Temporary Perineal Urethrostomy During Holmium Laser Enucleation of the Prostate (HoLEP)
A B S T R A C T
Purpose: To characterize the role of perineal urethrostomy in patients undergoing HoLEP for BPH symptom relief.
Methods: We identified all patients who required the creation of a perineal urethrostomy from a prospectively maintained institutional database between 1998-2017. Patient demographics, as well as operative and postoperative records, were analyzed to evaluate differences in those patients requiring a perineal urethrostomy.
Results Obtained: We identified 7 patients who underwent HoLEP and required a perineal urethrostomy. The mean age was 70 years old (range: 61-82 years old). Within this subset of patients, four had previously aborted BPH procedures; two had penile prosthesis and two were morbidly obese. The mean final prostate specimen weight was 111 grams (range: 23-319). The duration of catheterization varied from 37-600 hours. In patients with BMI ≥40kg/m2, the average duration of catheterization was 588 hours compared 119 hours in patients with BMI <40kg/m2. At the six-month follow-up, no patient reported daytime incontinence. No strictures, fistulae, or diverticula were identified in these patients.
Conclusion: Utilizing a temporary perineal urethrostomy during HoLEP, or any transurethral BPH procedure, for a small subset of patients with challenging anatomy represents an important skill in the endoscopist’s armamentarium. We note no adverse events aside from prolonged urinary catheterization. Surgeons should consider temporary perineal urethrostomy in lieu of aborting the procedure with the knowledge that it is safe and presents minimal long-term risks.
Keywords
HoLEP, urethrostomy, BPH
Introduction
Holmium laser enucleation of the prostate (HoLEP) represents a versatile outlet procedure for prostates of all sizes, resulting in a durable reduction in lower urinary tract symptoms related to benign prostate hyperplasia (BPH) [1, 2]. Outcomes are independent of size and HoLEP has been demonstrated to be at least equivalent, if not a superior treatment to transurethral resection of the prostate (TURP) [3]. While HoLEP can be performed in prostates of any size, there are limitations to the length of equipment utilized and, in some circumstances, it may be necessary to bypass the penile urethra in order to successfully perform the procedure.
A temporary perineal urethrostomy has been utilized at the time of TURP with success, with the thought that this approach would decrease the rate of urethral stricture disease by limiting the amount of urethra traversed by the scope [4, 5]. Although the practice of routine perineal urethrostomy at time of endoscopic surgery has been largely abandoned, the utilization of a temporary perineal urethrostomy for men with large prostates or difficult anatomy undergoing HoLEP has been successful in our practice to avoid conversion to an open suprapubic procedure when endoscopic instruments are not long enough to reach the bladder. Thus, we describe our surgical technique and experience in this unique patient population.
Methods
An Institutional Review Board approved prospectively collected and maintained institutional database of HoLEP patients between 1998-2017 was reviewed and utilized for this investigation. Patients who underwent a perineal urethrostomy at the time of surgery were identified and perioperative outcomes were examined in this unique group of patients.
Description of Technique
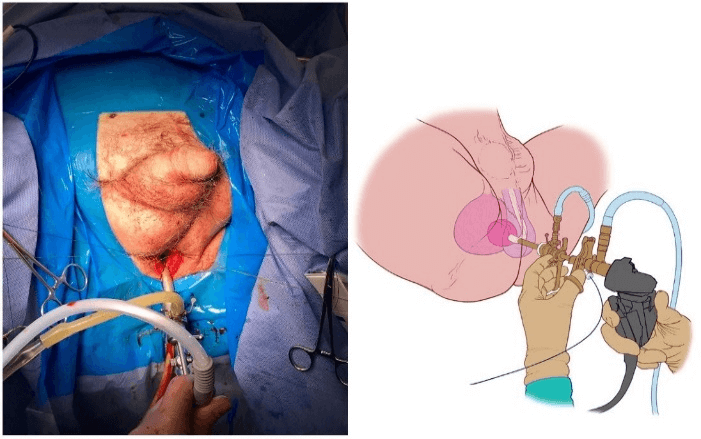
Attempted placement of the laser resectoscope is performed after urethral dilation using sequential metal sounds. If the laser resectoscope cannot successfully be advanced into the bladder, then a perineal urethrostomy is necessary to successfully complete the HoLEP procedure. To perform the perineal urethrostomy, the laser resectoscope is removed, and a 28F sound is placed within the urethra (Figure 1). A vertical incision is made on the perineum approximately 6cm in length over the sound. The dissection is carried through the bulbospongiosum muscle, which is split in the midline. Care is taken to avoid the bulbar artery, which can result in considerable bleeding if the dissection veers lateral and deep to the muscle.
