Journals
Pyrophosphate Treatment in Pseudoxanthoma Elasticum (PXE)-Preventing ReOcclusion After Surgery for Critical Limb Ischaemia
A B S T R A C T
Pseudoxanthoma elasticum (PXE) is a rare metabolic disease characterized by reduced plasma pyrophosphate (PPi) concentration, causing progressive soft tissue calcification represented by skin lesions, central vision lost and peripheral artery disease. PXE is currently incurable. Previous reports have shown early high failure after revascularization by unknown mechanism. Reports of oral PPi administration have shown to decrease tissue calcification in a murine model of PXE. We report the outcome of one patient treated with oral PPi and further operated for critical limb ischemia. During the one-year follow-up the operated area has not re-occluded and there have been no significant side effects.
Keywords
Pseudoxanthoma elasticum,PXE,pyrophosphate,critical limb ischemia
Case Report
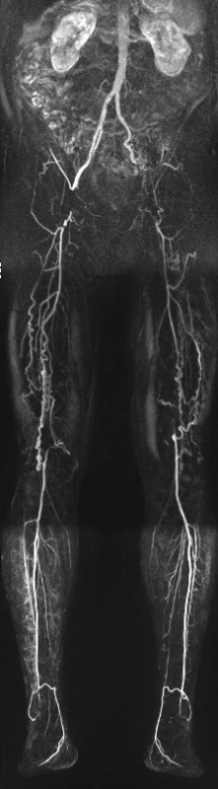
A 59-year-old male having medication for hypertension, type 2 diabetes and hypercholesterolemia, was referred to vascular surgeon due to rest pain in the right lower limb. He has a 40-year history of smoking. Previous suspicion of Pseudoxanthoma elasticum (PXE) on basis of central vision loss and typical skin lesion in the neck was confirmed by skin biopsy and later by homozygous mutation of ABCC6 gene (c.3421C>T, p. Arg1141). Patient has suffered from intermittent claudication, which has then progressed to rest pain in the right limb over the last two months. The ankle-brachial pressure index (ABI) at rest was 0.26 on the right and 0.48 on left side. The Walking Impairment Questionnaire (WIQ) score was 0.19. Magnetic resonance angiography (MRA) showed bilateral occlusion of the common and the superficial femoral artery, as well as occlusion of the left external iliac artery (Figure 1).
Patient had critical ischaemia in his right limb requiring revascularization and he was treated with the right common femoral artery endarterectomy and profundoplasty using the anterior accessory saphenous vein as a patch. The patient quit smoking before the procedure. As PXE patients have an increased risk of spontaneous gastrointestinal bleeding, aspirin medication was not used preoperatively. To prevent re-occlusion, an experimental pyrophosphate treatment was initiated two weeks before the operations with a fasting per oral once daily dose of 3600 mg (44 mg/kg) disodiumpyrophosphate powder (Na2PPi) dissolved into 2 dl of water. With the present Na2PPi-therapy the patients absorbs extra 0.8mg sodium and is informed to decrease daily salt intake. Before instituting treatment, absorption of pyrophosphate with two different doses was tested at ward by a two-day protocol. Fasting plasma pyrophosphate concentration was below normal, 0.7 µmol/l (healthy controls 0.8–1.6 µmol/l). A single dose of pyrophosphate increased the concentration of plasma pyrophosphate to the normal fasting range of healthy controls for 180 minutes (Figure 2).
