of immunoglobulin, ALT, A/G, HGB, creatinine, β2-MG, LDH, absolute value of neutrophil, absolute value of lymphocyte, absolute value of platelet, and NLR, MLR, PLR were recorded. According to the average NLR, MLR and PLR values of the enrolled patients as the critical points, MM patients were divided into low NLR group (NLR < 3.61) and high NLR group (NLR ≥ 3.61), low MLR group (MLR < 0.33) and high MLR group (MLR ≥ 0.33), and low PLR group (PLR < 129.78) and high PLR group (PLR ≥ 129.78). The differences in total survival time among groups were analysed.
V Statistical Analysis
We built the database covering the information of all the cases included. Statistical analysis was performed by SPSS 22.0 statistical software. Demographic and descriptive characteristics were summarized using descriptive statistics. Retrospective research and analysis methods were used; descriptive statistical methods were used for the clinical characteristics of newly diagnosed cases. The independent t-test as appropriate was used for comparison between groups, and Kaplan-Meier method was used for survival analysis, and the Log-rank method was used for testing, the Cox regression analysis equation is used for multivariate analysis, and P<0.05 indicates that the difference is statistically significant.
Results
I Clinical Characteristics of the Patients
Among the 60 MM patients, 33 were males (55%), 27 were females (45%), 26 died (43.3%), 34 survived (56.7%), and the median age of the patients was 65 (40-85) years old, 34 cases of IgG type (56.7%), 9 cases of IgA type (15%), 11 cases of light chain type (18.3%), 4 cases of IgD type (6.7%), 2 cases of the non-secretory type (3.3%); ISS Stages: 4 cases in stage I (6.7%), 19 cases in stage II (31.7%), and 37 cases in stage III (61.7%). There were 7 patients (11.7%) with elevated blood calcium, 7 patients (11.7%) with extramedullary infiltration, and 4 patients with early death (patients who died within 2 months after diagnosis). The range of white blood cells at the onset of the patient was (2.15~11.38) ×109/L. The range of platelets is (25~274) ×109/L. Ten of the 60 patients were involved in chromosomal abnormalities, including 4 with complex chromosomal karyotypes. FISH test was performed in all patients, and cytogenetic abnormalities were detected in 49 patients, with a cytogenetic detection rate of 81.7%. Among the patients, more common anomalies are 13q-, 1q+, IgH rearrangement, t (4;14), t (14;16), t (14;20), P53 deletion positive.
II Relationship between NLR and Clinical Characteristics
Among the 60 MM patients, 19 were in the high NLR group and 41 were in the low NLR group. The median age of patients in the high NLR group was 65 years and the average overall survival was 17.3 months, the median age of patients in the low NLR group was 66 years, and the average overall survival was 28.3 months. There were differences in OS, number of deaths, ISS stages, overall survival, and LDH between the two groups, and the differences between the two groups were statistically significant (P < 0.05). The other differences in gender, age, HGB, ALT, A/G, creatinine, PLT, β2-MG were not statistically significant (P > 0.05).
III Relationship between PLR and Clinical Characteristics
Among the 60 MM patients, 26 were in the high PLR group and 34 were in the low PLR group. The median age of patients in the high PLR group was 65 years and the average overall survival time was 14.7 months. The median age of patients in the low PLR group was 68 years, and the average overall survival time was 32.6 months. There were differences in OS, overall survival and platelet between the two groups, and the difference between the two groups was statistically significant (P < 0.05). The other differences in gender, age, ISS stages, ALT, HGB, number of deaths, A/G, creatinine, β2-MG and LDH were not statistically significant (P > 0.05).
IV Relationship between MLR and Clinical Characteristics
Among the 60 MM patients, 24 were in the high MLR group and 36 were in the low MLR group. The median age of patients in the high MLR group was 64 years, and the average overall survival time was 22.2 months, and the median age of patients in the low MLR group was 67 years, and the average overall survival time was 26.6 months. The two groups had differences in ISS staging, creatinine and other indicators, and the difference was statistically significant (P < 0.05). The other differences in OS, gender, age, survival time, number of deaths, HGB, ALT, platelets, A/G, β2-MG and LDH were not statistically significant (P > 0.05).
