Systematic Review of Accelerometer Based Navigation in Total Knee Arthroplasty: Improved Alignment, Clinical Results, and Patient Reported Outcomes Compared to Conventional Guides?
A B S T R A C T
Background: There have been significant advancements to restore knee alignment postoperatively in the TKA population. This includes the use of accelerometer-based portable navigation (ABN). ABN can lead to a more precise restoration of the neutral mechanical axis, improve efficiency and potentially decrease early- and long-term complications. The degree with which ABN can achieve this remains unclear. We performed a systematic review to answer this question.
Methods: We performed a systematic review in accordance with Cochrane guidelines of controlled studies (prospective and retrospective) in MEDLINE with an emphasis on studies comparing postoperative outcomes such as mechanical axis alignment, operative time, blood loss, complications and clinical outcome scores in total knee arthroplasty patients using ABN versus conventional intramedullary guides.
Results: ABN was associated with significantly fewer outliers in hip-knee-ankle alignment (p = 0.0006), femoral component alignment (p < 0.0001). ABN was associated with significantly less estimated blood loss (p = 0.05) and no difference in operative times (p = 0.21). Finally, there was no difference regarding functional outcomes or DVT.
Conclusion: ABN more accurately achieves neutral mechanical alignment with a smaller incidence of outliers. There was not an increase in operative time with using ABN and there were reductions in blood loss as well. We conclude that ABN offers the benefit of improved mechanical alignment.
Keywords
Accelerometer-based navigation, computer-assisted navigation, total knee arthroplasty, outcomes, knee, joint
Introduction
Total knee arthroplasty is one of the most common surgical procedures performed in the United States. As of 2010, over 600,000 TKA are performed annually [1]. This number is expected to increase by over 800% by 2050 [2]. Most orthopaedic surgeons strive to achieve neutral mechanical alignment; but, the means to accurately and reproducibly achieve these results remains controversial [3-5]. Historically, many orthopaedic surgeons have performed TKA with the use of conventional intramedullary cutting guides [6, 7]. Fortunately, there have been technological advancements to address the potential for malalignment and early-term revision. Current options include custom cutting blocks, robotic-assisted navigation, computer-assisted navigation (CAS), and more recently, accelerometer-based portable navigation (ABN). Benefits touted of ABN include accuracy, portability, simplicity in design and ease of use [8, 9]. With advanced technology, there is often additional associated cost including advanced preoperative imaging, such as computed tomography or MRI.
ABN does not require advanced imaging and offers an open platform which can be utilized with any knee arthroplasty system. In addition, there is not the need for large upfront capital costs associated with utilizing large CAS based or robotic-assisted systems. Further benefits compared to conventional guides include no violation of the intramedullary canal and potentially reducing blood loss and the risk of fat embolism [10]. These accelerometer-based navigation devices use microelectromechanical systems accelerometer and gyroscope technology to reference landmarks on the distal femur allowing adjustments in both sagittal and coronal resection planes. Proponents of ABN have suggested that this can lead to a more precise restoration of the neutral mechanical axis, decrease in surgical time due to more accurate initial bone resections to achieve proper balance and decrease in patient complications due to preservation of the femoral intramedullary canal. While the results associated with CAS, custom cutting blocks and now robotic-assisted navigation have been published, few studies have looked at the results associated with ABN.
While importance has been placed on the long-term survival of TKA implant designs and their functional outcomes, early-term outcomes have become of paramount interest recently with the implementation of the comprehensive care for joint replacement (CJR) that has aimed at curbing rising economic costs of TKA while providing high-level care [11]. While modifiable risk factors such as diabetes and preoperative anemia can be addressed prior to surgery, length of stay and discharge disposition can add cost to the episode of care and affect the bundle [12]. Readmissions following TKA for medical and surgical complications such as manipulation can be “bundle busters,” and thus attempts at reducing this need to be made [13, 14]. To date, little work has been done to examine if the use of ABN can be another potentially modifiable risk factor for helping to avoid a “bundle buster” [14]. In an effort to determine if ABN achieves its purported benefits, we conducted a systematic literature review to answer the following questions in the study: Does ABN achieve neutral mechanical alignment more reliably during TKA when compared with conventional guides? Does the use of ABN lead to improved clinical results after TKA when compared with conventional guides?
