Journals
Sub-acute physical and mental decline associated with abnormally hypercalcemia: the case report of an oldest-old woman saved by surgery
A B S T R A C T
Background: the case of an oldest-old woman with severe hypercalcemia and hyperparathyroidism due to left parathyroid adenoma.
Case presentation: An 85-year-old woman, hospitalized for rapid loss of functional abilities, mental confusion, worsening of depression, anorexia and incontinence. In the medical history, she had depression, hypertension, osteopenia and osteoarthritis. Blood examinations showed high levels of calcium and intact parathyroid hormone (PTHi), severe renal failure with hyperphosphoremia. After hydration and loop diuretic administration, renal function improved and pamidronate and calcimimetic treatments were followed by reduction of calcium levels. The ultrasound of neck identified a possible parathyroid adenoma; 99Tc-sestamibi scintigraphy and CT scan with contrast confirmed the diagnosis. The surgical left hemithyroidectomy was the treatment of choice and the PTHi and calcium reached normal circulating levels immediately post-surgery. At the 3-month clinical follow-up from surgery, the functional, psychological and cognitive functions improved substantially, although mood disorder secondary to disability persisted.
Conclusions: Hypercalcemia due to primary hyperparathyroidism is a low prevalence condition among older adults. However, we should keep in mind whenever we find ourselves facing a sudden and unjustified physical, psychological and cognitive deterioration in such a clinical condition old and oldest-old persons.
Keywords
hypercalcemia, hyperparathyroidism, disability, depression, psychosis.
Background
Primary hyperparathyroidism is a disease involving a broad range of alterations, mainly calcium homeostasis, sustained by parathyroid hormone (PTHi) levels that are abnormally elevated. Case studies worldwide show an annual incidence of 20 cases per 100.000 people with an estimated prevalence in the general population of 0.5% to 1%, increasing with age over 2% in both sexes [1]. Several patients with primary hyperparathyroidism are asymptomatic or experience mild symptoms related to chronic hypercalcaemia rather than increased parathyroid hormone [1]. Symptomatic primary hyperparathyroidism is a sporadic disease, mainly occurring after the age of 50 with a ratio between man and women from 1:3 to 1:5. Among symptomatic persons, 20–30% report nephrolithiasis. Overt skeletal disease is rare, while osteoporosis with related fracture is increasing.
Acute hypercalcaemic crisis with nephrogenic diabetes insipidus and dehydration is most likely to appear in patients with a concentration of albumin-adjusted calcium greater than 3.0 mmol/L. Acute pancreatitis is an uncommon, but serious complication. Clinically evident neuromuscular disease is uncommon, but proximal muscle weakness due to type II muscle fibre atrophy can be seen in association with severe bone disease (osteitis fibrosa cystica). Psychiatric symptoms include depression, dementia, confusion, and stupor. Associations have been described with hypertension, diabetes, gastrointestinal ulceration, gout, increased weight, and hyperlipidaemia [2]. In the oldest-old, the clinical picture of hyperparathyroidism differs markedly from that observed in young-old and middle-old persons. Kidney and skeletal disease, particularly osteoarthritis and osteoporosis, are the two common conditions associated with hyperparathyroidism, likely to cause the most severe burden of comorbidity. About 50% of oldest-old persons with hyperparathyroidism experience mental disturbances from slight or severe neurasthenic personality changes, depression, psychiatric symptoms or acute psychosis in most severe cases, or just lack of initiative in most cases [3].
Case Presentation
A woman 85 years old presented with anemia, progressive asthenia and worsening anorexia, insomnia and mental confusion, tightened constipation, polyuria, and incontinence, severe difficulty in walking and, more recent onset, tremors on the upper limbs. Symptoms rapidly become desperate so that the patient, independent up to five months earlier, had become completely dependent on families even for the simplest tasks of everyday life. Ultimately, she become so confused that she did not recognize her sons. The patient's past medical history was significant for non-insulin dependent diabetes mellitus (NIDDM), hypertension, osteopenia, without previous fractures, generalized osteoarthritis and dorsal scoliosis, without walking impairment, renal chronic disease, anxiety and depressive disorder. She had led a sedentary life, but she had no history of smoking or alcohol misuse. She had a family history of cancer. Ongoing chronic medications included angiotensin receptor blocker, vitamin D supplement, proton-pump inhibitor, antidepressants, and iron supplements were recently prescribed because of anemia. At the time of hospital admission, the patient appeared disoriented in time and space and clearly dehydrated. Her vital signs were in the normal range, except a weak pulse rate and not evaluable blood pressure. Fine tremors at rest were noticed in her head, upper limbs and hands; she was unable to stand up although no focal neurological sign was apparent. She presented tenderness with abdominal palpation and torpid peristalsis on physical examination. She reported no respiratory symptoms, no fever or pain. The electrocardiogram showed synusal rhythm, left anterior hemiblock. Other vital signs were in the normal range.