V Treatment Solutions
According to the general condition of the patient and the severity of the disease, the treatment such as general treatment, adjuvant treatment, chemotherapy and autologous stem cell transplantation are adopted. The chemotherapy regimens are mainly bortezomib-based therapies, such as bortezomib and dexamethasone, bortezomib, cyclophosphamide, and dexamethasone, bortezomib, immunomodulators and dexamethasone. Two patients received autologous stem cell transplantation after induction therapy.
VI Survival Status
Follow-up until May 26, 2020, among 60 patients, 34 survived and 26 died. The median overall survival was 24 months. The shortest survival period was 1 month, 4 patients died early and 2 died of infection, 3 cases were patients with significantly elevated creatinine at the first diagnosis. One of them died of exfoliative dermatitis during the first induction process, and one died of gastrointestinal bleeding during the induction process. The longest survival period was 84 months, and the patient was still alive at the end of the observation.
VII Univariate Analysis of Prognostic Risk Factors
Survival analyses were made by the method of Kaplan-Meier, with differences assessed by the long-rank test (Table 1). Univariate analysis suggests that NLR, PLR, age, ISS stages, ALT and HGB are associated with MM patients’ overall survival time; the difference was statistically significant (P < 0.05). MM patients with NLR ≥ 3.61, PLR ≥ 129.78, ≥ 65 years, ISS stage III, albumin < 35 g/L and hemoglobin < 100 g/L have a shorter and poorer prognosis. However, laboratory indicators such as MLR, immunoglobulin type, patient sex, creatinine level, LDH, β2-MG, A/G were not associated with overall survival (P > 0.05).
Table 1: Kaplan-Meier estimate of survival.
|
Parameters |
Number of cases |
χ2value |
P value |
|
Sex |
S |
0.425 |
0.515 |
|
Male |
33 |
|
|
|
Female |
27 |
|
|
|
Age |
|
6.015 |
0.014 |
|
< 65 years |
25 |
|
|
|
≥ 65 years |
35 |
|
|
|
NLR |
|
7.185 |
0.007 |
|
≥ 3.61 |
19 |
|
|
|
< 3.61 |
41 |
|
|
|
MLR |
|
1.276 |
0.259 |
|
≥ 0.33 |
24 |
|
|
|
< 0.33 |
36 |
|
|
|
PLR |
|
10.121 |
0.001 |
|
≥ 129.78 |
26 |
|
|
|
< 129.78 |
34 |
|
|
|
ISS Stages |
|
8.097 |
0.004 |
|
I~II |
23 |
|
|
|
III |
37 |
|
|
|
HGB |
|
7.399 |
0.007 |
|
≥ 100g/L |
18 |
|
|
|
< 100g |
42 |
|
|
|
ALT |
|
3.969 |
0.046 |
|
≥ 35g/L |
22 |
|
|
|
< 35g/L |
38 |
|
|
|
A/G |
|
1.69 |
0.194 |
|
≥ 1.2 |
18 |
|
|
|
< 1.2 |
42 |
|
|
|
β2-MG |
|
1.968 |
0.161 |
|
> 2.3 |
47 |
|
|
|
≤ 2.3 |
13 |
|
|
|
Cr |
|
1.235 |
0.266 |
|
≥ 177μmol/L |
16 |
|
|
|
< 177μmol/L |
44 |
|
|
|
LDH |
|
0.701 |
0.403 |
|
> 250U/L |
10 |
|
|
|
< 250U/L |
50 |
|
|
VIII The Influence of NLR and PLR on the Overall Survival of MM Patients
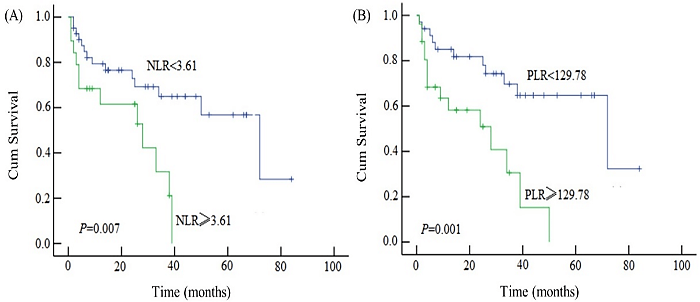
The overall survival of patients with NLR ≥ 3.61 was significantly different from that of patients with NLR < 3.61 (P=0.007). The overall survival of patients with PLR ≥ 129.78 was significantly different from that of patients with PLR < 129.78 (P=0.001) (Figure 1).