Search Strategy and Criteria
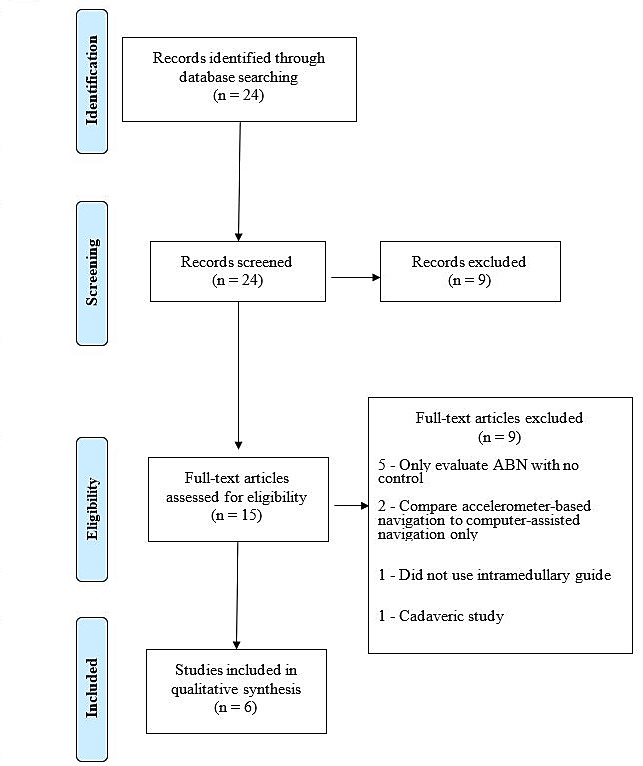
We performed a systematic review of prospective and retrospective studies related to the use of accelerometer-based portable navigation systems in total knee arthroplasty using the MEDLINE database. Relevant studies within this database were identified with the search headings: (knee (arthroplasty or replacement) and (portable navigation or accelerometer-based navigation). A literature search was performed in October 2018 and found 24 articles using MEDLINE [8-10, 15-35]. The abstracts of these articles were reviewed to determine their relevance to the study questions proposed (Figure 1). Six studies were identified and included. The lead author performed this search and the results were agreed on by all other authors. Of the six studies identified, two were Level I, one was Level II and three were Level III.
Of the six studies investigating whether portable navigation achieved neutral alignment more reliably than conventional methods, two provided Level 1 evidence, one provided Level II evidence and three provided Level III evidence [10, 27, 28, 30, 33, 35]. Finally, of the six studies investigating whether portable navigation translates to improved clinical results, one provided Level 1 evidence, one provided Level II evidence and three provided Level III evidence [10, 28, 30, 33, 35]. Studies reviewed differed with respect to their level of evidence ranging from Level I studies to Level III. The strength of the two Level I randomized control studies was verified using the modified Jaded scoring system and the included retrospective studies were evaluated with the Newcastle-Ottawa grading system [36, 37]. All included studies were thoroughly reviewed, and final conclusions were made after all authors reached a consensus.
Figure 1: The preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram for selection of studies based on inclusion criteria during systematic review.
Statistical Analysis
The outcome measures analysed for the first study question included coronal and sagittal alignment and the presence of outliers from the targeted postoperative prosthetic alignment (Table 1). For the second study question, there was a focus on the amount of blood loss, need for blood transfusion, operative time, postoperative complications including the incidence of DVT/PE, amount of blood loss and changes in knee function scores (Tables 2 & 3). Meta-analyses were performed to compare instrumentation accelerometer-based navigation (ABN) to intramedullary (IM) instrumentation using Review Manager 5.3 (The Cochrane Collaboration, The Nordic Cochrane Centre, Copenhagen).
Table 1: Summary of data regarding ABN vs. Conventional Guides for Alignment.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
Decreased outliers with portable navigation vs. conventional in the femoral coronal and sagittal planes 3% vs. 15% and 15% vs. 43% respectively (p <0.01) |
|
Moo et al., 2018 [29] |
60 |
III |
No difference in proportion of outliers in the mechanical axis (p = 0.38) |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Coronal femoral angle closer to perpendicular and fewer outliers in the femoral coronal plane only (p < 0.01) |
|
Goh et al., 2018 [26] |
114 |
II |
Improved mean mechanical axis (p = 0.018), femoral component alignment (p = 0.050), and tibial component alignment (p = 0.008), fewer mechanical axis outliers (p = 0.034) |
|
Ikawa et al., 2017 [10] |
241 |
I |
Significantly fewer patients having alignment >3° from neutral with ABN. Mean deviation from neutral significantly less with ABN. |
|
Gharaibeh et al., 2017 [23] |
179 |
I |
No difference in coronal or sagittal plane alignment |
Table 2: Summary of data for ABN vs. Conventional Guides for Blood Loss and Operative Time.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
No requirement for blood transfusion and no increase in operative time |
|
Moo et al., 2018 [29] |
60 |
III |
No difference in transfusion incidence of duration of surgery |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Decreased blood loss with no difference in duration of surgery |
|
Goh et al., 2018 [26] |
114 |
II |
No difference in duration of surgery |
|
Ikawa et al., 2017 [10] |
241 |
I |
No requirement for blood transfusion. Distal femoral resection time was longer 5.6 minutes vs. 2.9 minutes |
|
Gharaibeh et al., 2017 [23] |
179 |
I |
No difference in duration of surgery |
Table 3: Summary of data for ABN vs. Conventional Guides for Complications and Patient Reported Outcomes.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
No requirement for blood transfusion and no difference in incidence of DVT/PE |
|
Moo et al., 2018 [29] |
60 |
III |
No patients developed wound complications or major morbidity in the early post operative period (30 days) |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Less blood loss, no complications, no difference in 1-year post operative ROM, Knee society score, or knee function score |
|
Goh et al., 2018 [26] |
114 |
II |
No complications, no difference in 2-year post operative ROM, Knee society score, knee function score, or oxford knee score |
|
Ikawa et al., 2017[10] |
241 |
I |
Decreased blood loss, no requirement for transfusion, no incidence of DVT/PT |
Results
I Is Portable Navigation Able to Achieve Neutral Mechanical Alignment More Consistently During TKA?