The patient’s blood workup at admission confirmed moderate anemia (Hb 9.7 g/dl, reference range 12.0-16.0), high blood urea nitrogen (199 mg/dl, reference range 10-50) and acute kidney failure (creatinine 2.57 mg/dl, reference range 0.5-1.4). Serum calcium was 16 mg/dl (reference range 8.8-10.6), phosphorus 6.8 mg/dl (reference range 2.5-5) and PTHi 2740 pg/ml (reference range 15-88); CRP 1.6 mg/dl (reference range 0.01-0.5) and ERS 27 mm/hr (reference range 1-20) (Table 1). Urinary calcium and phosphorus were not available.
During the first days of hospitalization, as no other therapy to reduce plasmatic calcium can be performed for the severe renal failure, she was managed with fluid hydration intravenously and diuretic therapy (loop diuretic), with a gradual improvement of the renal function. Given the progressive increase of serum calcium up to 18.9 mg/dl, despite hydration and loop diuretic were continued, she underwent nephrology and endocrinology consultations, started pamidronate infusion, steroids, and ultimately, treatment with cinacalcet, a calcimimetic agent. Thus, she had a gradual and significant reduction in the levels of calcium that reached 14 mg/dl with improvement of her clinical conditions. An ultrasound of the neck showed an intrathyroid parathyroid adenoma in the upper pole of the left thyroid lobe. The 99Tc-sestamibi scanning for parathyroid evaluation confirmed the suspicion of primary hyperparathyroidism (Figure 1) and the CT scan of neck and chest with contrast revealed features suggestive of parathyroid adenoma adjoining the upper pole of the left lobe of thyroid gland. During the CT scan, a fracture of fifth rib in the left appeared. The clinical case was discussed with the consultants of the thoracic surgery unit, the patient underwent surgery ten days apart and a parathyroidectomy and left hemithyroidectomy were performed. Pre-operative PTHi was 1827 pg/ml and post-operative was 60 pg/ml. After surgery, circulating levels of calcium returned to normal range and renal function gradually improved. The istological analysis confirmed an atypical adenoma, with a favorable biological behavior, also considering the complete excision of the neoplasm.
Figure 1: The suspected enlarged gland identified preoperatively by 99Tc-sestamibi scintigraphy.
After five days from surgery, the patient moved to a nursing unit with a satisfying clinical status after starting oral therapy with a calcium and magnesium supplement, calcitriol, and levothyroxine. Two days later, she returned to the geriatric ward because of acute congestive heart failure associated with hospital acquired pneumonia; diuretic therapy and poor adherence to oral calcium supplementation, because of occurrence of nausea and vomiting, had caused transient hypocalcemia associated with hyponatremia and hypokalemia. After resolution of congestive heart failure associated with pneumonia healing, intravenous correction of electrolyte alterations was required to achieve acceptable levels of serum calcium and other electrolytes, with disappearance of nausea and vomiting. The biochemical values reached at the time of hospital discharge are shown in Table 1. After three months from hospital discharge, she performed a clinical follow-up with comprehensive assessment including neuropsychological evaluation. Biochemical exams showed mild anemia (Hb 10.5 g/dl, reference range 12-16), impairment of renal function (creatinine clearance evaluated with Cockroft-Gault 34 ml/min), serum calcium 9.6 mg/dl (reference range 8.8-10.6), vitamin D 40.2 ng/ml (reference range 30-50) and normal PTHi 26 pg/ml (reference range 15-88). Urinary calcium and phosphorus were lower, respectively 36 mg/24h (reference range 100- 300) and 0.15 g/24h (reference range 0.30-10). At clinical examination, vital signs were normal, with resolution of constipation and urinary incontinence. Cognitive functions improved in orientation, memory, attention, visual-spatial and speech abilities; anorexia and psychosis disappeared, while a deflection of mood persisted. From a physical perspective, she scored 9 at the Summary Physical Performance Battery, walking independently in and out of her house, tremors disappeared. She started iron supplements and continued calcitriol and calcium carbonate.
