Journals
Talus, anteromedial subtalar articular surface fracture dislocation. Case report and review of literature
A B S T R A C T
Introduction Talus fractures are uncommon and accounted for 2% of all lower limbs’ fractures. Due to its unique anatomical and biomechanical structure, talus plays an important role in ankle biomechanics. Talar fracture and/or dislocation can be associated with significant disability.
Case Presentation A case report to describe the presentation, management, and outcomes of 25 years old patient who presented with talar dislocation and associated rare fracture of infero-medial talar articular surface in anterior subtalar joint.
Treatment and outcomesopen reduction and internal fixation with three cannulated screws was performed. At 10 weeks follow-up, there was enough clinical and radiological evidence to suggest fracture healing. Patient allowed to weight bear using walker boot.
Discussionwe presented a rare case of talus fracture dislocation which was treated surgically with open reduction and internal fixation with satisfactory outcomes at 10 weeks of follow up.
Keywords
Talus, subtalar joint, fracture, dislocation, surgery
Introduction
Talus dislocation is commonly seen as results of high energy trauma, which is usually enough to detach it from the surrounding soft tissue [1]. Talus plays an important role in ankle biomechanics as it is supporting and distributing the forces applied to it during weight bearing [2]. Talus has unique biomechanical features and vascular supply, which means that talar fracture and/or dislocation, despite being uncommon, could result in significant disability [2]. The most common complications are avascular necrosis, non-union, osteoarthritis, and infection [1]. We report a rare case of fracture dislocation of the talus.
Case Presentation
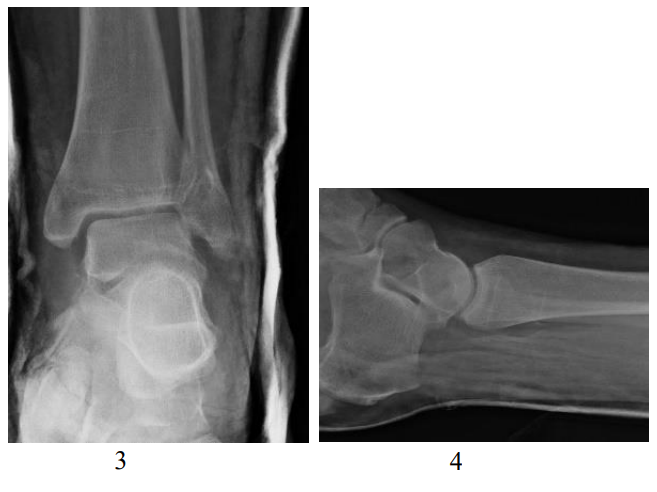
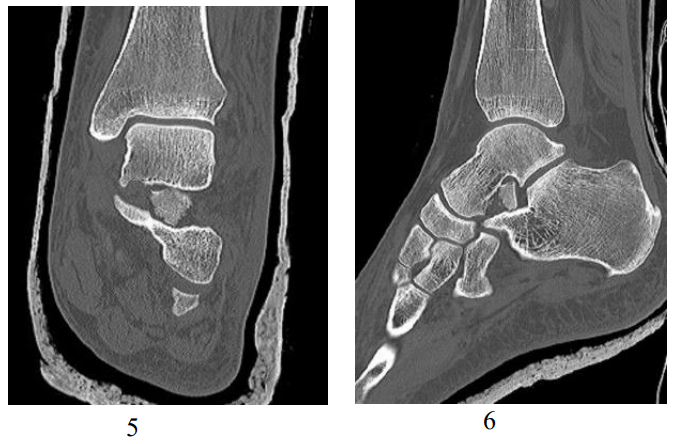
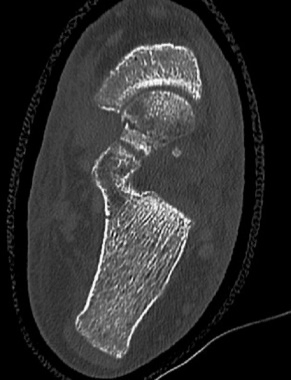
A 25 years old patient slipped on the stairs, falling on a left inverted foot. He presented to the emergency department with significant ankle/foot swelling and deformity. The foot was neurovascularly intact and it was a closed injury. Radiographs revealed talus dislocation out of ankle and subtalar joints (Figure 1 & 2). A successful close reduction was performed in the emergency department in sedation (Figure 3 & 4). Post reduction CT scan showed a displaced fracture of the antero-infero-medial articular surface of talus in anterior subtalar joint (Figure 5 & 6).