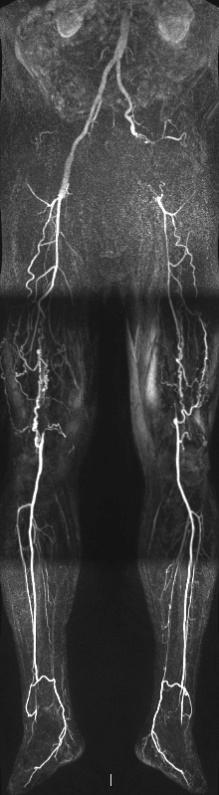
The surgical procedure and recovery were uncomplicated. At one-month control visit, the operated right limb was asymptomatic. The patient experienced only mild claudication of the other limb. The ABI was 0.70 on the right side and 0.52 on the left side. Low-dose aspirin treatment (50 mg per day) was started as the patient had no history of gastrointestinal bleeding. Three months after the operation, the right limb was still asymptomatic, with an ABI of 0.82. MRA showed no re-stenosis in the operated area (Figure 3). The collateral network had increased on both sides as analysed by an independent radiologist. Safety laboratory tests were normal and the patient experienced no significant side effects. Aspirin and PPi therapy were continued unaltered. At six-month and one-year control exams he was measured elevated systemic blood pressure and medication for it was increased. There were no side effects of the pyrophosphate treatment and the supplementation therapy has been continued. The Na2PPi powder has been encapsulated lately because of the bad taste. Recent systemic blood pressure have stayed in recommended limits. One year postoperatively the improved clinical situation remains without signs of re-stenosis on computed tomography angiography (CTA). The WIQ score has improved to 0.89.
Figure 1: Magnetic resonance angiography (MRA) of the patient with Pseudoxanthoma elasticum, who suffered from critical limb ischaemia on the right side and mild claudication on the left side. MRA showed bilateral occlusion of the common and the superficial femoral artery, as well as an occlusion of the left external iliac artery.
Figure 2: Plasma PPi levels of the patient following oral PPi administration. Dotted horizontal lines indicate the normal range of plasma PPi observed in healthy human volunteers (a minimum of 0.854 µmol/L and maximum of 1.688 µmol/L, approximately). Legend indicates the dose (per kg of body weight) and time of PPi consumption.
Figure 3: Magnetic resonance angiography (MRA) of the patient with Pseudoxanthoma elasticum at three months after endarterectomy and profundoplasty on the right side.
Discussion
PXE is a rare metabolic disease with autosomal recessive inheritance. The incidence has estimated to be 1:25,000–100,000 [1]. PXE is characterized by a reduced plasma pyrophosphate (PPi) concentration, causing progressive, extensive soft tissue calcification that leads to elastic fibre fragmentation in various soft conjunctival tissues [2]. The disease results from biallelic mutations in the ABCC6 gene on chromosome 16 that encodes an ATP-binding cassette transporter, leading to inefficient cellular ATP transport from the cell in the liver and, further, to low levels of circulating inorganic PPi. PXE can be diagnosed from a skin biopsy of an affected lesion, but genetic testing is the key to diagnosis. There is no known cure for PXE. The manifestation in PXE is represented by retinal macular degeneration, large skin folds and cardiovascular complications. The complications have a progressive nature. The skin lesions, yellowish plaques (pseudoxanthomas), as well as the retinal angioid streaks may already begin to form in childhood, but the vascular complications typically occur later in life (> 40 years). Primarily, small- and medium-sized arteries are affected. Arteriosclerosis, which is distinct from the more generally known atherosclerosis of the intimal arterial layer, develops in the medial layer. The vascular impact plays a major role in the complications and overall outcome of these patients [3].
PXE is a very rare disease for a vascular surgeon to come across, and there are only a few case reports of surgical treatment for arterial stenosis, showing a high rate of early failure in both endovascular and open repair [4]. The mechanism of postoperative failure is unknown. Furthermore, antiplatelet agents should be avoided due to the risk of gastrointestinal mucosal and retinal haemorrhages, which are associated with PXE due to the degeneration of the elastic lamina in small arteries. Considering the challenging situation of our patient, we strove to prevent early vascular postoperative occlusion by instituting an experimental therapy for the PPi deficiency, which seems to be the key to all complications of PXE. As PXE patients have hypopyrophosphatemia, the logical treatment option is PPi supplementation. However, it was previously assumed that PPi taken orally is not absorbed and only recently has oral PPi administration been shown to increase plasma PPi concentration in animals and humans [5]. Furthermore, the oral administration of PPi has been shown to decrease tissue calcification in a murine model of PXE [5].