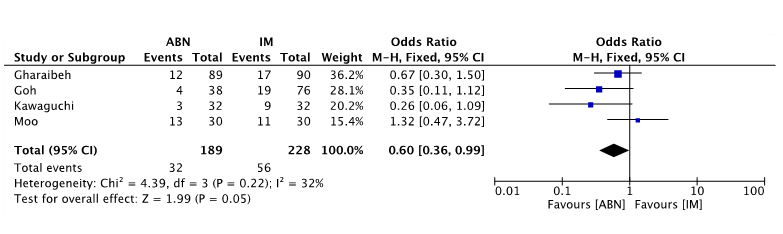
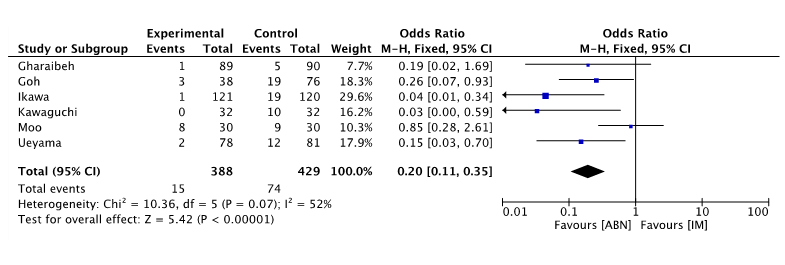
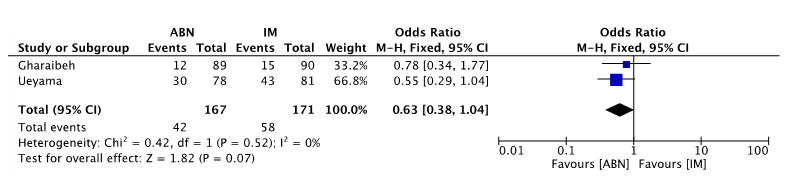
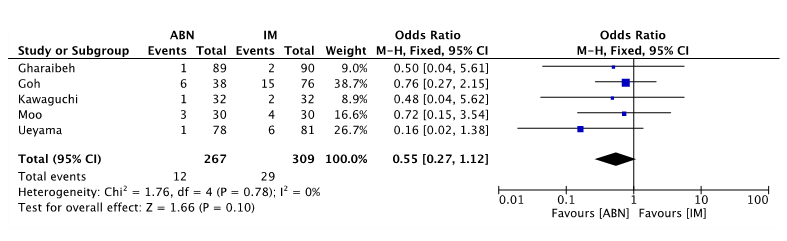
Regarding hip-knee-axis outliers, 75% of the studies found that ABN had fewer outliers compared to conventional guides [27, 28, 30]. One study did not find a difference between the ABN and conventional guides [33]. When pooling data from the included studies, ABN was associated with significantly fewer outliers in hip-knee-ankle alignment (p = 0.0006) (Figure 2). For femoral component coronal alignment, all six studies found that ABN had fewer outliers compared to conventional guides (Figure 3). Of those, 4 found statistically significant differences favoring the use of ABN to achieve coronal alignment with the distal femoral resection [10, 28, 30, 35]. When pooling the data from the included studies, ABN was associated with significantly fewer outliers for femoral coronal alignment compared to conventional guides (p<0.01).
Figure 2: Forest plot of hip-knee-ankle axis outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
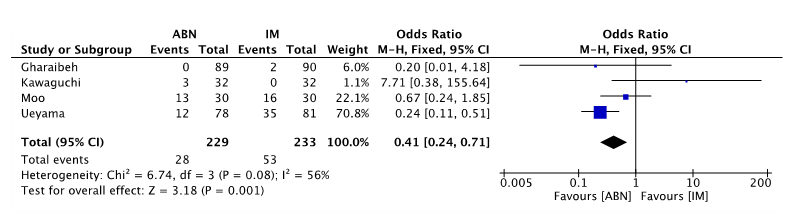
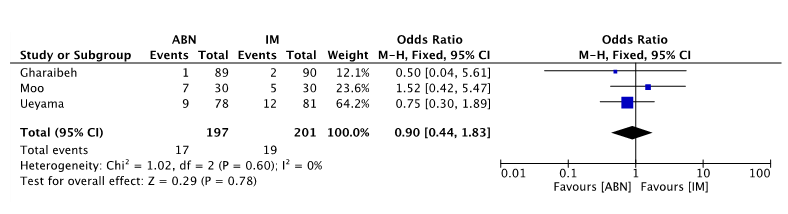
For femoral component sagittal alignment, 75% of the studies found that ABN had fewer outliers compared to conventional guides (Figure 4). Of those, one study found a statistically significant difference favoring the use of ABN to achieve proper sagittal alignment with the distal femoral resection [35]. When pooling the data from the included studies, ABN was associated with significantly fewer outliers for the femoral sagittal alignment compared to conventional guides (p<0.01). For tibial component coronal alignment, all five studies found that ABN had fewer outliers compared to conventional guides (Figure 5) [27, 28, 30, 33, 35]. However, these differences were not statistically significant. In addition, the pooled data from the included studies failed to find a difference between the two methods. For tibial component sagittal alignment, two of the three studies found that ABN had fewer outliers compared to conventional guides (Figure 6) [27, 35]. However, these differences were not statistically significant. In addition, the pooled data from the included studies failed to find a difference between the two methods.
