Segment VIII-Dependent Intrathoracic Accessory Liver
A B S T R A C T
Abnormally positioned liver tissues are usually incidental findings diagnosed during imaging studies or surgical procedures. Most of the cases described are of congenital origin. We present a case corresponding to a 21-year-old young man with this entity.
Keywords
Intrathoracic liver, congenital diaphragmatic hernia
Introduction
Abnormally positioned liver tissues are of low prevalence and are usually incidental findings diagnosed during imaging studies or surgical procedures [1]. Typically, they are located in the abdominal cavity, close to the orthotopic liver, and a supradiaphragmatic location is extremely rare [2-6]. Although an acquired aetiology is considered a possibility, especially following trauma or surgery, most of the cases described are of congenital origin, associated with defects in transverse septum development [3, 6].
Case Report
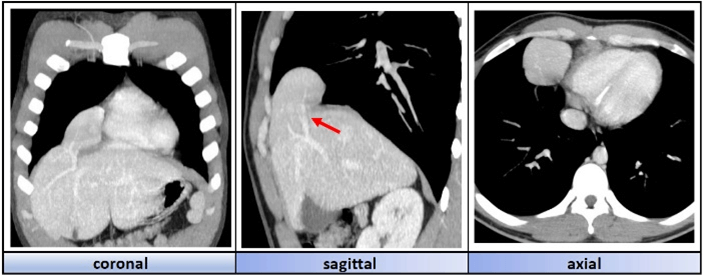
We present the case of a 21-year-old patient with no relevant past history who presents to the emergency room with episodes of mild chest pressure during physical exertion. A diagnostic study is performed, with the significant finding of a space-occupying lesion in the right lower mediastinum on the chest X-ray. To clarify the diagnosis, a thoraco-abdominal CT with contrast is requested, revealing a mass at the level of the lower right mediastinum compatible with accessory liver tissue dependent on segment VIII. It is associated with the presence of a diaphragmatic defect in the right parasternal space (Figure 1).
Figure 1: Tomography images of the different sectional planes in which we appreciate an intrathoracic accessory liver lobe dependant on segment VIII. Its vascular pedicle can be visualised (red arrow).
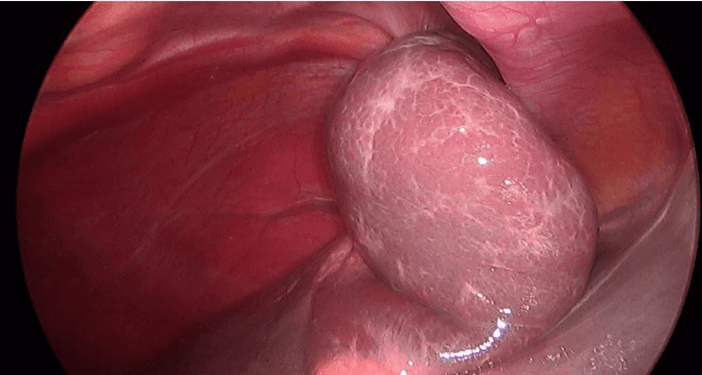
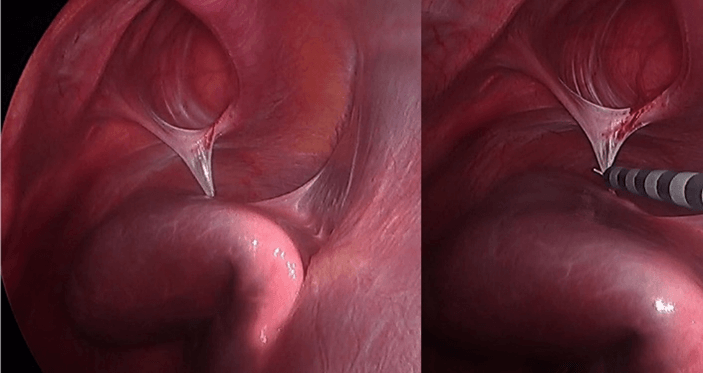
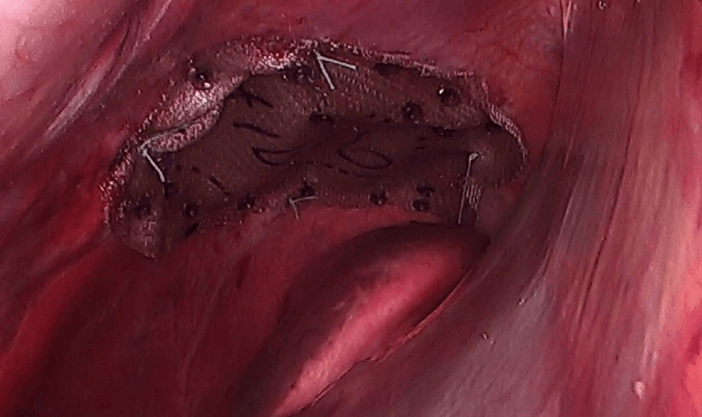
Given the patient’s symptoms and the above-mentioned findings, a surgical procedure was proposed, using a laparoscopic approach. Firstly, the accessory hepatic lobe is reduced into the abdominal cavity (Figure 2). To achieve this, it is necessary to divide loose adhesions joining the heterotopic liver to the diaphragm (Figure 3). Subsequently a diaphragmatic defect measuring 50 x 33 mm could be visualised (Figure 3). A monofilament polypropylene mesh with an absorbable hydrogel barrier was used for the repair. This was attached to the surrounding diaphragm with non-absorbable polyester stitches and helical staples (Figure 4). The postoperative period was uneventful, and he was discharged 24 hours after the procedure. In the check-ups carried out over the following months, the patient felt fully recovered, leading a normal life and the symptoms prior to the intervention had disappeared. A control chest X-ray showed no hernia recurrence.