Figure 1: A) Kaplan-Meier estimate of survival according to NLR; B) Kaplan-Meier estimate of survival according to PLR.
IX Multivariate Analysis of Prognostic Risk Factors
Cox regression analysis was performed on 60 patients, and the factors found in univariate analysis to be related to the total survival of the patients were further analysed by multivariate analysis (P < 0.05). The results indicated that PLR, HGB and ISS stages at the initial diagnosis were independent prognostic risk factors affecting the total survival of the patients (P < 0.05) (Table 2).
Table 2: Results of patient multivariate analysis (Cox regression model).
|
Parameters |
B |
SE |
Wald |
df |
P value |
RR value |
95%CI |
|
ISS stages |
1.791 |
0.578 |
9.610 |
1 |
0.002 |
5.995 |
(1.932-18.603) |
|
HGB |
1.749 |
0.623 |
7.872 |
1 |
0.005 |
5.747 |
(1.649-19.497) |
|
PLR |
1.581 |
0.467 |
11.475 |
1 |
0.001 |
4.681 |
(1.947-12.135) |
Discussion
Multiple myeloma is a malignant clonal plasma cell disease that originates from terminally differentiated B lymphocytes after the germinal center. It is characterized by the proliferation of monoclonal plasma cells in the bone marrow and the synthesis and secretion of monoclonal immunoglobulins, leading to hypercalcemia and renal end-organ damage such as functional impairment, anemia, and bone destruction is the second most common malignant tumor of the blood system and it is still an incurable disease [6]. The progression of neoplastic diseases is the result of various complex interactions of the body leading to various cellular changes in the bone marrow microenvironment. It is prone to be infection, immunosuppression and tumor progression, and there are numerous complex inflammation and angiogenesis processes in its progression [7]. Chronic inflammation leading to disease is part of the pathogenesis of multiple myeloma. Neutrophils and lymphocytes are the main cells of inflammation and immune response. So complete blood count can provide prognostic information for malignant tumors [8]. NLR and PLR are simpler systemic inflammatory indicators that can provide prognostic information for cancer [2].
Ethier et al. conducted a meta-analysis of 15 clinical studies on NLR prognosis in 8,563 patients, showing that patients with higher NLR had shorter PFS and OS [9]. Currently, NLR has been reported in hematologic tumors and in multiple myeloma, but the results are inconsistent. Zhou et al. found that MM patients receiving bortezomib as induction therapy, the induced complete response rate was 20% in patients with NLR ≥ 2.95 and 39.2% in patients with NLR < 2.95, and the increase of NLR was associated with shorter OS in patients, but it was not an independent risk factor for prognosis of multiple myeloma [10]. Onec et al. retrospective analysis of 52 cases of patients with multiple myeloma NLR and laboratory examination, founding that NLR is associated with C-reactive protein and β2-MG, NLR > 1.72 patients have high ISS in instalment, poor physical condition and renal function, NLR > 1.72 patients' overall survival was 26.14 months, and NLR ≤ 1.72 patients' overall survival was 42.75 months, two groups of survival difference was statistically significant (P < 0.05) [11].
Our center selected 60 patients with newly diagnosis of multiple myeloma, selected all of the patients’ average NLR as cut-off values, divided the patients into high NLR group (NLR 3.61 or higher) and low NLR (NLR < 3.61), found that compared to high NLR group. Overall survival of lower NLR group was obviously prolonged (28.3 months versus 17.3 months, P < 0.05), and the NLR ≥ 3.61 is new adverse prognostic factors in patients with MM, but not independent risk factors of poor prognosis. However, the other studies have found that higher NLR is an independent risk factor for poor prognosis in MM patients who are not suitable for transplantation or newly diagnosed [12-14]. The interaction between PLR and tumor prognosis has been studied in many solid tumors, such as esophageal cancer, ovarian cancer and fallopian tube cancer, etc.
