Journals
Remote Monitoring of Patients with COVID-19 after Hospital Discharge with Connected Health Platform: Outcomes and Quality of Life
A B S T R A C T
Background: Telemonitoring with applications and connected devices facilitates a more accessible and efficient attention. Its implementation has been accelerated thanks to the pandemic by COVID-19, where they have allowed the continuity of care.
Objective: To evaluate the efficacy of a remote monitoring platform for the outpatient follow-up after hospital discharge by COVID-19.
Methods: Prospective observational study of patients discharged from the hospital with COVID-19 infection between March 23 and May 25, 2020, who were followed for one month with the Connected Health telemonitoring platform. The mobile phone application connected to a pulse oximeter, allowed to measure vital signs and answer health questionnaires (EQ5D3L and CAT) daily, and alert the medical team that could be contacted by video consultation.
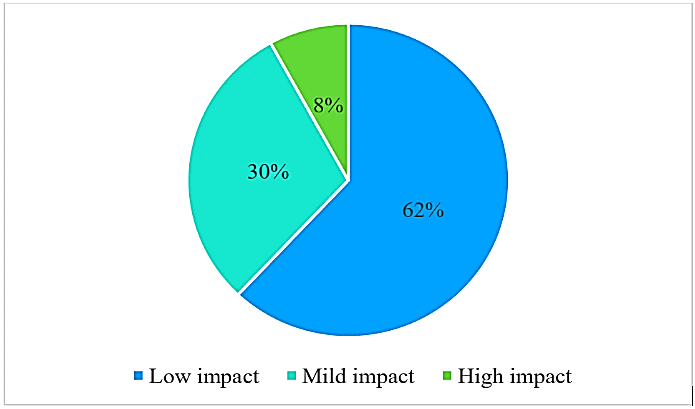
Results: 95 patients (64% male) with a mean age of 54 (SD 26-81) years were included. The application allowed the detection of alerts for pain (80% of patients) and a decrease in oxygen saturation (12%). No patient required hospital readmission or presented complications. The application allowed strict monitoring of symptoms and quality of life. The main symptom was severe pain (59% of patients) followed by anxiety or depression (25%). The average state of health was 65 (SD 20-100). COVID-19 caused a low impact on the quality of life of 62% of the patients, although 8% reported a significant limitation, due to shortness of breath and leaving the house.
Conclusion: telemonitoring allows a safe remote monitoring of patients after hospital discharge by COVID-19. The Connected Health application has allowed the measurement of oxygen saturation, symptoms and quality of life, and the detection and management of alerts by the medical team through video consultation.
Keywords
Digital health, telemedicine, telemonitoring, COVID-19, quality of life, real world data
Introduction
The emergence of digital health is an increasingly evident reality, with innovative patient-centered care models, promoting accessibility, safety and efficiency in all areas of health, thanks to disruptive technologies such as telemedicine, mobile health, applications, artificial intelligence, sensors and other devices. These new digital technologies allow building a different relationship with the patient, focused on their needs, agile and continuous 24 hours a day, where the user enjoys much more information, participation and autonomy. They have the potential to simplify healthcare processes, to improve the quality and reduce the cost of medical care [1].
Mobile devices and applications create the digital channel, where healthcare can be delivered anywhere. The video consultation is a clear example of this, being very useful for disease control and follow-up after discharge from the hospital. The networking of physical devices over the internet allows patients to use connected sensors that measure all kinds of physiological variables, adherence to medication and their perceived state of health, making it easier for doctors to remotely monitor the health of a patient in real time. This has led to the creation of Connected Health platforms, which allow telemonitoring of patients with wearables linked to mobile applications. The data is managed in the cloud by software that allows alerting healthcare personnel of clinical deterioration and thus acting early. There is sufficient evidence that telemedicine reduces healthcare costs, improves the health of the population and the customer experience in healthcare [2].
Real world data is data related to the patient's health status collected in real time, thanks to smartphones and the Internet of Things. The integration of these electronic medical records and biometric data allows creating the digital phenotype of the patient. There is a need for this real data documentation and communication between patients and the medical team. Patients provide information that is complementary but different from that collected by the doctor, since they tend to underestimate the symptoms of the patients, having shown that severe symptoms are not reported in clinical trials by up to 76%. Numerous trials have shown that outpatient symptom monitoring improves communication between the patient and the medical team, quality of life, symptom management and survival, and in turn the satisfaction of the medical team and the support to clinical decision [3, 4].