Figure 2: The heterotopic liver once reduced into the abdominal cavity.
Figure 3: Soft adhesion joining the heterotopic liver to the diaphragm.
Figure 4: Polipropilene mesh attached to diaphragmatic ring.
Discussion
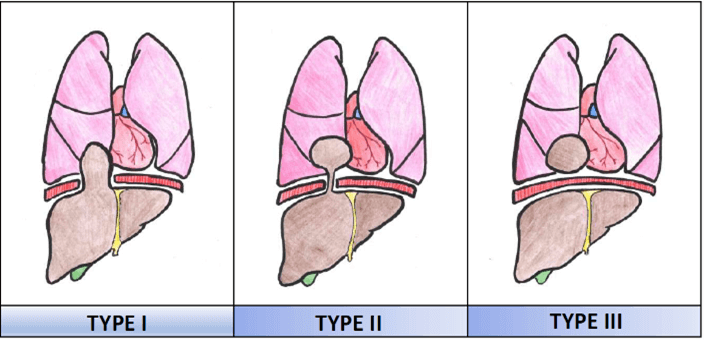
In terms of terminology, an accessory hepatic lobe is considered as one that is attached to the liver by at least one vascular pedicle. By comparison, an ectopic liver is one that is separated from the main liver without any connection to it [7]. With reference to these concepts, Mehmet et al. propose a classification of intra thoracic accessory liver tissue based upon its location and its relationship with the orthotopic liver, as set out below (Figure 5) [2]:
Type I: Direct extension of liver tissue into the thoracic cavity through a diaphragmatic defect. The case presented in this article corresponds to this type.
Type II: Accessory liver within the thoracic cavity connected to the orthotopic liver via a vascular pedicle that perforates the diaphragm or passes through one of its natural anatomical hiatuses.
Type III: Liver tissue in the thoracic cavity independent of the intra-abdominal liver (ectopic liver).
Figure 5: Intrathoracic accesory liver tissue classification. *Figure adapted from Adin ME et al. [2].
Although some cases have been associated with chest pain, dry cough or haemoptysis, it is accepted that the presence of liver tissue in the thoracic cavity rarely has a clinical impact [5, 8]. However, it can be prone to the same pathological events as the abdominal liver and there are even authors who suggest a greater probability of hepatocellular carcinoma, hepatitis or cirrhosis than in the same [2, 6]. Alternatively, the presence of a vascular pedicle can lead to the occurrence of ischaemic lesions due to its torsion, a condition previously described in intraabdominal accessory lobes [2, 9, 10]. Regarding the moment of diagnosis, most cases correspond to intraoperative findings during procedures performed for suspicion of a thoracic tumor of a different origin. [3, 5, 6]. However, thanks to radiological advances, more and more cases are being diagnosed preoperatively [1, 2]. Supradiaphragmatic liver tissue can mimic any space-occupying lesion found at this site, such as tumors, bronchopulmonary sequestration, or hydatid cysts [5, 6, 8]. For this reason, it is vitally important to choose the correct imaging technique, namely CT Angiography or MRI Angiography, to reach the correct diagnosis. With these imaging techniques, a mass will be detected with a radiological density similar to that of liver parenchyma and, if present, a vascular pedicle that connects it to the orthotopic liver will also be visible [2, 5].
