Journals
Suboccipital Endoscopic Key Hole Approach for Pilocytic Astrocytoma by Fluorescein Guide
A B S T R A C T
There are no reports of full endoscopic approach for midline vermian pilocytic astrocytoma by suboccipital endoscopic key hole approach and there are only one previously study about use of fuorescein in benign neuroepithelial primary brain tumors. We reported a patient treated previously in other centers for upper vermian paraventricular pilocytic astrocytoma that was operated by suboccipital full endoscopic approach using a high-dose fluorescein-sodium (20mg/kg) with a standard could light for resection. We concluded that the suboccipital key hole endoscopic approach is a good alternative for vermian and IV ventricle tumors in selected cases of partial vermis absent caused by previous surgeries or tumors cysts extension and offers a unique and detailed anatomic perspective. High doses of intravenous fluorescein-sodium seem to be a useful intraoperative technique for delineation of pilocytic astrocytoma.
Highlights:
Cerebellar pilocytic astrocytoma represent a benign tumor
Minimally invasive surgery constitutes a good alternative in selected patients.
Intravenous fluorescein – sodium improves delineation and resection of the lesion.
K E Y W O R D S
Endoscopic approach, fluorescein, fourth ventricle, suboccipital approach, pilocytic astrocytoma
Introduction
Infratentorial supracerebellar microsurgical approach was previously described for fourth ventricle or cerebellar lesions [1]. On the other hand, this approach was effective in pineal lesions and there are reports using a pure endoscopic approach [2-4]. However, there are no reports of full endoscopic approach for midline vermian pilocytic astrocytoma by infratentorial supracerebellar or suboccipital endoscopic approach. Successful use of high-dose of fluorescein-sodium (20mg/kg) with a standard light microscope for resection of malignant Central Nervous System tumors was reported [5]. However, there are only one previously study about use of fluorescein in benign neuroepithelial primary brain tumors with contrast enhancement [6].
The aim of our paper was to report the effectiveness of suboccipital full endoscopic approach for a vermian pilocytic astrocytoma and the successful use of high-dose fluorescein-sodium (20mg/kg) with a standard could light for resection.
Case Report
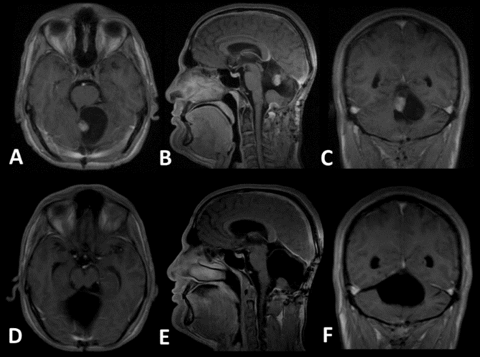
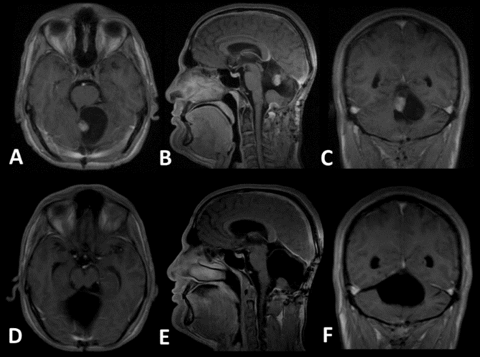
A 36-years-old male patient, with a previous history of partial microsurgical resection in other center 3 months ago, for cerebellar pilocytic astrocytoma, is presented. He suffered severe truncal ataxia and progressive suboccipital headache. There was no nystagmus or other associated neurological abnormality. Ophthalmological review and fundoscopy was normal. Magnetic Resonance Image (RMI) shows a large cystic lesion in cerebellar vermis and a mural nodule in fourth ventricle roof iso-intense on T1- weighted images and intense gadolinium enhancement of the nodule (Figure: 1, A-C).
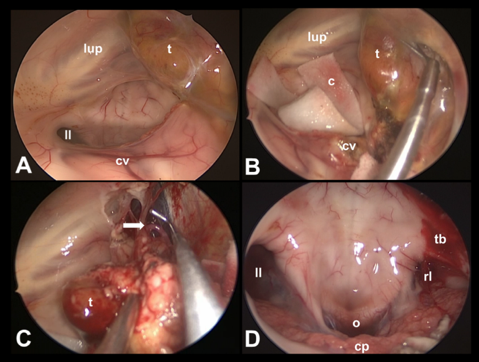
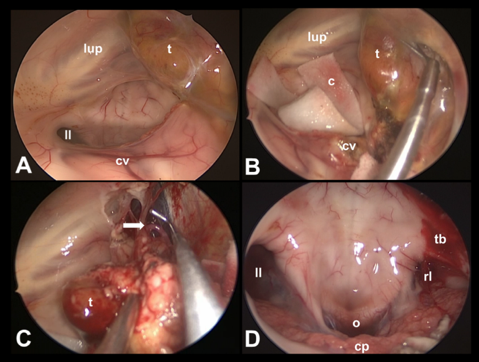
Selection of infratentorial approach was based in the localization of tumor nodule in superior vermis adherent to superior half of IV ventricle floor. The patient was placed in the semi-sitting position. Right internal jugular venous catheter was applied for the detection and treatment of air embolism during surgery. Cefazoline was used as antibiotic prophylaxis. We don’t use cisternal opening with cerebrospinal fluid drainage or preoperative lumbar drain placement because of the long cystic component and partial absence of vermian tissue that offer a wide surgical corridor. We used 20% fluorescein-sodium (20 mg per Kg) IV prior durotomy in order to identify the nodule easier in the context of a re-intervention (Figure: 2). Complete resection of the yellow well demarcated paraventricular nodule was achieved confirmed by postoperative control MRI study (Figure: 1, D-F). The histopathological exam confirms a pilocytic astrocytoma (OMS grade I) and did not find tumor tissue in the perilesional fluorescein-sodium negative tissue. We did not observe complications related to the use of high dose fluorescein-sodium.
