Pseudomeningocele From Brachial Plexus Root Avulsion
A B S T R A C T
We report a case of a 42-year-old male involved in a motor vehicle accident. Initial MRI revealed T2 hypo-intensity of the anterior cord at the C6 level of the cervical spine which raised significant discussions within the neurosurgical, radiology and ICU departments at our institution. After careful review of images and patient’s clinical examination we suspected root avulsion of the brachial plexus. Subsequent MRI brachial plexus showed a large axillary pseudomeningocele originating from the C5-T2 nerve roots. Our team concluded the patient suffered a complete brachial plexus injury from right lateral hyperflexion as extrapolated from his injuries. The aim of this report is to highlight the uncommon condition and report of key clinical findings and management strategies.
Keywords
Pseudomeningocele, brachial Plexus, root avulsion
Case
A 42-year-old man was transferred to the emergency room after being involved in a motor vehicle accident. The patient was heavily intoxicated and was struck by a car travelling approximately 60km/hr. GCS was 8 on arrival and required intubation due to concerns of airway compromise and haemodynamic instability. No formal neurological examination was performed prior to intubation. He sustained predominantly right sided injuries including a right parietal scalp laceration, right sided extradural haematoma, right sided rib fractures of 5-8 and L1 and L2 transverse process fractures. He was immediately sent to theatres for an evacuation of this extradural haematoma and remained intubated in intensive care due to slow recovery compounded by agitation. There was extensive discussion within the department regarding the need for an MRI of the spine with one clinician advocating clearance on CT alone. For patient safety it was concluded the patient would require clearance either clinically or with radiological evidence of stability via MRI or dynamic x-ray.
MRI of the cervical spine was done on day 2 of admission (Figure 1). It revealed a T2 hypointense area anterior to the cord at C6 level tracking through the C6 neural foramina as well as a T2 hyperintensity on the cord at the level of C3-6. There was no evidence of ligamentous damage. The importance of these findings was not clear. Decision was made to wean sedation and assess the patient clinically. Clinical examination revealed complete loss of power and sensation of the left upper limb with no reflexes elicited. Function was still present in his right upper limb and bilateral lower limbs.
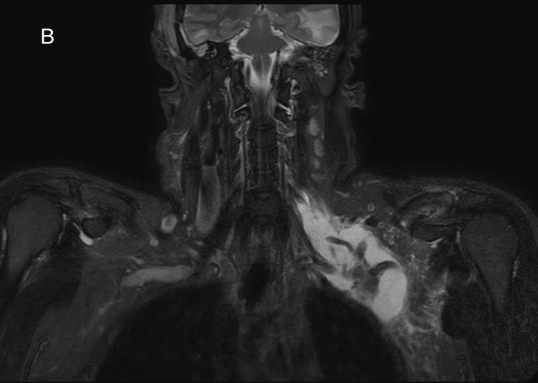
MRI of the brachial plexus was done on day 6 which revealed a large pseudomeningocele in the left axilla with the subclavian artery traversing the collection (Figure 2). Closer inspection of the spine revealed avulsion of the C6, C7 and T2 nerve roots and high T2 and low T1 signal in the neural foramina of C5/6, C6/7, C7/T1 and T1/2. The pseudomeningocele was continuous with these hyperintensities.
Due to extensive other injuries and traumatic brain injury the patient had a prolonged inpatient stay in ICU and the neurosurgical unit. After his acute medical issues were resolved he was transferred to rehabilitation. On 2-month follow-up, although the patient made marked improvement of his cognition and function, he still had no movement or sensation of his left upper limb.
Discussion
The brachial plexus is composed of the anterior branches of the C5, C6, C7, C8, and T1 spinal nerves and responsible for the sensory and motor function of the upper limbs. Due to the biomechanics and range of motion of the cervical spine, the brachial plexus can become injured during high force accidents [1]. The pathophysiology of traumatic brachial plexus injuries is important to understand as the clinical history and presentation can ultimately guide assessment and management. In our patient there was strong evidence to show significant distraction of the arm and contralateral hyperflexion of the neck. This forceful distraction can stretch the nerves and can cause neuropraxia, tears in the dura and arachnoid mater or cause complete root avulsions. Majority of these forces are secondary to motor vehicle accidents with 1% of major traumas associated with brachial plexus injuries [1, 2].