Table 1: Patient’s blood workup at different time points from hospital admission to discharge
|
|
Admission |
Before surgery |
After surgery |
Discharge |
Reference Range |
|
Haemoglobin, gr/dl |
9.7 |
9.9 |
9.4 |
9.7 |
12.0-16.0 |
|
Urea, mg/dl |
199 |
33 |
37 |
37 |
10.0-50.0 |
|
Creatinine, mg/dl |
2.57 |
1.39 |
1.84 |
1.51 |
0.5-1.4 |
|
Creatinine clearance, ml/min |
19 |
39 |
29 |
36 |
>80 |
|
Magnesium, mg/dl |
1.5 |
1.5 |
1.4 |
1.5 |
1.5-2.6 |
|
Calcium, mg/dl |
16.0 |
10.8 |
7.3 |
8.0 |
8.5-10.7 |
|
Phosphorus, mg/dl |
6.8 |
2.8 |
2.3 |
2.8 |
2.5-5.0 |
|
Sodium, mEq/L |
135 |
140 |
134 |
138 |
135-155 |
|
Potassium, mEq/L |
3.6 |
3.2 |
3.4 |
3.9 |
3.5-5.5 |
|
Clorum, mEq/L |
99 |
110 |
97 |
98 |
95-115 |
|
PTHi, pg/ml |
2740 |
1827 |
60 |
58 |
15.0-88.0 |
PTHi: Parathyroid hormone intact
Discussion
Primary hyperparathyroidism is a common disorder in which PTHi is excessively secreted from one or many parathyroid glands. Hyperparathyroidism usually occurs as the result of sporadic parathyroid adenomas or carcinomas but can also be seen in association with multiple endocrine neoplasia and in rare genetic syndromes and metabolic diseases [4]. Classically characterized as hypercalcemia in the presence of elevated serum PTHi concentration, it is now recognized as a spectrum ranging from inappropriately high or even normal PTHi in the setting of high-normal or even normal calcium. [5]. This is the first case report showing calcium levels higher than 18 mg/dl, suspected as incompatible with life in people with kidney disease. Currently, the majority of patients with hyperparathyroidism are asymptomatic and they do not present with the classic symptoms of kidney stones or severe bone disease. An individual is more often diagnosed through routine biochemical laboratory testing done for other purposes. Although patients often lack the classic symptoms, primary hyperparathyroidism is associated with many nonspecific complaints such as depression, anxiety, memory loss, fatigue, sleep problems, bone or muscle pains, gastroesophageal reflux disease, nephrocalcinosis and hypercalciuria [5-7]. Musculoskeletal manifestations occur from hypercalcemia but also due to the direct effect of PTHi on cortical bone. Parathyroid hormone acts on PTHi-receptors in osteoblasts, which stimulates osteoblasts differentiation to osteoclasts with subsequent cortical bone resorption [8]. Therefore, the persistent high PTHi level can lead to osteopenia, osteoporosis, or even to cyst formation and fibrosis. The most severe form of bone disease in primary hyperparathyroidism is known as osteitis cystic fibrosis, but it is rarely seen in modern clinical practice [9].
This case report supports the evidence that hyperparathyroidism is associated with neuropsychological symptoms that can mimic symptoms of other diseases, like depression, personality change, osteoporosis, fatigue or anorexia, or can rise confusion during the diagnosis process. A history of anemia in an older adult’s subject may be an indication of the presence of a disease other than a simple anemia for reduced production in bone marrow. In fact, parathyroid hormone, when an excessive amount, can interfere with normal erythropoiesis by downregulating the erythropoietin receptors on the erythroid progenitors thus diminishing the action of erythropoietin. It was postulated that PTHi affect erythropoiesis through the stimulation of calcium entry into erythroid cells [10]. Since our patient was also affected by an exacerbation of chronic renal failure, it was also important to rule out secondary hyperparathyroidism, a condition in which parathyroid hormone excess is caused by a partial resistance to the metabolic effects of the hormone. Secondary hyperparathyroidism is a frequent complication of vitamin D deficiency, chronic renal failure and a major factor in the pathogenesis of renal osteodystrophy. A high serum phosphate decreased levels of serum 1.25 (OH)2D3 and the sequent low serum calcium are the major metabolic abnormalities in chronic renal failure, which lead to secondary hyperparathyroidism [11].