Digital health solutions have played a crucial role during the COVID-19 pandemic to support public health policies, such as mobile health apps for COVID-19 self-assessment and monitoring [5]. Its benefits have been to establish a formal and secure communication channel between the citizen and the health professional, decrease non-essential visits to health centers, thus reducing the risk of infection for both citizens and health professionals and ensure continuity of care [6]. In the present study, we evaluated the efficacy of outpatient remote monitoring after hospital discharge by COVID-19, by measuring oxygen saturation, symptoms and quality of life, and the detection and management of alerts by the medical team, through video consultation.
Methods
Prospective observational study of patients discharged from the hospital with clinical, serological and/or PCR and radiological diagnoses of lung involvement by COVID-19, between March 23 and May 25, 2020. 164 patients who were consecutively discharged, were offered a clinical follow-up through the Connected Health telemonitoring platform for one month. To do this, they had to be stable, have passed the critical period of the disease, remain fever-free for at least 48 hours, and have a baseline oxygen saturation > 92%. 95 patients agreed to participate, who gave their informed consent and received at their home a pulse oximeter (Lifevit OL-750) with bluetooth connectivity that allowed the connection to the Connected Health application that the patient himself downloaded on his mobile phone. The use of the Connected Health application and data registration was approved by the Center's Research Ethics Committee.
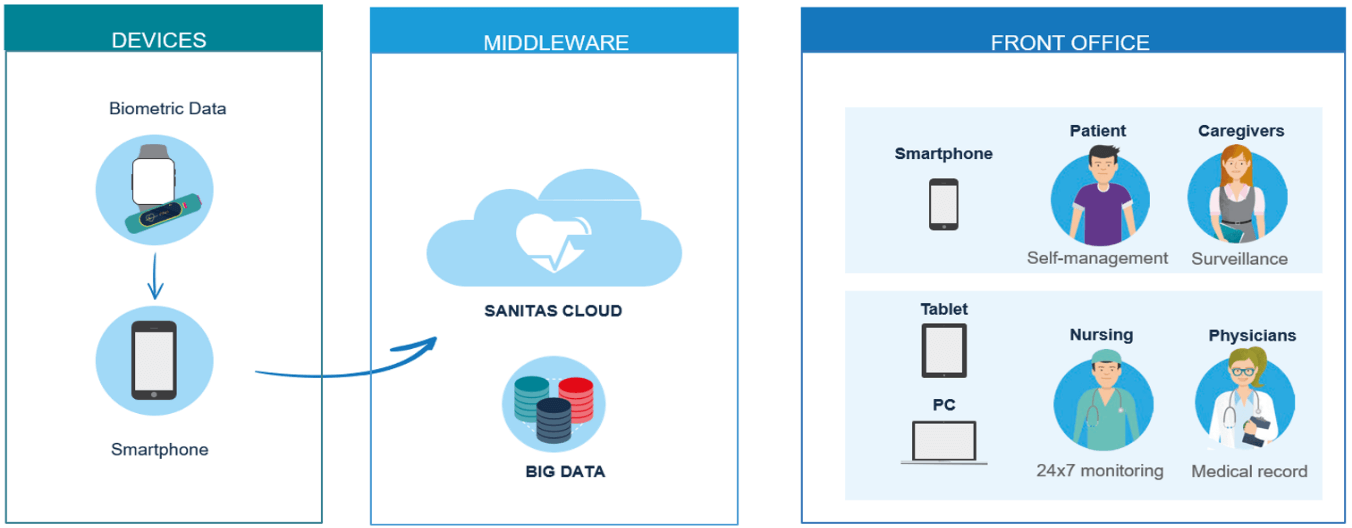
Connected Health is a platform for remote monitoring, continuously, anytime, anywhere, connected to the medical team. It allows to measure and see the evolution of vital signs with devices connected to the application and to answer health questionnaires adapted for different disease profiles. The doctor responsible for the patient activates the service directly from the electronic medical record. The intelligent system analyses these measurements and the answers to the questionnaires and allows the detection of anomalies in the measurements. The nursing team periodically reviews the information received and proactively contacts the patients by video consultation, prioritizing according to the information received, and in the event of incidents if they cannot resolve it, a doctor assesses the situation. The application also allows the patient to contact the nursing team by video consultation 24/7. It includes other functionalities, such as treatment reminders, information of interest about the disease, and keeping family members or caregivers informed (Figure 1), which have proven useful in controlling other diseases such as high blood pressure [7].