However, the mechanism of PLR's role in tumor prognosis is not clear at present, and relevant studies have been rarely reported. Due to reactive thrombosis may be associated with inflammation, activation of platelets in a variety of forms to promote tumor occurrence, the development of growth or metastatic carcinoma, can secrete a variety of angiogenesis and tumor growth factors, such as C-reactive protein, thrombospondin-1 (TSP-1), transformation generates factor (TGFβ) and vascular endothelial growth factor (VEGF) and platelet-derived growth factor and accelerated the growth of tumor angiogenesis by promoting [15, 16]. Platelets play a significant role in the progression of tumor metastasis, which may be related to affecting angiogenesis. It protects tumor cells from the immune system by forming tumor thrombus. Platelets, neutrophils and lymphocytes have a significant effect on the prognosis of solid tumor patients.
The importance has been confirmed, PLR has also been studied as a prognostic marker, and higher PLR is considered to be an increase in inflammation associated with more aggressive tumor characteristics [17, 18]. Wongrakpanich et al. retrospectively analysed 175 MM patients and divided them into NLR ≥ 2.78 group, NLR < 2.78 group, PLR ≥ 155.58 group and PLR < 155.58 group [19]. They found that the high NLR and high PLR groups all had lower levels of albumin and higher ISS stages; the low NLR group has a longer overall survival than the high NLR group (66 months vs 37 months, P < 0.05). Compared with the low PLR group, there was no significant difference in overall survival between the high PLR group and the low PLR group (45 months vs 62 months, P=0.07), and NLR ≥ 2.78 was an independent risk factor for poor prognosis.
Solmaz et al. retrospectively analysed the clinical data of 186 newly diagnosed MM patients and studied the correlation between NLR, MLR, PLR and prognosis [20]. The cut-off values of NLR, PLR and MLR were 1.9, 120 and 0.27, respectively, and found that PLR < 120 is an independent risk factor for poor prognosis, and there is no statistically significant difference in OS and PFS between high-low group NLR and high-low group MLR patients. Our study found that MM patients with PLR ≥ 129.78 have a poor prognosis, which is related to overall survival and is an independent risk factor for poor prognosis. It is contrary to the results of Solmaz et al., and contrary to some domestic and foreign research results, and MLR has no effect on survival. Obvious impact, consistent with foreign reports.
The results of this study are not consistent with the results of some research centers, domestic and overseas. There may be the following reasons: 1) This study is a retrospective study of a single center. Most of the patients come from the region, which may be influenced by regional and economic influences and has certain limitations. 2) Different study groups have different clinical characteristics of the patients enrolled, leading to differences in the values of neutrophils, lymphocytes, and platelets in patients, resulting in differences in NLR, PLR, and MLR; 3) There is no consensus on the selection of cut-off values at home and abroad. At present, there are mainly three methods: median, mean, and receiver operating characteristic curve (ROC curve) interception point. In this study, the average NLR average 3.61 and the PLR average 129.78 are the cut-off values. Different methods for selecting critical values may also lead to different research results.
We found that NLR and PLR among inflammatory markers were linked to the prognosis of newly diagnosed MM patients, and PLR is an independent risk factor for poor prognosis. NLR and PLR are convenient and economical parameters, which can be used as prognostic indicators for newly diagnosed MM. MLR has nothing to do with the overall survival time of newly diagnosed patients, and it will not have anything to do with the prognosis. The pathophysiological mechanism of the association between NLR and PLR and poor prognosis of MM is currently unknown, and further research is required.
Funding
This work was supported by Natural Science Youth Foundation of Jiangsu (BK20180372); Jiangsu Provincial Key Discipline of Medicine (ZDXKB2016020); Science and Technology Bureau Social Undertaking Science and Technology Development Project of Nanjing Jiangning District (2019SHSY0034).