This is the first report to show that low fasting PPi level can be normalized for three hours by oral PPi administration in a PXE patient. Individualized per oral pyrophosphate treatment was started with a dose (44 mg/kg) after an absorption study derived from previous studies on experimental animals and healthy individuals [5]. Daily pyrophosphate dose is significantly below the maximum recommended diphosphate concentration in daily food intake (5000–12000 mg/kg; Commission Regulation [EU] N:o 1130/2011). So far, during the one-year follow-up, the operated limb has been asymptomatic, and the operated area has not re-occluded. Furthermore, the ABI and WIQ have improved from the baseline level, and the collateral network has increased in MRA. We cannot rule out the possibility that the encouraging results are based only on the combination of treating PAD risk factors and a successful operation. In the light of the poor results of surgical treatment reported previously, however, the new pyrophosphate supplementation therapy shows promise, as the side effects seem negligible. However, the sodium load in a disease with cardiovascular complications must be considered. Clinical trials on oral pyrophosphate are being planned
Conclusion
A rare disease such PXE should always be considered when the calcification of peripheral arteries is observed at a young age. The standards of follow-up for screening and monitoring the complications of PXE do not currently exist. Genetic counselling should be considered for all PXE patients, and multidisciplinary co-operation is crucial. After careful consideration, surgical treatment can be considered and produce a good result. Nevertheless, it is becoming apparent that systemic pyrophosphate levels play a key role in preventing unwanted soft tissue calcification. It remains unclear whether pyrophosphate is a suitable long-term treatment option for PXE patients. Considering the risk–benefit ratio in the presence of a known relentless vascular complication, however, PPi supplementation therapy deserves a clinical trial, as it holds promise of being effective.
Patient Consent
An informed consent was obtained from the patient.
Funding
This study is financially supported by the Competitive State Research Financing of the Expert Responsibility area of Tampere University Hospital and Vappu Uuspää foundation.
Conflicts of Interest
A.V. filed a patent “Oral pyrophosphate for use in reducing tissue calcification” to the Netherland Patent Office (P32885NL00/RKI).
Article Info
Article Type
Case ReportPublication history
Received: Wed 12, Jun 2019Accepted: Sat 29, Jun 2019
Published: Tue 16, Jul 2019
Copyright
© 2023 Suvi Väärämäki. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.04.02
Author Info
Suvi Väärämäki Hannu Uusitalo Natália Tőkési Saku Pelttari András Váradi Pasi I Nevalainen
Corresponding Author
Suvi VäärämäkiCentre for Vascular Surgery and Interventional Radiology, Tampere University Hospital and University of Tampere, Tampere, Finland
Figures & Tables

References
- Li Q, van de Wetering K, Uitto J (2019) Pseudoxanthoma Elasticum as a Paradigm of Heritable Ectopic Mineralization Disorders: Pathomechanisms and Treatment Development. Am J Pathol 189: 216-225. [Crossref]
- Jansen RS, Duijst S, Mahakena S, Sommer D, Szeri F et al. (2014) ABCC6-mediated ATP secretion by the liver is the main source of the mineralization inhibitor inorganic pyrophosphate in the systemic circulation-brief report. Arterioscler Thromb Vasc Biol 34: 1985-1989. [Crossref]
- Pingel S, Pausewang KS, Passon SG, Blatzheim Ak, Gliem M et al. (2017) Increased vascular occlusion in patients with pseudoxanthoma elasticum. Vasa 46: 47-52. [Crossref]
- Ammi M, Kranenburg G, Omarjee L, Martin L, Spiering W et al. (2015) Abnormally high failure rate for femoral angioplasty in patients with seudoxanthoma elasticum. J Vasc Surg Cases 1: 276-278.
- Dedinszki D, Szeri F, Kozák E, Pomozi V, Tokesi N et al. (2017) Oral administration of pyrophosphate inhibits connective tissue calcification. EMBO Mol Med 9: 1463-1470. [Crossref]