Figure 1: Features of Connected Health telemonitoring platform.
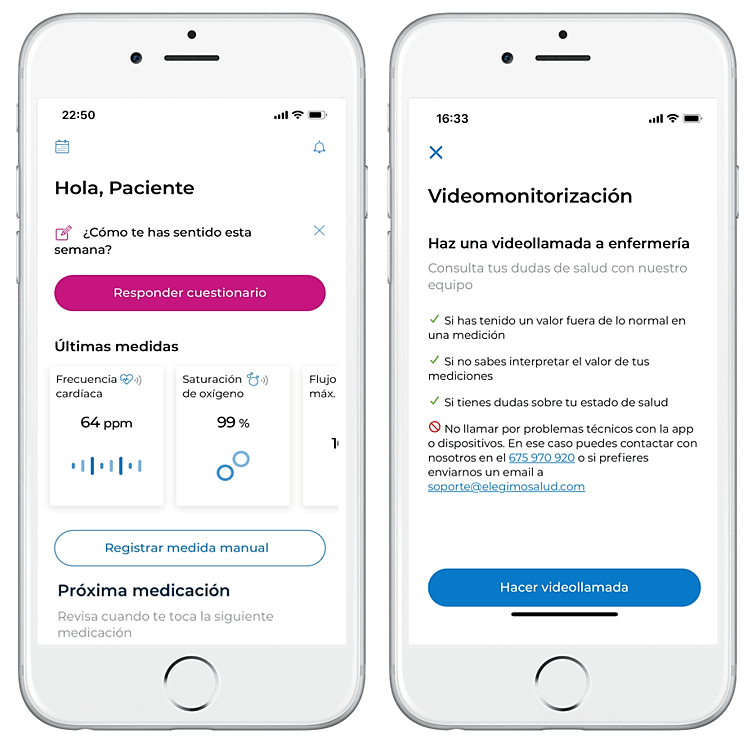
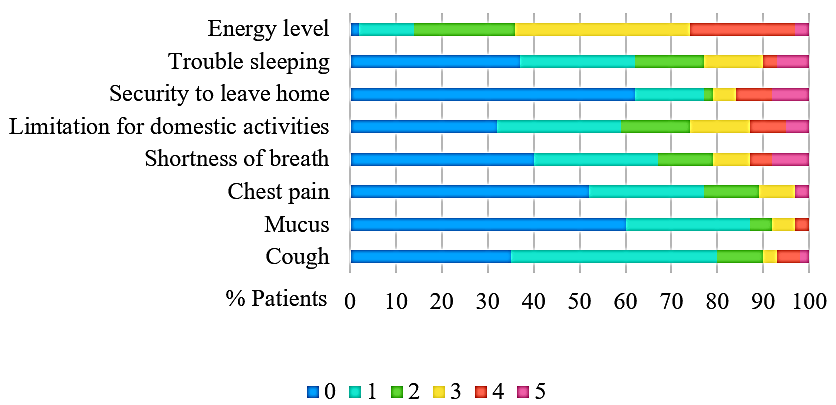
For the follow-up of patients with COVID-19, a post-hospitalization profile was created, collecting the oxygen saturation measurements with a pulse oximeter, and allowing linking other devices or manually including other physiological measurements such as temperature or blood pressure. The application also allowed asking two daily quality of life questionnaires (Figure 2). A generic, self-completed EQ5D3L questionnaire that measures five dimensions of health: mobility, self-care, habitual activities, pain and anxiety or depression, as well as a general health score on a scale of 0 (the worst health condition imaginable) to 100 (the best one), and the specific questionnaire COPD Assessment Test (CAT) whose questions were considered would be useful to see the evolution of respiratory symptoms in patients with COVID-19 [8, 9].
The scores for each section are graduated between 0 (I never cough) and 5 points (I am always coughing). The sum obtains a total score that can range from 0 (better perception of quality of life) to 40 points (worse perception of quality of life). Based on the total score obtained in the CAT, they are classified into 4 groups: low impact (1-10 points): most days are "good days", but the disease is the cause of some of its limitations. Medium impact (11-20 points): there are few "good days" in a week and the disease is one of the main problems of the patient. High impact (21-30 points): There are no "good days" in a typical average week, and illness is the most important problem. Very high impact (31-40 points): the limitation produced by the disease is maximum. For the analysis of the data, usual descriptive statistical techniques have been used.
Figure 2: Connected Health application: screenshots.