Treatment
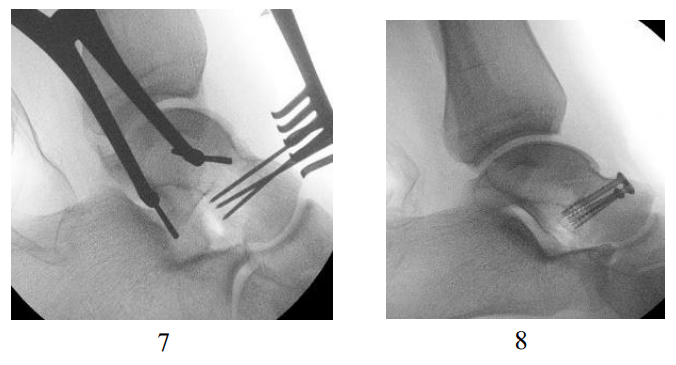
After an interval of around 1 week to let soft tissue settle, an anteromedial approach used to approach the subtalar joint. Joint was distracted and fractured infero-medial segment of talus retrieved from subtalar joint and reduced. Through separate anterior midline approach using small incision, anterior cruciate ligament (ACL) jig used to help insertion of the guide wires. Cannulated lag screws were used to fix the fractured fragment (Fig. 7 & 8). He was managed in a non-weight bearing cast for ten weeks.
Outcomes and follow-up
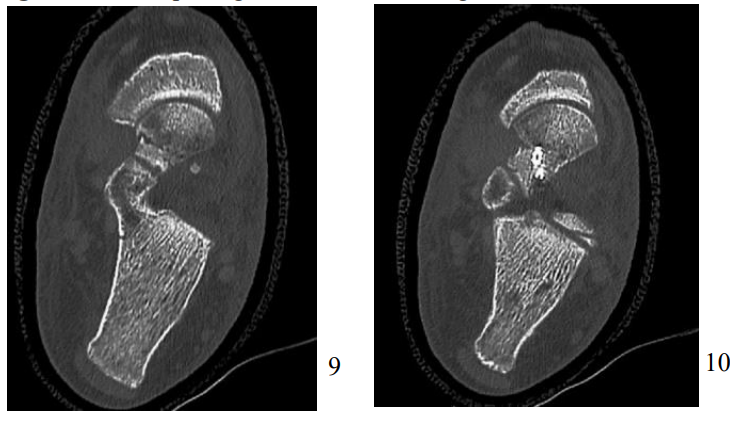
Post-operatively, the patient followed up at 2 weeks for a wound check and at 10 weeks. Follow up CT scan at 10 weeks showed fracture to remain well fixed with early signs of healing (Figure 9 & 10). Patients’ symptoms were improving, and he allowed to weight bear with walker boot at 10 weeks after surgery. The postoperative outcomes were assessed using Foot and Ankle Ability Measure / Activity of Daily Living (FAAM / ADL), and the Manchester-Oxford Foot Questionnaire (MOXFQ) [3]. FAAM / ADL score was 50% at 10 weeks follow-up after surgery (which implies increased parameters to perform activities of daily living). On the other hand, MOXFA was used to evaluate improvement in its three domains: pain, problems with social interaction, and difficulties with walking/standing. Pain score improved from 70% at 2 weeks follow up down to 10% at 10 weeks follow up. Similarly, the social interaction scores and the difficulties with standing / walking scores decreased from 83% to 66%, and from 100% to 82%, respectively during the same follow-up window. The reduction in the last two domains means that the patient had fewer problems with social interaction and fewer difficulties with standing / walking at 10 weeks compared to 2 weeks of follow-up.
Figure 1: Pre-Manipulation XR of Left Ankle Joint (AP View).
Figure 2: Pre-Manipulation XR of Left Ankle Joint (Lateral View).
Figure 3: Post Closed Reduction XR. (AP View).
Figure 4: Post Closed Reduction XR. (AP View).
Figure 5: Post Closed Reduction CT Scan Showing the Fractured Segment (Coronal View).
Figure 6: Post Closed Reduction CT Scan Showing the Fractured Segment (Sagittal View).
Figure 7: Intra-op Image Intensifier Showing the Guide Wires for Cannulated Screws.