Table 2: Indications for parathyroidectomy in the setting of primary hyperparathyroidism [12]
|
Age <50 |
|
All Symptomatic Patients |
|
Signs/Symptoms Concerning for Malignancy |
|
Asymptomatic patients with the following: |
|
- Serum Ca >1.0 mg/dl above Normal Range |
|
- Dual-Energy X-Ray Absorptiometry T-Score ≤2.5 At Lumbar Spine, Femoral Neck or Distal Radius |
|
- Vertebral Fractures |
|
- Estimated Glomerular Filtration Rate <60 ml/min/1.73 m2 |
|
- Urinary Ca Excretion >400 mg/24 h |
|
- Nephrolithiasis And Nephrocalcinosis |
|
Asymptomatic Patients Unable to Undergo Medical Surveillance |
|
Asymptomatic Patients Desiring Definitive Surgical Management |
At the time of clinical presentation, our patient had high serum phosphate that returned to normal range after hydration and improvement of renal function. Thus, later hypercalcemia was associated with a low phosphoremia. This allowed us to differentiate a primitive form from both a secondary and tertiary hyperparathyroidism, in both of which phosphoremia is high. It might be possible to conclude that renal failure was not the cause of parathyroid hormone excess but hypercalcemia itself triggering the acute exacerbation of chronic renal failure. The differential diagnosis with neoplastic hypercalcemia is easier because, in the latter, in the face of high levels of serum calcium, parathyroid hormone is constantly suppressed. In our patient, there were all indications for parathyroidectomy (Table 2), which was in fact recommended by the thoracic surgery consultants [12, 13]. Since the sensitivity and predictive value of parathyroid 99Tc-sestamibi scintigraphy is poor in presence of multiglandular disease, an intraoperative parathyroid hormone dosing method was performed to verify complete adenomatous parathyroid removal [14]. Because the half-life of PTHi is short (<2 minutes) a 50-90% drop from baseline within 10 minutes is a signal of complete removal of the hyperfunction of parathyroid tissue [13, 14].
After surgery serum calcium is rapidly reduced, reaching a nadir after 24-36 hours. Parathyroid hormone returns to normal range within 30 hours although the compensatory response to hypocalcemia remains inadequate for a few weeks. After surgery, in patients with bulky adenomas, there is an important calcium requirement that is used to remineralize the skeleton. To avoid electrolyte imbalance, our patient receives calcium, magnesium and vitamin D supplements together with levothyroxine given the hemithyroidectomy performed [15].
Conclusions
Although hyperparathyroidism is a low prevalence disease among older adults, it must be kept in mind whenever we find ourselves facing an unjustified and accelerated physical and mental deterioration. The simple determination of serum calcium levels can lead to a precise diagnosis that is timeless and critical in preventing the clinical derangements from health condition, even affecting the results of surgery.
Article Info
Article Type
Case ReportPublication history
Received: Wed 27, Feb 2019Accepted: Tue 19, Mar 2019
Published: Sat 11, May 2019
Copyright
© 2023 Carmelinda Ruggiero. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.02.008
Author Info
Carmelinda Ruggiero Bianco AR Boccardi V Marta Baroni Mecocci P Messina S Monacelli M Parretti L Puma F
Corresponding Author
Carmelinda RuggieroGeriatric and Gerontology Section, Department of Medicine, University of Perugia, Perugia, Italy
Figures & Tables
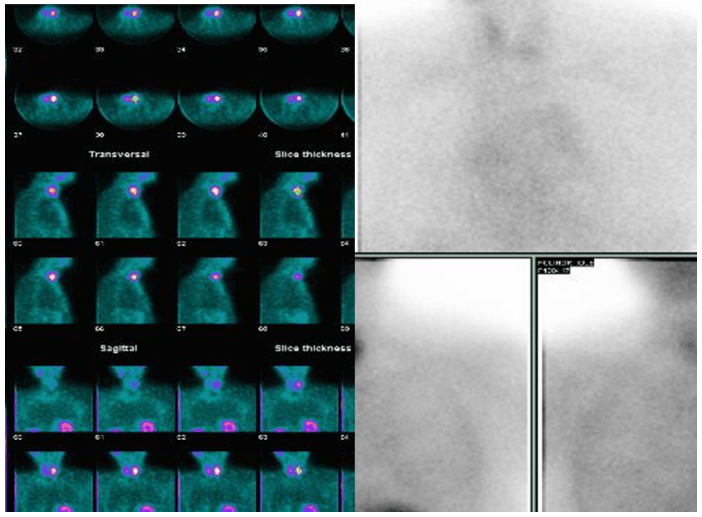
Table 1: Patient’s blood workup at different time points from hospital admission to discharge
|
|
Admission |
Before surgery |
After surgery |
Discharge |
Reference Range |
|
Haemoglobin, gr/dl |
9.7 |
9.9 |
9.4 |