Results
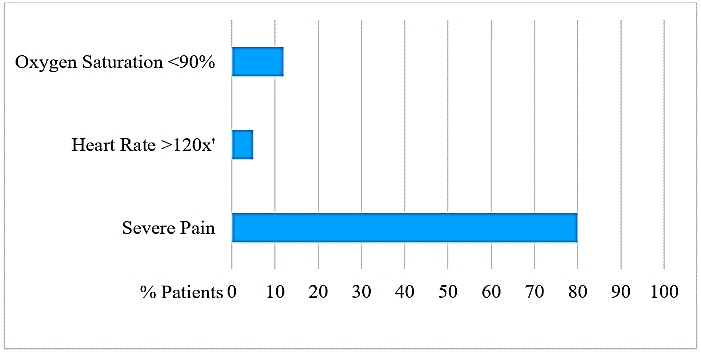
Of the 95 patients included in the study, 61 were men and 34 women, with a mean age of 54 years (SD 26-81) and all completed the follow-up for a month. 69 of the 164 patients who were discharged during the recruitment period refused to enter the program. The application allowed the detection and management of alerts by video consultation, especially for pain, which presented 80% of the patients, and for a decrease in oxygen saturation, which presented 12% (Figure 3).
Figure 3: Alerts detected by the Connected Health application.
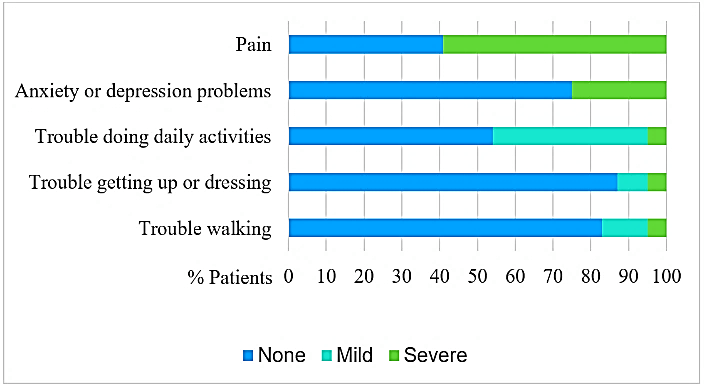
The mean saturation of all participants was 94% (SD 86%-99%). No patient died, presented serious complications, nor did they need to go to the emergency department or hospital readmission. The application allowed strict monitoring of symptoms and quality of life. The main symptom was severe pain (59% of patients) followed by anxiety or depression (25%). Figure 4 shows these results obtained with the EQ5D3L questionnaire, which also showed an average health status of 65 (SD 20-100). The analysis of the CAT questionnaire showed that COVID-19 had caused a low impact for 62% of the patients, where most of the days were "good days", but with some limitation (Figure 5), although 8% of patients reported an important limitation, due to lack of air and when leaving the house (Figure 6). The results shown are the average of the answers of the different days during the follow-up.
Figure 4: Results of the EQ5D3L quality of life questionnaire: symptoms and severity.
Figure 5: Results of the CAT questionnaire (COPD Assessment Test): impact on quality of life.
Figure 6: Results of the CAT (COPD Assessment Test) questionnaire: severity of symptoms in a scale from 0 (little) to 5 (a lot).
Discussion
This study demonstrates the efficacy of the Connected Health platform for the remote monitoring of patients after hospital discharge by COVID-19. The application has facilitated the measurement of oxygen saturation, symptoms and other quality of life measures, and has allowed the detection and management of alerts by the medical team through video consultation. Other studies have shown that remote monitoring of patients to control COVID-19 symptoms at home is effective and safe, improving engagement and health education, while minimizing exposure to COVID-19 and the use of face-to-face medical care [10]. If this telemonitoring is carried out specifically after hospital discharge, it is also safe and efficient; it makes early hospital discharge possible (especially if ambulatory pulse oximetry is offered), it reduces the hospital stay, the use of protective materials and healthcare costs, increasing available beds for other patients. It also increases patient satisfaction, which allows them to recover in their family environment [11].
In our sample, no patient died, needed to go to the emergency room or to be re-admitted to the hospital. These results agree with those published in a similar study, which has also demonstrated the usefulness of telemonitoring in higher-risk COVID-19 patients, by allowing clinical control, early detection of disease deterioration, and offering patient and family support [12]. This monitoring strategy and rapid alert management gives the user a sense of control and security in uncertain days, reducing the use of other healthcare resources. The deployment of digital health solutions, especially telemedicine, has been shown to reduce system overload, save time for the healthcare professional, avoid non-essential visits by citizens to healthcare facilities and decrease the infection rate, both for citizens as probably for health professionals, which in our hospital has only been 7% [13, 14].