Figure 8: Intra-op Image Intensifier Showing 3 Cannulated Screws.
Figure 9: CT Scan at 10 Weeks Showing Evidence of Early Bone Healing.
Figure 10: CT Scan at 10 Weeks Showing Evidence of Early Bone Healing.
Discussion
Talar fracture accounts for 2% of all lower extremities fracture and up to 5% of foot and ankle fracture [4]. Up to 60% of talus surface is covered with articular cartilage, which means that most of the talar body receives its blood supply from the vascular anastomosis around its neck [5, 6]. In the last few years, there were many reported cases of rare talar fractures. For instance, Chandramohan, reported a case of fractured posterior process of talus highlighting the importance of diagnosing these fractures which are usually misdiagnosed as an ankle sprain [7]. A case of isolated fracture of lateral tubercle of talar posterior process was described by Lunebourg & Zermatten [8]. However, up to our best knowledge, there is no reported case for fracture info-medial talar articular surface with the anterior process of the calcaneum that accompanied talo-tibial and subtalar dislocation. The Indications for surgical fixation of talar fracture and duration of non-weight bearing duration is variable in literature. Immediate reduction of talus dislocations is important to preserve arterial blood supply and to prevent swelling of surrounding soft tissue, which, in turn may compromise talus blood supply [9]. Displaced talar fracture should be treated as early as possible to reduce the risk of avascular necrosis [10]. Surgical fixation of displaced talar fractures should be followed by a period of 6-12 weeks of non-weight bearing, depending on bone quality and extent of comminution and rigidity of fixation [10].
Acknowledgment
The authors declare that no part of this study has been taken from existing published or unpublished materials without due acknowledgement and that all secondary materials used herein has been fully referenced.
We declare that this work received no financial support of any source.
Conflict of interest
No Conflict of Interest.
Funding
No source of funding.
Article Info
Article Type
Case Report & Review of LiteraturePublication history
Received: Mon 25, Mar 2019Accepted: Tue 09, Apr 2019
Published: Fri 19, Apr 2019
Copyright
© 2023 Ahmed Aljawadi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.02.015
Author Info
Ahmed Aljawadi Anand Pillai Noman Jahangir Noman Shakeel Niazi
Corresponding Author
Ahmed AljawadiTrauma and Orthopaedics, Manchester Foundation Trust, Southmoor Rd, Wythenshawe, Manchester, M23 9LT, The United Kingdom
Figures & Tables









References
- Heylen S, De Baets T, Verstraete P (2011) Closed total talus dislocation: a case report. Acta orthop Belg 77: 838-842. [Crossref]
- Donatelli RA (1987) Abnormal biomechanics of the foot and ankle. J Orthop Sports Phys Ther 9: 11-6. [Crossref]
- Morley D, Jenkinson C, Doll H, Lavis G, Sharp R, et al. (2013) The Manchester–Oxford Foot Questionnaire (MOXFQ) development and validation of a summary index score. Bone joint Res 2: 66-9. [Crossref]
- Mohammad Hosein Taraz-Jamshidi, Omid Shapari, Reza Shiravani, Saeed Moalemi, Ali Birjandinejad (2013) Simultaneous Bilateral Fracture Dislocation of the Talus: A Case Report. Trauma Mon 18: 90-94. [Crossref]
- Hama S, Onishi R, Yasuda M, Minato K, Miyashita M (2018) Adolescent talus body fracture with high displacement: A case report. Medicine (Baltimore) 97: e12043. [Crossref]
- Gelberman RH, Mortensen WW (1983) The arterial anatomy of the talus. Foot Ankle 4: 64-72. [Crossref]
- Chandramohan C (2017) A rare Case of the Posterior Process of Talus Fracture with Subtalar and Talonavicular Subluxation A Case Report. University Journal of Surgery and Surgical Specialities 3(3).
- Lunebourg A, Zermatten P (2014) Fracture of the lateral process of the talus: a report of two cases. J Foot Ankle Surg 53: 316-9. [Crossref]
- Schulze W, Richter J, Russe O, Ingelfinger P, Muhr G (2002) Surgical treatment of talus fractures: a retrospective study of 80 cases followed for 1-15 years. Acta Orthop Scand 73: 344-351. [Crossref]
- Rammelt S, Zwipp H (2009) Talar neck and body fractures. Injury 40: 120-135. [Crossref]