Figure 1: A vertical incision directly over the bulbar urethra with a urethral sound in place.
In the morbidly obese patient, the distance from the skin to the urethra can be several centimeters; so, use of a self-retaining retractor is often necessary. Once the bulbar urethra is palpated, a sharp incision approximately 1-2 cm in length is carried through the spongy tissue until the scalpel reaches the sound (Figure 2). We utilize full-thickness chromic stay sutures through the urethra that are tagged to the drape to assist retraction and easy identification of the urethra at the time of closure. We minimize cautery on the delicate spongy tissue to reduce the propagation of thermal injury, subsequent devascularization and stricture. Once hemostasis is achieved, the sound is removed, and the laser scope is placed into the urethra via the perineal opening (Figure 3). The rest of the HoLEP procedure is performed as per previous description [6]. Once morcellation is completed, a three-way catheter mounted on a mandarin guide is placed via the natural urethral opening to allow the surgeon to direct it past the perineal defect and into the bladder. The perineal urethral opening is then closed. Care must be taken to avoid incidental puncture of the catheter when closing the urethra. We utilize a 3-0 absorbable vicryl suture and perform a two-layer closure, ensuring opposition of the urethral mucosal and spongy tissue. The bulbospongiosum muscle is reapproximated, and the subcutaneous tissues and skin are closed with 4-0 absorbable chromic suture.
Figure 2: Initial dissection through the bulbospongiosus muscle.
Figure 3: Laser scope deployment into the bulbar urethra.
Results
We identified 7 patients who underwent HoLEP and required a perineal urethrostomy between 2002 and 2017. The mean age was 70 years (range: 61-82 years) and the mean BMI 47.13 (26.1-70). Reasons for perineal urethrostomy included: 1 patient with an extremely large prostate (>300 grams), 4 patients with extremely large prostates who had previously aborted BPH procedures, 2 of these aborted procedures were because of morbid obesity (BMI ≥40), and 2 because of penile prosthesis. The mean AUA SS for the group was 21.3 (range 14-26), and PVR for those not in retention or intermittently catheterizing was 94.8 (range 78-111). Prior to surgical intervention, 1 patient had an indwelling catheter preoperatively, 1 patient was intermittently catheterizing, and 1 patient had a concomitant bladder stone.
The mean weight of the final specimen was 111 grams (range: 23-319). No patient was diagnosed with prostate cancer on the postoperative specimen, and no patient required blood transfusion. The duration of catheterization varied from 37-600 hours. In patients with BMI ≥40kg/m2, the average duration of catheterization was 588 hours compared to 119 hours in patients with BMI <40kg/m2. At six-month follow-up, no patient reported day or nighttime incontinence, mean AUA SS was 7.3 (range 1-17). Mean PSA post-HoLEP was 1.2 (range 0.3-2.7). No strictures, fistulas, or diverticula were identified in these patients.
Discussion
We identified a small cohort of patients with significant anatomic constraints necessitating a perineal urethrostomy in order to complete a HoLEP for outlet obstruction. While there was significant variability in prostate size, as well as patient BMI, we did not identify any complications with regards to the temporary perineal urethrostomy. Likewise, catheter duration was relatively brief, with no evidence of incontinence at the six-month follow-up. We did note that patients with a higher BMI were more likely to require a longer catheterization time than those who were smaller.
HoLEP is an effective endourological treatment option for symptomatic BPH patients with large prostate glands. In this subset of patients with large prostates, the average specimen weight was 110.7 (23.3-284) grams. Previously we have reported on patients with preoperative TRUS calculated weight > 175g [7]. In this series of 57 patients, the mean operative time was approximately 2 hours, and a mean enucleated weight of 176.4g. The mean duration of catheterization and hospital stay were 18.5 and 26 hours, respectively. The overall complication rate was 5% with no subsequent procedure performed. At 6 months follow up, the AUA symptom score was 6.6, the mean PSA was 0.78 and the average Qmax was 18.5 [7]. Matlaga et al. reported similar results in patients with preoperative TRUS calculated weight > 125g [8].