Figure 3: Forest plot of femoral coronal alignment outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 4: Forest plot of femoral sagittal alignment outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 5: Forest plot of femoral axis alignment outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 6: Forest plot of tibial coronal alignment outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 7: Forest plot of tibial sagittal alignment outliers in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
II Does Portable Navigation Provide Any Clinical Benefit for Patients Undergoing TKA?
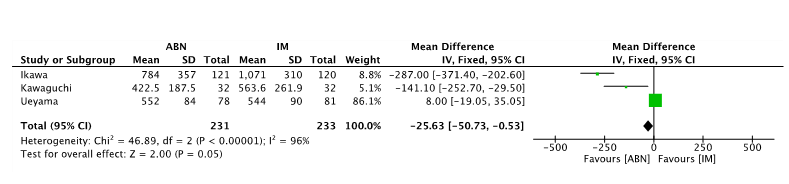
For this review, we utilized the need for transfusion and duration of surgery as a means to assess the clinical and financial benefit of using portable navigation. Previous studies have found that the raw cost per unit of blood transfused is approximately $200 and the cost of operating room use ranges from $22 to $133 [38, 39]. For blood loss, two of the three studies found that ABN had statistically significant less blood loss compared to conventional guides (Figure 7) [10, 28]. On average, ABN cases had 586.2 mL of blood loss compared to 726.2 mL. When pooling this data from the three studies, ABN was associated with significantly less blood loss compared to conventional guides (p<0.01). None of the patients in those studies required transfusion in either the ABN or conventional guides. While there was less blood loss with regard to using ABN, this did not translate into a cost savings given the lack of transfusions. For the duration of surgery, the use of ABN was found to take on average of 2.7 minutes longer compared to conventional guides. When pooling the data from the six studies, there was not a significant difference in the operative times between ABN and conventional guides (p>0.05) (Figure 8) [10, 27, 28, 30, 33, 35].
Figure 8: Forest plot of blood loss in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
III Does Portable Navigation Lead to Improved Clinical Results After TKA
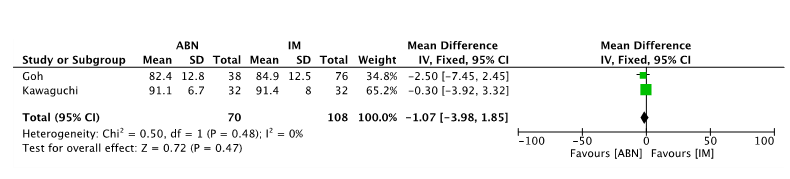
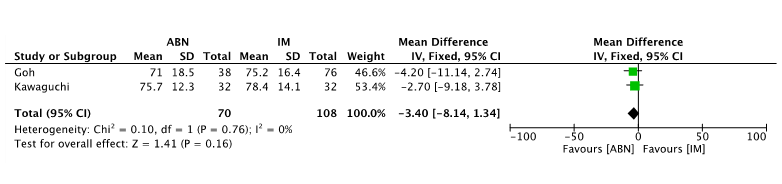
To assess clinical results, we reviewed the incidence of postoperative complications including blood loss, incidence of DVT/PE and patient-reported outcomes including knee society score and knee function score. For the three studies that evaluated for differences in DVT/PE or wound complications, there was not a significant difference between ABN and conventional guides [28, 33, 35]. When comparing ABN versus conventional guides for differences in patient reported outcomes, there were two studies that included this data [28, 30]. There was not a statistically significant difference between ABN and conventional guides regarding Knee Society Scores and Knee Function Scores. When the data was pooled between the two studies to detect a difference, there still was not a significant difference between the two resection methods about patient outcomes (Figures 9-11).
Figure 9: Forest plot of total operative time in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 10: Forest plot of Knee Society Scores in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Figure 11: Forest plot of Knee Function Scores in accelerometer-based navigation (ABN) versus intramedullary guide (IM).
Discussion
Previous studies have demonstrated that mechanical alignment, specifically achieving a neutral mechanical axis, is crucial for a successful total knee arthroplasty [3, 40]. The most common practice during arthroplasty is the use of an extramedullary tibial alignment guide and an intramedullary femoral alignment guide [41]. Previous studies have shown that these guides may not consistently provide the most accurate knee alignment [6, 31]. A meta-analysis by Mason et al. demonstrated that computer-assisted resections achieved femoral varus/valgus alignment and tibial varus/valgus alignment closer to the mechanical axis than conventional methods [6]. Unfortunately, these computer-assisted navigation systems have many drawbacks including a long learning curve, longer operative times and increased costs [9, 23]. These issues with CAS have led to the development of accelerometer-based navigation systems.