Regarding treatment, given the scarcity of cases in the literature, it is difficult to establish a management protocol and hence treatment should be individualized in each case. Most authors recommend surgical resection to prevent complications, such as hepatic ischaemia caused by pedicle torsion or a malignant degeneration [1, 5, 6]. Although most cases reported in the literature were treated via the thoracic route, in our case we opted for a laparoscopic approach. This decision was based on the fact that the defect to be treated affected a liver segment easily accessible via this route. Similarly, surveillance without surgical treatment has been described and shown to result in a good clinical evolution. Although a more powerful imaging technique will be necessary for initial diagnosis, follow-up using ultrasound is a safe option [2].
In conclusion, we consider essential to integrate the presence of accessory liver tissue into the differential diagnosis of supradiaphragmatic lesions, in order to facilitate a correct therapeutic approach. The decision between the options of vigilance or surgery, with or without liver resection, should be individually based according to the criteria of anatomy, clinical symptoms, surgical risk, and the probability of developing complications.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 02, Apr 2021Accepted: Tue 13, Apr 2021
Published: Thu 22, Apr 2021
Copyright
© 2023 Miguel Ángel Suárez-Muñoz. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.04.11
Author Info
Hinojosa-Arco LC Roldan-Rua JF Eslava-Cea Y Ortega-Martinez A Avila-Garcia N Miguel Ángel Suárez-Muñoz
Corresponding Author
Miguel Ángel Suárez-MuñozLiver Transplant Unit, University Hospital Regional, Malaga, Spain
Figures & Tables
References
1.
Ito S, Takeda R,
Kokubo R, Kojima Y, Goto M et al. (2016) Accessory liver lobe attached to the
gallbladder wall preoperatively detected by ultrasonography: A case report. Int
J Surg Case Rep 26: 205-208. [Crossref]
2.
Adin ME,
Cetincakmak MG, Deniz MA, Göya C (2018) Accessory liver within the thoracic
cavity. Surg Radiol Anat 40: 1085-1091. [Crossref]
3.
Kitamura Y,
Sakakura N, Uchida T, Suyama M (2012) Accessory lobe of the right liver mocking
a pulmonary tumor in an adult woman. Gen Thorac Cardiovasc Surg 60:
525-527. [Crossref]
4.
Choi S, Kim H,
Kim J (2008) Heterotopic supradiafragmatic liver combined with intralober
pulmonary sequestration. Ann Thorac Surg 85: 1809-1810. [Crossref]
5.
Wang Y, Junlin L,
Zhang WG, Chen J, He Y et al. (2010) Accessory lobe of right liver mimicking a
pulmonary tumor in an adult male. Ann Thorac Surg 89: e9-e10. [Crossref]
6.
Chen YY, Huang
TW, Chang H, Hsu HH, Lee SC (2014) Intrathorathic caudate lobeo of the liver: a
case report and literature review. World J Gastroenterol 20: 5147-5152.
[Crossref]
7.
Collan Y,
Hakkiluoto A, Hastbacka J (1978) Ectopic liver. Ann Chir Gynaecol 67:
27-29. [Crossref]
8.
Rendina EA, Venuta F, Pescarmona EO, Martelli M, Ricci C
(1989) Intrathoracic lobe of the liver. Case
report and review of the literature. Eur J Cardiothorac Surg 3: 75-78. [Crossref]
9.
Ladurner R, Brandacher G, Mark W, Iannetti C,
Lottersberger C et al. (2005) Complete
hepatic ischemia due to torsion of a large accessory liver lobe: first case to
require transplantation. Transpl Int 18: 467-469. [Crossref]
10. Glenisson M, Salloum C,
Lim C, Lacaze L, Malek A et al. (2014)
Accessory liver lobes: anatomical description and clinical implications. J
Visc Surg 151: 451-455. [Crossref]