In 86 patients, the mean operative time and hospital stay were 128 minutes and 26 hours, respectively. The mean PSA level and AUA symptom score at 1 year were 0.96 ng/ml (90% reduction) and 5.1, respectively [8]. Humphreys et al. stratified HoLEP outcomes based on gland size and reported that hospitalization, catheterization, complication rates, and postoperative outcomes were similar for glands <75g, 75g to 125g, and >125g [9]. This reinforces the safety and efficacy of HoLEP in patients with large prostates, which was seen in our group of patients. Furthermore, these results and limited adverse events support the role of HoLEP over simple prostatectomy even when perineal urethrostomy is needed for large prostate glands.
The mean catheterization time for our cohort was 10.5 (1.4-25) days, and there were no blood transfusions. Kuntz et al. compared HoLEP to open prostatectomy (OP) in prostates greater than 100 grams and reported catheterization time of 1.25 days and 8.1 days for HoLEP and OP, respectively. The transfusion rate was zero for HoLEP and 13.3% in the OP group [10]. Zhang et al. recently studied HoLEP vs. robotic-assisted simple prostatectomy (RSP). In their study, the catheterization time for HoLEP was 0.7 days and 8 days in the RSP group. They reported a transfusion rate of 1.8% for HoLEP and 9.4% for RSP [11]. Four of the six patients in our cohort underwent surgical retreatment of BPH after aborted TURP elsewhere. These patients in our cohort treated continued to have no adverse outcome with the HoLEP surgery, despite prior instrumentation, which is consistent with the current literature.
Marien et al. described similar catheterization times in patients undergoing HoLEP for surgical retreatment when compared to primary HoLEP procedures [12]. While HoLEP with a perineal urethrostomy does prolong catheterization to allow for the urethral closure to heal, it does not considerably prolong catheterization or hospitalization time and has significantly lower transfusion rates when compared to the other standard of care procedures discussed above. Importantly there were no complications associated with catheter removal in our cohort, and the patients experienced no adverse sequelae from the urethral incision despite significant comorbidities.
Historically, surgeons previously utilized a perineal urethrostomy to combat high stricture rates in patients undergoing a TURP with unaccommodating urethras. Melchior and colleagues performed prostate resections via a perineal urethrostomy on patients whose urethras would not comfortably accommodate a 28F resectoscope sheath or when the prostate was estimated to be greater than 40 grams [4]. In their series, the authors reported no mortality and low morbidity with a significant complication of false passage creation during the procedure occurring in only 2 of 676 patients (0.3%) and an overall complication rate of 2.4%. All patients were catheterized for only 3 days in the immediate postoperative period [4]. Bissada et al. compared stricture rates in patients undergoing TURP vs. prostate resection via perineal urethrostomy (TPRP) [5]. The reported stricture rate for TURP and TPRP was 16.4% and 2.27%, respectively. Thus, they concluded that perineal urethrostomy should be performed at the earliest question of urethral accommodation to the resectoscope [5]. Elmansy et al. studied the long-term outcomes of HoLEP at 10-year follow-up and reported bladder neck contracture, urethral stricture and reoperation rate in 0.8%, 1.6% and 0.7% patients, respectively [13].
In our study, we found no evidence of stricture disease in any of the six patients at last follow-up. An important consideration while performing a perineal urethrostomy is the urethral blood supply. Transection of the bulbar urethra can diminish the retrograde blood supply from the dorsal penile artery [14]. Due to this, there is potential for the development of a future stricture due to worsening vascular blood supply. Myers et al. reviewed the outcomes of perineal urethrostomy and recommended the use of a large longitudinal urethrostomy in preventing future complications [14]. Thus, stricture formation can best be prevented with a longitudinal incision like the one performed in this series.
Our study has limitations that should be addressed. First, we report on a very small, select group of patients. Further research on a larger subset of patients is needed to provide more information on the topic. Second, as a tertiary referral center, our patient follow-up was limited at only six months. Though limited, most stricture related complications are detected at 1- or 3-month follow-up, thus short term follow up provides the most valuable information on this group of subjects [5]. Despite these limitations, this study adds important information to the literature about performing a HoLEP procedure on a patient with difficulty anatomy and offers instructions on how to perform the temporary perineal urethrostomy as part of the HoLEP.