A previous study by Goh et al. found that compared to CAS, ABN cost significantly less, has a shorter learning curve, and reduces operative times [23]. Thus, in an attempt to determine if this new technology can provide benefit, we performed a systematic review to determine the validity that ABN can achieve more reliable mechanical alignment and improved clinical results while being a cost-effective solution. As with any study, the current work has limitations. The first limitation is a small sample size of included articles in this review. The literature on accelerometer-based navigation is sparse which contributed to our small number of studies. Furthermore, of the six included studies, only two were Level 1 evidence. With any systematic review, each included study is subject to inherent bias. These biases can potentially affect the synthesis of ultimate conclusions.
Finally, all the included studies were authored by high volume arthroplasty surgeons which, when comparing the difference in operative time or incidence of mechanical axis outliers between ABN and conventional methods, would not be as readily apparent as when compared to low-volume surgeons. As with any newer technology, there could also be a learning curve to adopting newer technology such as ABN. Thus, the potential advantages of using ABN by these experienced surgeons who were accustomed to using conventional methods could have introduced some learning curve bias into the results and impeded some of the potential advantages of ABN. Regarding whether ABN provides a proven benefit over conventional guides for postoperative alignment, ABN was found to have improved long-leg alignment compared to conventional guides. In addition, the femoral coronal and sagittal alignments were more accurate compared to conventional guides.
As Fang et al. demonstrated that coronal malalignment following total knee arthroplasty can lead to lower survival rates, the importance of achieving proper coronal alignment has long-term consequences on revision rates [4]. While the importance of sagittal alignment should not be disregarded, sagittal malalignment can often be better tolerated by the patient as this lies in the flexion/extension arc of the limb and thus, outliers are often tolerated by the patient. These outliers typically do not have an effect on their functional outcome and not affect the long-term survival of the implant. However, varus and valgus outliers for coronal alignment can lead to improper ligament tension and lead to potentially increased loading to the implants [4]. Besides the potential for increased revision rates as a result of malalignment, malalignment can also lead to instability [42]. The ability to achieve proper balance at the conclusion of the procedure revolves around proper femoral and tibial resections with soft tissue releases. Inaccurate distal femoral resections can lead to coronal instability. The use of conventional guides for the distal femoral resection is challenging and there is variability in the valgus angle needed to restore proper alignment [43, 44].
The ability to accommodate for different femoral neck offsets and precisely target a specific distal femoral resection angle has the potential to obviate malalignment related revision. Nam et al. demonstrated that using ABN was found to have over 95% accuracy regarding the femoral mechanical axis and there was only 0.83o variance in a cadaveric study between a preoperative target and actual alignment when using ABN [8, 18]. Thus, as our review found, the use of ABN achieves more accurate long-leg alignment with fewer outliers, especially with the distal femoral resection. With total knee arthroplasty being performed in the outpatient setting, reducing potential complications including blood transfusions or fractures has become even more important [45]. As discussed earlier, the use of ABN was associated with fewer sagittal alignment outliers.
While a sagittal alignment for the femoral component is often tolerated by the patient, if a severe extension of the femoral implant occurs, this often is associated with a notch in the anterior femoral cortex. This can lead to the weakening of the distal femur and potential for supracondylar femur fracture [46]. Besides this potential complication, ABN also does not violate the canals of the femur or the tibia. As our study found significant reductions in blood loss with ABN, this can potentially reduce the incidence of painful hematomas or wound drainage. While there was not a difference in the need for transfusion, the use of ABN for those performing tourniquetless knee arthroplasty might see a larger need to use ABN to avoid increases in blood loss and potential for transfusion due to increased intraoperative blood loss [47]. Further studies are needed to evaluate this potential benefit of ABN in tourniquetless TKA.
The use of computer-assisted navigation is often associated with longer surgical times [48]. However, our study failed to find a significant difference in operative times between ABN and conventional guides. The use of ABN was associated with an average of 2.7 minutes longer compared to conventional guides. While ABN might not be timesaving during the operation itself, the unseen advantage of using ABN is the potential for fewer instrument trays needed for the procedure. Similar to those using patient-specific instrumentation (PSI), ABN requires opening the 4-1 femoral cutting block without the need to open additional instrument pans for the distal femur and tibial cuts. Thus, the femoral cutting block can be peel packed and opened once the proper size is determined. Similarly, the tibial baseplate can be opened once sizing is determined. The time savings can come from fewer instrument trays that need to be turned over between cases [49, 50]. The reduced costs associated with a reduction in instrument turnover is one of the potential hidden savings with using ABN and is the study of further research.
There is an associated cost with using ABN, much like there are associated capital costs with using CAS. ABN is not associated with the large upfront costs, but the use of these navigation units can be substantial. Our institutional use of ABN is associated with an increased cost of $600 per case. In an era of bundled payments, clinical benefit needs to be demonstrated to prove its use as any additional cost will affect the overall costs within the episode of care [12]. Our study did not find improvements in the patient-reported outcomes and it remains to be seen if ABN can reduce readmissions within this new era of cost containment and avoid the “bundle buster”. There is the potential to be reimbursed for the use of ABN as CPT coding allows for the use of 20985, which is the code used for computer-assisted navigation for a musculoskeletal procedure, imageless. This is associated with an RVU amount of 2.5. Thus, there is potential to help offset the cost associated with the use of ABN.