Surgical bleeding was less than 200 ml and surgical time was 190 minutes. There were not trans operative or postoperative complications. The patient was extubated in the operating room and pass the first 24 hours in Intensive Care Unit. The 24 hours CT scan show bilateral pneumoencephalus and surgical field without hematoma or other complications. Preoperative troncular ataxia improves dramatically 48 hours after surgery (Figure: 3). The hospital stay was 5 days.
Figures

Discussion
Surgical approach
The infratentorial supracerebellar approach was originally reported by Victor Horsley in 1910 and popularized by Stein using a microsurgical technique [7, 8]. However, this approach was not exclusive for pineal region. Zapletal in 1956 described four cases operated by this corridor including a malignant astrocytoma and a meduloblastoma of the upper vermis [9]. Authors decided using this approach due the upper vermian localization of the lesion next to fourth ventricle floor and the wide corridor favored by previously microsurgical approach and the cystic component of the tumor. However, they prefer to use the therm “Suboccipital Approach” due the absence of most of cerebellar vermis.
This approach can be done in different positions. Sitting position was chosen because gravity works in the surgeon’s favor by reducing pooling of blood in the operative field and by facilitating dissection of the tumor [10]. There was not air embolism or other complications related to these positions. Low risk of air embolism was previously demonstrated for other authors in spite of the head elevation [11]. We observed a significant but not tension and asymptomatic pneumoencephalus in a postoperative 24 hours CT scan. Other authors prefer prone positions because it is less likely to experience air embolism, tension pneumoencephalus, postoperative pain, nausea, and hospitalization time. However, we did not find those events.
We selected endoscopic visualization because their better light intensity extended viewing angle and clear depiction of details within the narrow surgical field resulting in improved surgical orientation and safety in a previously microsurgical failed approach to tailor a complete resection of the nodule. We don’t use an endoscope holder due the fact that dynamic magnification provided by an assistant with continuously readjustment of the surgical target decreased the surgical time and facilitated a dynamic and effective team work. This philosophy was previously described in other full endoscopic approaches [12]. However, this strategy requires a surgical team experience but facilitated a learning curve with two surgeons working together.
Fluorescein-sodium use
Fluorescein-sodium is a fluorophore that has been increasingly used and researched in neuro-oncologic surgery since the late 1990s [13]. The principle of brain tumor staining consists in the accumulation of fluorescein in brain tumors with impaired blood-brain barrier. Successful use of high-dose fluorescein-sodium (20mg/kg) with a standard light microscope for resection of high-grade gliomas, meningiomas, hemangioblastoma and metastases has been reported [14]. Recently Minkin et al., reported for the first time the usefulness of high-dose fluorescein in patients operated on for benign neuroepithelial brain tumors (grade I WHO tumors) with contrast enhancement on magnetic resonance imaging [15].
We decided using fluorescein to observe a nodule enhancement in a previously operated surgical field. We observed an intense contrast enhancement and a good delineation of the lesion that facilitated the tumor dissection of right upper cerebellar peduncle and fourth ventricle.
Endoscopic anatomy of the fourth ventricle
There are two routes of fourth ventricle endoscopic approach described: during a transacueductal endoscopic approach and during transtelovelar endoscopic approach [16, 17]. The first offer a wider view but have the limitation of less resolution image because it uses a flexible endoscope (fiberscope) [16]. In the other hand, the transtelovelar approach using a rode endoscope lens show a more resolution image but the exposed area of fourth ventricle floor are limited compared to the approach reported in this particular case. In this report authors use an infratentorial supracerebellar approach with rod lens endoscopes in a partial absent cerebellar vermis. These factors offer a better and unique visualization in terms of resolution, anatomic orientation and panoramic view only seen in previous reports in cadaveric studies but not in live patient.