Conclusion
Utilizing a temporary perineal urethrostomy during HoLEP, or any transurethral BPH procedure, for a small subset of patients with challenging anatomy represents an important skill in the endourologist’s surgical armamentarium. We note no adverse events aside from slightly prolonged urinary catheterization when a temporary perineal urethrostomy was performed at the time of HoLEP. Potential patients who may require a temporary perineal urethrostomy are exceptionally large gland prostates, the morbidly obese, or those with a functioning implanted penile prosthesis. Surgeons should consider temporary perineal urethrostomy in lieu of aborting the procedure or performing open prostatectomy in such patients with the knowledge that it is safe and presents minimal long-term risks.
Disclosure
No competing financial interests exist. Dr. Lingeman is a consultant for Lumenis and Boston Scientific. He also has financial interests in Beck Laboratories. Dr. Krambeck is a consultant for Boston Scientific and Lumenis. Dr. Large is a consultant for Boston Scientific. Dr. Rivera is a consultant for Lumenis, Cook, and Boston Scientific.
Ethical Approval
This study utilized data from an IRB approved prospectively maintained database.
Consent
Proper informed consent was obtained.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 24, Apr 2020Accepted: Thu 07, May 2020
Published: Fri 15, May 2020
Copyright
© 2023 Joshua Heiman. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.02.04
Author Info
Amy Krambeck Deepak Agarwal James Lingeman Joshua Heiman Marcelino Rivera Tim Large
Corresponding Author
Joshua HeimanIndiana University School of Medicine, Department of Urology, Indianapolis, Indiana, USA
Figures & Tables


References
- Krambeck AE, Handa SE, Lingeman JE (2010) Experience with more than 1,000 holmium laser prostate enucleations for benign prostatic hyperplasia. J Urol 183: 1105-1109. [Crossref]
- Elkoushy MA, Elshal AM, Elhilali MM (2015) Reoperation After Holmium Laser Enucleation of the Prostate for Management of Benign Prostatic Hyperplasia: Assessment of Risk Factors with Time to Event Analysis. J Endourol 29: 797-804. [Crossref]
- Tan AH, Gilling PJ, Kennett KM, Frampton C, Westenberg AM et al. (2003) A randomized trial comparing holmium laser enucleation of the prostate with transurethral resection of the prostate for the treatment of bladder outlet obstruction secondary to benign prostatic hyperplasia in large glands (40 to 200 grams). J Urol 170: 1270-1274. [Crossref]
- Melchior J, Valk WL, Foret JD, Mebust WK (1974) Transurethral resection of the prostate via perineal urethrostomy: complete analysis of 7 years of experience. J Urol 111: 640-643. [Crossref]
- Bissada NK (1977) Transurethral resection of prostate via perineal urethrostomy: follow-up report. Urology 10: 39-41. [Crossref]
- Dusing MW, Krambeck AE, Terry C, Matlaga BR, Miller NL et al. (2010) Holmium laser enucleation of the prostate: efficiency gained by experience and operative technique. J Urol 184: 635-640. [Crossref]
- Krambeck AE, Handa SE, Lingeman JE (2010) Holmium laser enucleation of the prostate for prostates larger than 175 grams. J Endourol 24: 433-437. [Crossref]
- Matlaga BR, Kim SC, Kuo RL, Watkins SL, Lingeman JE (2006) Holmium laser enucleation of the prostate for prostates of> 125 mL. BJU Int 97: 81-84. [Crossref]
- Humphreys MR, Miller NL, Handa SE, Terry C, Munch LC et al. (2008) Holmium laser enucleation of the prostate--outcomes independent of prostate size? J Urol 180: 2431-2435. [Crossref]
- Kuntz RM, Lehrich K, Ahyai SA (2008) Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5-year follow-up results of a randomised clinical trial. Eur Urol 53: 160-166. [Crossref]
- Zhang MW, El Tayeb MM, Borofsky MS, Dauw CA, Wagner KR et al. (2017) Comparison of perioperative outcomes between holmium laser enucleation of the prostate and robot-assisted simple prostatectomy. J Endourol 31: 847-850. [Crossref]
- Marien T, Kadihasanoglu M, Miller NL (2016) Holmium laser enucleation of the prostate: patient selection and perspectives. Res Rep Urol 8: 181-192. [Crossref]
- Elmansy HM, Kotb A, Elhilali MM (2011) Holmium laser enucleation of the prostate: long-term durability of clinical outcomes and complication rates during 10 years of followup. J Urol 186: 1972-1976. [Crossref]
- Myers JB, Porten SP, McAninch JW (2011) The outcomes of perineal urethrostomy with preservation of the dorsal urethral plate and urethral blood supply. Urology 77: 1223-1227. [Crossref]