In summary, we believe that valid conclusions can be drawn from this review. Based on this systematic review, it appears that when compared to conventional methods, ABN more accurately achieves neutral mechanical alignment and femoral coronal and sagittal component alignment with a smaller incidence of outliers. Compared to conventional instrumentation, ABN had less blood loss and equivalent operative time. Further research is needed to determine if there is potential for ABN to be cost-effective with reduced readmissions in the early-term and reduced revisions in the long-term to justify its cost associated with use.
Article Info
Article Type
Review ArticlePublication history
Received: Tue 23, Jun 2020Accepted: Wed 08, Jul 2020
Published: Wed 15, Jul 2020
Copyright
© 2023 Stephen T. Duncan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSR.2020.01.05
Author Info
Stephen T. Duncan Cale Jacobs Lucian Warth Syed K. Mehdi
Corresponding Author
Stephen T. DuncanDepartment of Orthopaedic Surgery, University of Kentucky, Lexington, Kentucky, USA
Figures & Tables
Table 1: Summary of data regarding ABN vs. Conventional Guides for Alignment.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
Decreased outliers with portable navigation vs. conventional in the femoral coronal and sagittal planes 3% vs. 15% and 15% vs. 43% respectively (p <0.01) |
|
Moo et al., 2018 [29] |
60 |
III |
No difference in proportion of outliers in the mechanical axis (p = 0.38) |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Coronal femoral angle closer to perpendicular and fewer outliers in the femoral coronal plane only (p < 0.01) |
|
Goh et al., 2018 [26] |
114 |
II |
Improved mean mechanical axis (p = 0.018), femoral component alignment (p = 0.050), and tibial component alignment (p = 0.008), fewer mechanical axis outliers (p = 0.034) |
|
Ikawa et al., 2017 [10] |
241 |
I |
Significantly fewer patients having alignment >3° from neutral with ABN. Mean deviation from neutral significantly less with ABN. |
|
Gharaibeh et al., 2017 [23] |
179 |
I |
No difference in coronal or sagittal plane alignment |
Table 2: Summary of data for ABN vs. Conventional Guides for Blood Loss and Operative Time.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
No requirement for blood transfusion and no increase in operative time |
|
Moo et al., 2018 [29] |
60 |
III |
No difference in transfusion incidence of duration of surgery |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Decreased blood loss with no difference in duration of surgery |
|
Goh et al., 2018 [26] |
114 |
II |
No difference in duration of surgery |
|
Ikawa et al., 2017 [10] |
241 |
I |
No requirement for blood transfusion. Distal femoral resection time was longer 5.6 minutes vs. 2.9 minutes |
|
Gharaibeh et al., 2017 [23] |
179 |
I |
No difference in duration of surgery |
Table 3: Summary of data for ABN vs. Conventional Guides for Complications and Patient Reported Outcomes.
|
Author & Year |
Sample Size |
Level of Evidence |
Conclusion |
|
Ueyama et al., 2018 [31] |
159 |
III |
No requirement for blood transfusion and no difference in incidence of DVT/PE |
|
Moo et al., 2018 [29] |
60 |
III |
No patients developed wound complications or major morbidity in the early post operative period (30 days) |
|
Kawaguchi et al., 2017 [24] |
67 |
III |
Less blood loss, no complications, no difference in 1-year post operative ROM, Knee society score, or knee function score |
|
Goh et al., 2018 [26] |
114 |
II |
No complications, no difference in 2-year post operative ROM, Knee society score, knee function score, or oxford knee score |
|
Ikawa et al., 2017[10] |
241 |
I |
Decreased blood loss, no requirement for transfusion, no incidence of DVT/PT |

References
- Cram P, Lu X, Kates SL, Singh JA, Li Y et al. (2012) Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA 308: 1227-1236. [Crossref]
- Inacio MCS, Paxton EW, Graves SE, Namba RS, Nemes S (2017) Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage 25: 1797-1803. [Crossref]
- Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM et al. (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428: 26-34. [Crossref]
- Fang DM, Ritter MA, Davis KE (2009) Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 24: 39-43. [Crossref]
- Schiraldi M, Bonzanini G, Chirillo D, de Tullio V (2016) Mechanical and kinematic alignment in total knee arthroplasty. Ann Transl Med 4: 130. [Crossref]
- Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K (2007) Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty 22: 1097-1106. [Crossref]
- Pang CH, Chan WL, Yen CH, Cheng SC, Wo SB et al. (2009) Comparison of total knee arthroplasty using computer-assisted navigation versus conventional guiding systems: a prospective study. J Orthop Surg (Hong Kong) 17: 170-173. [Crossref]