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 11, Aug 2020Accepted: Tue 25, Aug 2020
Published: Tue 01, Sep 2020
Copyright
© 2023 Baoan Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2020.09.01
Author Info
Lin Gui Jinning Shi Wei Zhang Wenjing Zhang Fei Wang Baoan Chen
Corresponding Author
Baoan ChenDepartment of Hematology and Oncology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, Jiangsu Province, China
Figures & Tables
Table 1: Kaplan-Meier estimate of survival.
|
Parameters |
Number of cases |
χ2value |
P value |
|
Sex |
S |
0.425 |
0.515 |
|
Male |
33 |
|
|
|
Female |
27 |
|
|
|
Age |
|
6.015 |
0.014 |
|
< 65 years |
25 |
|
|
|
≥ 65 years |
35 |
|
|
|
NLR |
|
7.185 |
0.007 |
|
≥ 3.61 |
19 |
|
|
|
< 3.61 |
41 |
|
|
|
MLR |
|
1.276 |
0.259 |
|
≥ 0.33 |
24 |
|
|
|
< 0.33 |
36 |
|
|
|
PLR |
|
10.121 |
0.001 |
|
≥ 129.78 |
26 |
|
|
|
< 129.78 |
34 |
|
|
|
ISS Stages |
|
8.097 |
0.004 |
|
I~II |
23 |
|
|
|
III |
37 |
|
|
|
HGB |
|
7.399 |
0.007 |
|
≥ 100g/L |
18 |
|
|
|
< 100g |
42 |
|
|
|
ALT |
|
3.969 |
0.046 |
|
≥ 35g/L |
22 |
|
|
|
< 35g/L |
38 |
|
|
|
A/G |
|
1.69 |
0.194 |
|
≥ 1.2 |
18 |
|
|
|
< 1.2 |
42 |
|
|
|
β2-MG |
|
1.968 |
0.161 |
|
> 2.3 |
47 |
|
|
|
≤ 2.3 |
13 |
|
|
|
Cr |
|
1.235 |
0.266 |
|
≥ 177μmol/L |
16 |
|
|
|
< 177μmol/L |
44 |
|
|
|
LDH |
|
0.701 |
0.403 |
|
> 250U/L |
10 |
|
|
|
< 250U/L |
50 |
|
|
Table 2: Results of patient multivariate analysis (Cox regression model).
|
Parameters |
B |
SE |
Wald |
df |
P value |
RR value |
95%CI |
|
ISS stages |
1.791 |
0.578 |
9.610 |
1 |
0.002 |
5.995 |
(1.932-18.603) |
|
HGB |
1.749 |
0.623 |
7.872 |
1 |
0.005 |
5.747 |
(1.649-19.497) |
|
PLR |
1.581 |
0.467 |
11.475 |
1 |
0.001 |
4.681 |
(1.947-12.135) |
References
- Florian R Greten, Sergei I Grivennikov (2019) Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 51: 27-41. [Crossref]
- Serife Solmaz Medeni, Celal Acar, Aybuke Olgun, Alev Acar, Ahmet Seyhanli et al. (2018) Can Neutrophil-to-Lymphocyte Ratio, Monocyte-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio at Day +100 be used as a prognostic marker in Multiple Myeloma patients with autologous transplantation? Clin Transplant 32: e13359. [Crossref]
- Nathan A Cannon, Jeffrey Meyer, Puneeth Iyengar, Chul Ahn, Kenneth D Westover et al. (2015) Neutrophil-lymphocyte and platelet-lymphocyte ratios as prognostic factors after stereotactic radiation therapy for early-stage non-small-cell lung cancer. J Thorac Oncol 10: 280-285. [Crossref]
- Arnoud J Templeton, Olga Ace, Mairéad G McNamara, Mustafa Al Mubarak, Francisco E Vera Badillo et al. (2014) Prognostic role of platelet to lymphocyte ratio in solid tumors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev 23: 1204-1212. [Crossref]
- S Vincent Rajkumar, Meletios A Dimopoulos, Antonio Palumbo, Joan Blade, Giampaolo Merlini et al. (2014) International Myeloma working group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol 15: e538-e548. [Crossref]
- Dae Sik Kim, Eun Sang Yu, Ka Won Kang, Se Ryeon Lee, Yong Park et al. (2017) Myeloma prognostic index at diagnosis might be a prognostic marker in patients newly diagnosed with multiple myeloma. Korean J Intern Med 32: 711-721. [Crossref]