Microsurgical anatomy of the fourth ventricle has been comprehensively addressed by classic descriptions of this complex region [18]. Neuroendoscopy has been offer a new, somewhat different perspective of the "inside" view of the fourth ventricle but only by the endoscopic transaqueductal approach [16]. There are at least 23 superficial structures clearly identifiable in the fourth ventricle in neuroanatomy studies that represents the comparative basis of parallel endoscopic anatomy during the fourth ventricle endoscopic surgery [16, 18]. We were identified the following anatomical structures: median sulcus, median eminence, facial colliculus, striae medullaris, auditory tubercle, choroid plexus, inferior fovea, hypoglossal and vagal triangles, area postrema, obex, canalis medullaris, lateral recess, and the foramina of Luschka and Magendie. The locus coeruleus could not be seen as other authors’ reports during transacueductal approach [16].
Conclusion
The suboccipital endoscopic key hole approach is a good alternative for vermian and IV ventricle tumors in selected cases of partial vermis absent caused by previous surgeries or tumors cysts extension and offers a unique and detailed anatomic perspective. High doses intravenous fluorescein-sodium seems to be a useful intraoperative technique for delineation of pilocytic astrocytoma.
Article Info
Article Type
Case ReportPublication history
Received 14 May, 2018Accepted 24 May, 2018
Published 9 July, 2018
Copyright
© 2018 Joel Caballero García. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.02.002
Author Info
Corresponding author
Joel Caballero GarcíaNational Institute of Oncology and Radiobiology, 23 street Number 301 Apto C-12, Vedado, La Habana, PC: 10 400, Cuba
Figures & Tables

References
1. Matsushima T (2015) Midline Suboccipital Approach and Its Variations for Fourth Ventricular or Cerebellar Hemispheric Lesions. In: Microsurgical Anatomy and Surgery of the Posterior Cranial Fossa. Springer 57-71.
2. Kuan-Yin T, Hsin-I M, Wei-Hsiu L, Chi-Tun T (2012) Endoscopic Supracerebellar Infratentorial Retropineal Approach for Tumor Resection. World Neurosurg 77: 399-E1-399-E4. [Crossref]
3. Thaher F, Kurucz P, Fuellbier L, Bittl M, Hopf NJ (2014) Endoscopic surgery for tumors of the pineal region via a paramedian infratentorial supracerebellar keyhole approach (PISKA). Neurosurg Rev 37: 677-684. [Crossref]
4. Sughrue ME (2011) Minimally Invasive Approaches to the Pineal Region. Neurosurg Clin N Am 22: 381-384. [Crossref]
5. Schebesch KM, Brawanski A, Hohenberguer C, Höhne J (2016) Fluorescein Sodium-Guided Surgery of Malignant Brain Tumors: History, Current Concepts, and Future Projects. Turk Neurosurg 26: 185-194. [Crossref]
6. Minkin K, Naydenov E, Gabrovski K, Dimova P, Penkov M, et al. (2016) Intraoperative fluorescein staining for benign brain tumors. Clin Neurol Neurosurg 149: 22-26. [Crossref]
7. Horsley V (1910) Discussion of paper by CMH Howell on tumors of the pineal body. Proc R Soc Med 3: 77-78.
8. Stein BM (1971) The infratentorial supracerebellar approach to pineal lesions. J Neurosurg 35: 197-202. [Crossref]
9. Zapletal B (1956) Ein neuer operativer Zugang zum Gebiet der Incisura tentorii. Zentralbl Neurochir 16: 64-69.
10. Kennedy BC, Bruce JN (2011) Surgical Approaches to the Pineal Region Neurosurg Clin N Am 22: 367-380.
11. Uschold T, Abla AA, Fusco D, Bristol RE, Nakaji P (2011) Supracerebellar infratentorial endoscopically controlled resection of pineal lesions: case series and operative technique. J Neurosurg Pediatr 8: 554-564. [Crossref]
12. Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL (2005) Expanded endonasal approach: the rostrocaudal axis: part I. Crista galli to the sella turcica. Neurosurg Focus 19: 3. [Crossref]
13.Kuroiwa T, Kajimoto Y, Ohta T (1988) Development of a fluorescein operative microscope for use during malignant glioma surgery: A technical note and preliminary report. Surg Neurol 50: 41-48. [Crossref]
14. Ung TH, Kellner C, Neira JA, Wang SH, D'Amico R, et al. (2015) The use of fluorescein sodium in the biopsy and gross-total resection of a tectal plate glioma. J Neurosurg Pediatr 16: 732-735. [Crossref]
15. Minkin K, Naydenov E, Gabrovski K, Dimova P, Penkov M, et al. (2016) Intraoperative fluorescein staining for benign brain tumors. Clin Neurol Neurosurg 149: 22-26. [Crossref]
16. Longatti P, Fiorindi A, Feletti A, D'Avella D, Martinuzzi A (2008) Endoscopic anatomy of the fourth ventricle. J Neurosurg 109: 530-535. [Crossref]
17. Di Leva A, Komatsu M, Komatsu F, Tschabitscher M (2012) Endoscopic telovelar approach to the fourth ventricle: anatomic study. Neurosurg Rev 35: 341-349. [Crossref]
18. Rhoton AL Jr (2003) Rhoton’s Cranial Anatomy and Surgical Approaches. Philadelphia: Lippincott Williams & Wilkins.