- Nam D, Jerabek SA, Cross MB, Mayman DJ (2012) Cadaveric analysis of an accelerometer-based portable navigation device for distal femoral cutting block alignment in total knee arthroplasty. Comput Aided Surg 17: 205-210. [Crossref]
- Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB et al. (2013) Accelerometer-based, portable navigation vs imageless, large-console computer-assisted navigation in total knee arthroplasty: a comparison of radiographic results. J Arthroplasty 28: 255-261. [Crossref]
- Ikawa T, Takemura S, Kim M, Takaoka K, Minoda Y et al. (2017) Usefulness of an accelerometer-based portable navigation system in total knee arthroplasty. Bone Joint J 99-B: 1047-1052. [Crossref]
- Centers for Medicare & Medicaid Services (CMS), HHS (2018) Medicare Program; Changes to the Comprehensive Care for Joint Replacement Payment Model (CJR): Extreme and Uncontrollable Circumstances Policy for the CJR Model. Final rule. Fed Regist 83: 26604-26610. [Crossref]
- Clair AJ, Evangelista PJ, Lajam CM, Slover JD, Bosco JA et al. (2016) Cost Analysis of Total Joint Arthroplasty Readmissions in a Bundled Payment Care Improvement Initiative. J Arthroplasty 31: 1862-1865. [Crossref]
- Yu S, Garvin KL, Healy WL, Pellegrini VD Jr, Iorio R (2016) Preventing Hospital Readmissions and Limiting the Complications Associated With Total Joint Arthroplasty. Instr Course Lect 65: 199-210. [Crossref]
- Wodowski AJ, Pelt CE, Erickson JA, Anderson MB, Gililland JM et al. (2019) 'Bundle Busters': Who Is at Risk of Exceeding the Target Payment and Can They Be Optimized? Bone Joint J 101-B: 64-69. [Crossref]
- Nam D, Cross M, Deshmane P, Jerabek S, Kang M et al. (2011) Radiographic results of an accelerometer-based, handheld surgical navigation system for the tibial resection in total knee arthroplasty. Orthopedics 34: e615-e621. [Crossref]
- Nam D, Jerabek SA, Haughom B, Cross MB, Reinhard KR et al. (2011) Radiographic analysis of a hand-held surgical navigation system for tibial resection in total knee arthroplasty. J Arthroplasty 26: 1527-1533. [Crossref]
- Nam D, Dy CJ, Cross MB, Kang MN, Mayman DJ (2012) Cadaveric results of an accelerometer based, extramedullary navigation system for the tibial resection in total knee arthroplasty. Knee 19: 617-621. [Crossref]
- Nam D, Nawabi DH, Cross MB, Heyse TJ, Mayman DJ (2012) Accelerometer-based computer navigation for performing the distal femoral resection in total knee arthroplasty. J Arthroplasty 27: 1717-1722. [Crossref]
- Bugbee WD, Kermanshahi AY, Munro MM, McCauley JC, Copp SN (2014) Accuracy of a hand-held surgical navigation system for tibial resection in total knee arthroplasty. Knee 21: 1225-1228. [Crossref]
- Nam D, Cody EA, Nguyen JT, Figgie MP, Mayman DJ (2014) Extramedullary guides versus portable, accelerometer-based navigation for tibial alignment in total knee arthroplasty: a randomized, controlled trial: winner of the 2013 HAP PAUL award. J Arthroplasty 29: 288-294. [Crossref]
- Huang EH, Copp SN, Bugbee WD (2015) Accuracy of A Handheld Accelerometer-Based Navigation System for Femoral and Tibial Resection in Total Knee Arthroplasty. J Arthroplasty 30: 1906-1910. [Crossref]
- Iorio R, Mazza D, Drogo P, Bolle G, Conteduca F et al. (2015) Clinical and radiographic outcomes of an accelerometer-based system for the tibial resection in total knee arthroplasty. Int Orthop 39: 461-466. [Crossref]
- Goh GS, Liow MHL, Lim WS, Tay DK, Yeo SJ et al. (2016) Accelerometer-Based Navigation Is as Accurate as Optical Computer Navigation in Restoring the Joint Line and Mechanical Axis After Total Knee Arthroplasty: A Prospective Matched Study. J Arthroplasty 31: 92-97. [Crossref]
- Keeney JA (2016) Innovations in Total Knee Arthroplasty: Improved Technical Precision, But Unclear Clinical Benefits. Orthopedics 39: 217-220. [Crossref]
- Steinhaus ME, McLawhorn AS, Richardson SS, Maher P, Mayman DJ (2016) Handheld Navigation Device and Patient-Specific Cutting Guides Result in Similar Coronal Alignment for Primary Total Knee Arthroplasty: A Retrospective Matched Cohort Study. HSS J 12: 224-234. [Crossref]
- Fujimoto E, Sasashige Y, Nakata K, Yokota G, Omoto T et al. (2017) Technical Considerations and Accuracy Improvement of Accelerometer-Based Portable Computer Navigation for Performing Distal Femoral Resection in Total Knee Arthroplasty. J Arthroplasty 32: 53-60. [Crossref]
- Gharaibeh MA, Solayar GN, Harris IA, Chen DB, MacDessi SJ (2017) Accelerometer-Based, Portable Navigation (KneeAlign) vs Conventional Instrumentation for Total Knee Arthroplasty: A Prospective Randomized Comparative Trial. J Arthroplasty 32: 777-782. [Crossref]