The health-related quality of life is the way in which the patient perceives her illness and is of utmost importance to know the state of health of an individual [15]. There are few studies that analyse the quality of life in patients with COVID-19 and it is difficult to compare them due to the use of different health tests. These must be valid, repeatable and sensitive to change. Using generic or disease-specific instruments has its advantages and disadvantages. The generic instruments detect the global effects on quality of life, applicable to different populations with different diseases, but they do not explore particular aspects that are basic in certain diseases, as in the COVID-19 are the degree of dyspnea or cough. Although there is no specific questionnaire for this disease, its symptoms are analysed by other lung disease questionnaires such as CAT, which allow us to assess more subtle changes in the disease, such as shortness of breath, reported by 8% of patients in the present study.
Our quality of life results are similar to those published by Ping et al., where the mean health status score of the EQ-5D questionnaire for patients with COVID-19 was 85.5 and the most frequently reported problem was pain (19%) and anxiety or depression (17.6%) [16]. Their sample presented better health score, possibly due to the fact that they analysed outpatients in general, not just a severe disease after hospital discharge. Other studies show how COVID-19 affects people's health and quality of life, but not only in those who suffer from it, but even in those who suspect having symptoms of COVID-19, which show a higher probability of depression and lower quality of life [17, 18].
This study should be interpreted with caution due to certain limitations. Although the CAT questionnaire has been developed to help assess the impact of COPD symptoms and not to analyse the symptoms of COVID-19, CAT has also been shown to be effective in other diseases such as bronchiectasis, where it correlates with the severity of dyspnea and functional capacity in daily life [19]. In our study, pain was the most frequently reported symptom when responding to the CAT questionnaire, and at the same time, pain was the main reason for alert generation throughout the application.
The alarm situation due to the COVID-19 pandemic and confinement have undoubtedly influenced the high adherence to the program, and therefore these results cannot be extrapolated to the monitoring of other diseases. The fact that the study was conducted in a single hospital and without a control group is another limitation, so it should be confirmed in larger samples and with control groups, which help define the role of telemedicine in this or future epidemics.
At times like this pandemic, the most adverse scenarios often provide an opportunity to develop and test the ability of these digital health technologies to increase the efficiency of systems. The high pressure on the healthcare system in a situation of extreme crisis has been a surprising engine of change. The lessons learned in the pandemic by COVID-19 have helped define future steps, but many financial barriers to the adoption of digital solutions have yet to be removed [20]. Although evaluating the efficiency of adopting these long-term implemented digital health solutions is of utmost importance, the satisfactory experience in this and other studies will certainly create good expectations about the convenience and accessibility of virtual care, which will be difficult to reverse once the COVID-19 crisis subsides.
Conclusion
The past decade has seen unprecedented progress in digital health, enabling closer contact with patients. Thanks to telemedicine, we have the opportunity to create new data-based approaches to identify and intervene early in clinically significant events, thus improving both the quality and quantity of life [21]. This study has shown how the Connected Health platform allows a safe remote monitoring of COVID-19 patients after hospital discharge, facilitating the measurement of oxygen, symptoms and quality of life, and its management by the medical team through video consultation. Although new studies are needed to demonstrate the effectiveness of these digital health tools in situations such as this COVID-19 pandemic, this has undoubtedly helped us, both health personnel and the population, to be better prepared for this next digital age.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 24, Aug 2020Accepted: Tue 08, Sep 2020
Published: Mon 21, Sep 2020
Copyright
© 2023 César Morcillo Serra. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.05.05
Author Info
César Morcillo Serra Domingo Marzal Martín Jorge Velázquez Moro José Francisco Tomás Martínez
Corresponding Author
César Morcillo SerraMedical Direction, Sanitas Digital Hospital, Barcelona, Spain
Figures & Tables
References
- Morcillo C, González JL (2020) New digital healthcare technologies. Med Clin Barc 154: 20-22. DOI: 10.1016/j.medcli.2019.07.004.