- Yang Han, Xidi Wang, Bingping Wang, Guosheng Jiang (2016) The progress of angiogenic factors in the development of leukemias. Intractable Rare Dis Res 5: 6-16. [Crossref]
- Shanthini M Crusz, Frances R Balkwill (2015) Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol 12: 584-596. [Crossref]
- Josee Lyne Ethier, Danielle Desautels, Arnoud Templeton, Prakesh S Shah, Eitan Amir (2017) Prognostic role of neutrophil-to lymphocyte ratio in breast cancer: a systematic review and meta-analysis. Breast Cancer Res 19: 2. [Crossref]
- Xin Zhou, Jing Wang, Jun Xia, Feng Cheng, Jingjue Mao et al. (2018) Evaluation of neutrophil-to-lymphocyte ratio in newly diagnosed patients receiving bortezomib-based therapy for multiple myeloma. Cancer Biomark 22: 43-48. [Crossref]
- Birgul Onec, Harika Okutan, Murat Albayrak, Esra Saribacak Can, Vedat Aslan et al. (2017) The Predictive Role of the Neutrophil/Lymphocyte Ratio in Survival with Multiple Myeloma: A Single Center Experience. J Clin Lab Anal 31: e22032. [Crossref]
- Gyeong Won Lee, Sung Woo Park, Se Il Go, Hoon Gu Kim, Min Kyoung Kim et al. (2018) The Derived Neutrophil-to-Lymphocyte Ratio Is an Independent Prognostic Factor in Transplantation Ineligible Patients with Multiple Myeloma. Acta Haematol 140: 146-156. [Crossref]
- J J Hu, S M Nie, Y Gao, X S Yan, J X Huang et al. (2019) The correlations and prognostic value of neutrophil to lymphocyte ratio, immunophenotype and cytogenetic abnormalities in patients with newly diagnosed multiple myeloma. Zhonghua Xue Ye Xue Za Zhi 40: 1044-1046. [Crossref]
- Yanjie Li, Hujun Li, Wenjing Li, Lijin Wang, Zhiling Yan et al. (2017) Pretreatment neutrophil/lymphocyte ratio but not platelet/lymphocyte ratio has a prognostic impact in multiple myeloma. J Clin Lab Anal 31: e22107. [Crossref]
- Z Baranyai, M Krzystanek, V Jósa, K Dede, E Agoston et al. (2014) The comparison of thrombocytosis and platelet-lymphocyte ratio as potential prognostic markers in colorectal cancer. Thromb Haemost 111: 483-490. [Crossref]
- Takashi Tsuruo, Naoya Fujita (2008) Platelet aggregation in the formation of tumor metastasis. Proc Jpn Acad Ser B Phys Biol Sci 84: 189-198. [Crossref]
- Tarik Salman, Seher Nazli Kazaz, Umut Varol, Utku Oflazoglu, Ilkay Tugba Unek et al. (2016) Prognostic Value of the Pretreatment Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio for Patients with Neuroendocrine Tumors: An Izmir Oncology Group Study. Chemotherapy 61: 281-286. [Crossref]
- Aime T Franco, Adam Corken, Jerry Ware (2015) Platelets at the interface of thrombosis, inflammation, and cancer. Blood 126: 582-588. [Crossref]
- Supakanya Wongrakpanich, Gemlyn George, Wikrom Chaiwatcharayut, Sylvia Biso, Nellowe Candelario et al. (2016) The Prognostic Significance of Neutrophil-to-Lymphocyte and Platelet-to-Lymphocyte Ratios in Patients with Multiple Myeloma. J Clin Lab Anal 30: 1208-1213. [Crossref]
- Serife Solmaz, Ozcan Uzun, Celal Acar, Omur Gokmen Sevindik, Ozden Piskin et al. (2018) Is the platelet to lymphocyte ratio a new prognostic marker in multiple myeloma? J Lab Physicians 10: 363-369. [Crossref]