- Kawaguchi K, Michishita K, Manabe T, Akasaka Y, Higuchi J (2017) Comparison of an Accelerometer-Based Portable Navigation System, Patient-Specific Instrumentation, and Conventional Instrumentation for Femoral Alignment in Total Knee Arthroplasty. Knee Surg Relat Res 29: 269-275. [Crossref]
- Ueyama H, Matsui Y, Minoda Y, Matsuura M, Nakamura H (2017) Using Accelerometer-Based Portable Navigation to Perform Accurate Total Knee Arthroplasty Bone Resection in Asian Patients. Orthopedics 40: e465-e472. [Crossref]
- Goh GS, Liow MHL, Tay DK, Lo N, Yeo S et al. (2018) Accelerometer-Based and Computer-Assisted Navigation in Total Knee Arthroplasty: A Reduction in Mechanical Axis Outliers Does Not Lead to Improvement in Functional Outcomes or Quality of Life When Compared to Conventional Total Knee Arthroplasty. J Arthroplasty 33: 379-385. [Crossref]
- Jones CW, Jerabek SA (2018) Current Role of Computer Navigation in Total Knee Arthroplasty. J Arthroplasty 33: 1989-1993. [Crossref]
- Matsumoto K, Ogawa H, Fukuta M, Mori N, Akiyama H (2018) Comparative Study for Alignment of Extramedullary Guides versus Portable, Accelerometer-Based Navigation in Total Knee Arthroplasty. J Knee Surg 31: 92-98. [Crossref]
- Moo IH, Chen JYQ, Chau DHH, Tan SW, Lau ACK et al. (2018) Similar radiological results with accelerometer-based navigation versus conventional technique in total knee arthroplasty. J Orthop Surg (Hong Kong) 26: 2309499018772374. [Crossref]
- Shoji H, Teramoto A, Suzuki T, Okada Y, Watanabe K et al. (2018) Radiographic assessment and clinical outcomes after total knee arthroplasty using an accelerometer-based portable navigation device. Arthroplast Today 4: 319-322. [Crossref]
- Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K et al. (2018) An accelerometer-based portable navigation system improved prosthetic alignment after total knee arthroplasty in 3D measurements. Knee Surg Sports Traumatol Arthrosc 27: 1580-1586. [Crossref]
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ et al. (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17: 1-12. [Crossref]
- Lo CK, Mertz D, Loeb M (2014) Newcastle-Ottawa Scale: Comparing Reviewers' to Authors' Assessments. BMC Med Res Methodol 14: 45. [Crossref]
- Shippert RD (2005) A study of time-dependent operating room fees and how to save $100,000 by using time-saving produts. Am J Costmetic Surg 22: 25-34.
- Toner RW, Pizzi L, Leas B, Ballas SK, Quigley A et al. (2011) Costs to hospitals of acquiring and processing blood in the US: a survey of hospital-based blood banks and transfusion services. Appl Health Econ Health Policy 9: 29-37. [Crossref]
- Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92: 2143-2149. [Crossref]
- Moon YW, Han J, Lee K, Jang SW, Seo J (2013) Clinical Outcome of IM-Guided Total Knee Arthroplasty with Inappropriate Femoral Resection in Coronal Plane. Knee Surg Relat Res 25: 19-24. [Crossref]
- Le DH, Goodman SB, Maloney WJ, Huddleston JI (2014) Current modes of failure in TKA: infection, instability, and stiffness predominate. Clin Orthop Relat Res 472: 2197-2200. [Crossref]
- Zhou K, Ling T, Xu Y, Li J, Yu H, Wang H et al. (2018) Effect of individualized distal femoral valgus resection angle in primary total knee arthroplasty: A systematic review and meta-analysis involving 1300 subjects. Int J Surg 50: 87-93. [Crossref]
- Nam D, Vajapey S, Haynes JA, Barrack RL, Nunley RM (2016) Does Use of a Variable Distal Femur Resection Angle Improve Radiographic Alignment in Primary Total Knee Arthroplasty? J Arthroplasty 31: 91-96. [Crossref]
- Crawford DA, Adams JB, Berend KR, Lombardi AV Jr (2019) Low complication rates in outpatient total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28: 1458-1464. [Crossref]
- Lesh ML, Schneider DJ, Deol G, Davis B, Jacobs CR et al. (2000) The consequences of anterior femoral notching in total knee arthroplasty. A biomechanical study. J Bone Joint Surg Am 82: 1096-1101. [Crossref]
- Zhou K, Ling T, Wang H, Zhou Z, Shen B et al. (2017) Influence of tourniquet use in primary total knee arthroplasty with drainage: a prospective randomised controlled trial. J Orthop Surg Res 12: 172. [Crossref]
- Hsu RW, Hsu W, Shen W, Hsu W, Chang S (2019) Comparison of Computer-Assisted Navigation and Conventional Instrumentation for Bilateral Total Knee Arthroplasty: The Outcomes at Mid-Term Follow-Up. Medicine (Baltimore) 98: e18083. [Crossref]
- Hamilton WG, Parks NL, Saxena A (2013) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplasty 28: 96-100. [Crossref]
- Noble JW Jr, Moore CA, Liu N (2012) The value of patient-matched instrumentation in total knee arthroplasty. J Arthroplasty 27: 153-155. [Crossref]