- Reed V Tuckson, Margo Edmunds, Michael L Hodgkins (2017) Telehealth. N Engl J Med 377: 1585-1592. [Crossref]
- Kathi Mooney, Donna L Berry, Meagan Whisenant, Daniel Sjoberg (2017) Improving cancer care through the patient experience: how to use patient‐reported outcomes in clinical practice. Am Soc Clin Oncol Educ Book 37: 695-704. [Crossref]
- Lisa S Rotenstein, Robert S Huckman, Neil W Wagle (2017) Making patients and doctors happier-the potential of patient‐reported outcomes. N Engl J Med 377: 1309-1312. [Crossref]
- Anna U Morgan, Mohan Balachandran, David Do, Doreen Lam, Andrew Parambath et al. (2020) Remote Monitoring of Patients with Covid-19: Design, implementation, and outcomes of the first 3,000 patients in COVID Watch. NEJM Catal Innov Care Deliv. [Crossref]
- J Ena (2020) Telemedicine for COVID-19. Rev Clin Esp. [Crossref]
- González JL, Morcillo C (2020) Efficiency of Connected Health Telemonitoring Platform for Patients with High Blood Pressure. J Int Cardiol Open Access 3: 2-4. DOI: 10.31487/j.JICOA.2020.03.09.
- A Simon Pickard, Thomas Kohlmann, Mathieu F Janssen, Gouke Bonsel, Sarah Rosenbloom et al. (2007) Evaluating equivalency between response systems: application of the Rasch model to a 3-level and 5-level EQ-5D. Med Care 45: 812-819. [Crossref]
- P W Jones, G Harding, P Berry, I Wiklund, W H Chen et al. (2009) Development and first validation of the COPD assessment test. Eur Respir J 34: 648-654. [Crossref]
- Tucker Annis, Susan Pleasants, Gretchen Hultman, Elizabeth Lindemann, Joshua A Thompson et al. (2020) Rapid Implementation of a COVID-19 Remote Patient Monitoring Program. J Am Med Inform Assoc ocaa097. [Crossref]
- L A Grutters, K I Majoor, E S K Mattern, J A Hardeman, C F P van Swol (2020) Home telemonitoring makes early hospital discharge of COVID-19 patients possible. J Am Med Inform Assoc ocaa168. [Crossref]
- M Martínez García, M Bal Alvarado, F Santos Guerra, R Ares Rico, R Suárez Gil et al. (2020) Monitoring of COVID-19 patients by telemedicine with telemonitoring. Rev Clin Esp.
- Pol Pérez Sust, Oscar Solans, Joan Carles Fajardo, Manuel Medina Peralta, Pepi Rodenas et al. (2020) Turning the Crisis Into an Opportunity: Digital Health Strategies Deployed During the COVID-19 Outbreak. JMIR Public Health Surveill 6: e19106. [Crossref]
- Yunpeng Ji, Zhongren Ma, Maikel P Peppelenbosch, Qiuwei Pan (2020) Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health 8: e480. [Crossref]
- Cèsar Morcillo, Ofelia Aguado, Jordi Delás, Francesc Rosell (2007) Utility of the Minnesota Living with Heart Failure Questionnaire for Assessing Quality of Life in Heart Failure Patients. Rev Esp Cardiol 60: 1093-1096. [Crossref]
- Weiwei Ping, Jianzhong Zheng, Xiaohong Niu, Chongzheng Guo, Jinfang Zhang et al. (2020) Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS One 15: e0234850. [Crossref]
- Yingfei Zhang, Zheng Feei Ma (2020) Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int J Environ Res Public Health 17: 2381. [Crossref]
- Hoang C Nguyen, Minh H Nguyen, Binh N Do, Cuong Q Tran, Thao T P Nguyen et al. (2020) People with Suspected COVID-19 Symptoms Were More Likely Depressed and Had Lower Health-Related Quality of Life: The Potential Benefit of Health Literacy. J Clin Med 9: 965. [Crossref]
- Fernanda C Lanza, Rejane A S Castro, Anderson A de Camargo, Drielly J M Zanatta, Samia Rached et al. (2018) COPD Assessment Test (CAT) is a Valid and Simple Tool to Measure the Impact of Bronchiectasis on Affected Patients. COPD 15: 512-519. [Crossref]
- Judd E Hollander, Brendan G Carr (2020) Virtually Perfect? Telemedicine for Covid-19. N Engl J Med 382: 1679-1681. [Crossref]
- C Jason Wang, Chun Y Ng, Robert H Brook (2020) Response to COVID-19 in Taiwan: Big Data Analytics, New Technology, and Proactive Testing. JAMA 323: 1341-1342. [Crossref]