9.7 |
12.0-16.0 |
|
Urea, mg/dl |
199 |
33 |
37 |
37 |
10.0-50.0 |
|
Creatinine, mg/dl |
2.57 |
1.39 |
1.84 |
1.51 |
0.5-1.4 |
|
Creatinine clearance, ml/min |
19 |
39 |
29 |
36 |
>80 |
|
Magnesium, mg/dl |
1.5 |
1.5 |
1.4 |
1.5 |
1.5-2.6 |
|
Calcium, mg/dl |
16.0 |
10.8 |
7.3 |
8.0 |
8.5-10.7 |
|
Phosphorus, mg/dl |
6.8 |
2.8 |
2.3 |
2.8 |
2.5-5.0 |
|
Sodium, mEq/L |
135 |
140 |
134 |
138 |
135-155 |
|
Potassium, mEq/L |
3.6 |
3.2 |
3.4 |
3.9 |
3.5-5.5 |
|
Clorum, mEq/L |
99 |
110 |
97 |
98 |
95-115 |
|
PTHi, pg/ml |
2740 |
1827 |
60 |
58 |
15.0-88.0 |
PTHi: Parathyroid hormone intact
Table 2: Indications for parathyroidectomy in the setting of primary hyperparathyroidism [12]
|
Age <50 |
|
All Symptomatic Patients |
|
Signs/Symptoms Concerning for Malignancy |
|
Asymptomatic patients with the following: |
|
- Serum Ca >1.0 mg/dl above Normal Range |
|
- Dual-Energy X-Ray Absorptiometry T-Score ≤2.5 At Lumbar Spine, Femoral Neck or Distal Radius |
|
- Vertebral Fractures |
|
- Estimated Glomerular Filtration Rate <60 ml/min/1.73 m2 |
|
- Urinary Ca Excretion >400 mg/24 h |
|
- Nephrolithiasis And Nephrocalcinosis |
|
Asymptomatic Patients Unable to Undergo Medical Surveillance |
|
Asymptomatic Patients Desiring Definitive Surgical Management |
References
- Percivale A, Gnerre P, Damonte G, Buscaglia S, Monachesi M, (2015) et al. Primary hyperparathyroidism: epidemiology, clinical features, diagnostic tools and current management. Italian J Medicine 9: 330-345.
- William D Fraser (2009) Hyperparathyroidism. Lancet 374: 145-158.
- Adami S, Marcocci C, Gatti D (2002) Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res 17: N18-N23. [Crossref]
- Tibblin S, Pålsson N, Rydberg J (1983) Hyperparathyroidism in the elderly. Ann Surg 197: 135-138. [Crossref]
- Mackenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A (2011) Primary Hyperparathyroidism: An over- view. Int J Endocrinol 2011: 251410. [Crossref]
- Madkhali T, Alhefdhi A, Chen H, Elfenbein D (2016) Primary hyperparathyroidism. Ulus Cerrahi Derg 32: 58-56.
- Silverberg SJ, Lewiecki EM, Mosekilde L, Peacock M, Rubin MR (2009) Presentation of asymptomatic pri- mary hyperparathyroidism: proceedings of the third international workshop. J Clin Endocrinol Metab 94: 351-356. [Crossref]
- Bandeira F, Griz L, Chaves N, Bandeira F, Griz L, et al. (2013) Diagnosis and management of primary hyperparathyroidism-a scientific statement from the Department of Bone Metabolism, the Brazilian Society for Endocrinology and Metabolism. Arq Bras Endocrinol Metabol 57: 406-424. [Crossref]
- Calvi LM, Sims NA, Hunzelman JL, Knight MC, Giovannetti A, et al. (2001) Activated parathyroid hormone/parathyroid hormone-related protein receptor in osteoblastic cells differentially affects cortical and trabecular bone. J Clin Invest 107: 277-286. [Crossref]
- Sikole A (2000) Pathogenesis of anaemia in hyperparathyroidism. Med Hypotheses 54: 236-238. [Crossref]
- Silver J, Kilav R, Sela-Brown A, Naveh-Many T (2000) Pediatric Nephrology. 14: 626-628.
- Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, et al. (2016) The American Association of Endocrine Surgeon Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg 151: 959-968. [Crossref]
- Parnell KE, Oltmann SC (2018) The surgical management of primary hyperparathyroidism: an updated re- view. International J Endocrine Oncology 5.
- Inabnet WB (2004) Intraoperative parathyroid hormone monitoring. World J Surg 28: 1212-1215. [Crossref]
- Witteveen JE, van Thiel S, Romijn JA, Hamdy NA (2013) Hungry bone syndrome: still a challenge in the post-operative management of primary hyperparathyroidism: a systematic review of the literature. Eur J Endocrinol 168: R45-R53. [Crossref]