Figure 1: (A) Axial T2 Weighted MRI. Hypointense lesion anterior to cord traversing into the left C5/6 neural foramina (red arrow) (B) Sagittal T2 Weighted MRI of cervical spine revealing hypointensity anterior to cord (red solid arrow) with T2 cord changes at C3-C6 (dotted red arrow).
Figure 2: Coronal MRI of Brachial plexus. A) T1 weighted images showing hypointense collection at left axilla with B) T2 weighted imaging showing T2 hyperintensity for the same collection. Fluid collection continuous with the neural foramina of the brachial plexus.
Clinical examination is of key importance as early assessment and establishing neurological stability or deterioration dictates timing and candidacy for surgery [3]. Patients may present with weakness, dysesthesia and headaches. Weakness or sensory changes in the distribution of the brachial plexus should act as an indication for injury and can indicate the level of the injury. Headaches occurred in 15.2% of patients with traumatic brachial plexus injuries with a third of these patients having positional headaches [4]. These findings may be related to either the meningeal irrigation from blood within the CSF or pseudomeningocele developing from the avulsed nerve roots causing low CSF pressure headaches.
MRI remains the gold standard in assessing brachial plexus injuries and can help differentiate pre-ganglionic and post ganglionic injuries which helps dictate the plans and prognosis of these injuries [5, 6]. Nerves can be identified on MRI as hypo-intense linear structures on T1 and T2 surrounded by fat. In injuries there is a break in the nerve and can also be associated with surrounding blood or pseudomeningocele. Pseudomeningocele on MRI are however not absolute signs of root avulsions with high false positive rates and results should always be paired with clinical examination to improve diagnostic accuracy [7]. Unfortunately MRI is still unable to differentiate accurately the level of the nerve injury i.e post ganglionic vs preganglionic which is helpful for management [5]. Some clinicians advocate for exploration and identification of the brachial plexus injury to guide management. In our patient the combination of cord damage, blood in subdural space, pseudomeningocele, sensory and weakness in the upper limb were all indicators of root avulsion.
Management in patients in high energy traumas should always follow ATLS protocol and patients should remain in C spine precautions. Clearance of the cervical spine is out of the scope of this report however it is clear when there is concerns of ligamentous injury or in comatose patient, further investigations are required. This is usually in the form of dynamic x-rays of the cervical spine or an MRI [8]. Once brachial plexus injuries are identified the aim should be to improve function. Post ganglionic injuries have a favourable prognosis as the anterior horn cells in the spinal cord persists. Therefore if continuity is established with surgery then chance of recovery can be improved[9, 10]. In patients with pre-ganglionic injuries such as root avulsions nerve transfers are required as the cell bodies of the native motor neurones have receded [10].
Conclusion
In the assessment of traumatic brachial plexus injuries there was significant discordance within clinicians regarding the significance of the MRI findings. Using our case as a vignette we hoped to illustrate with our images the clinical clues and indications to suggest brachial plexus root avulsions.
Article Info
Article Type
Case ReportPublication history
Received: Sat 31, Aug 2019Accepted: Thu 19, Sep 2019
Published: Fri 27, Sep 2019
Copyright
© 2023 Joseph Yoon. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.05.01
Author Info
Corresponding Author
Joseph YoonDepartment of Neurosurgery, Royal Darwin Hospital, Northern Territory, Australia
Figures & Tables



References
- Faglioni W Jr, Siqueira MG, Martins RS, Heise CO, Foroni L (2014) The epidemiology of adult traumatic brachial plexus lesions in a large metropolis. Acta Neurochir (Wien) 156: 1025-1028. [Crossref]
- Midha R (1997) Epidemiology of brachial plexus injuries in a multitrauma population. Neurosurgery 40: 1182-1189. [Crossref]
- Silbermann-Hoffman O, Teboul F (2013) Post-traumatic brachial plexus MRI in practice. Diagn Interv Imaging 94: 925-943. [Crossref]
- H́ebert-Blouin MN, Mokri B, Shin AY, Bishop AT, Spinner RJ (2013) Cerebrospinal fluid volume-depletion headaches in patients with traumatic brachial plexus injury: Clinical article. J Neurosurg 118: 149-154. [Crossref]
- Wade RG, Takwoingi Y, Wormald JCR, Ridgway JP, Tanner S et al. (2018) Magnetic resonance imaging for detecting root avulsions in traumatic adult brachial plexus injuries: Protocol for a systematic review of diagnostic accuracy. Syst Rev BMC 7: 76. [Crossref]
- Fuzari HKB, Dornelas de Andrade A, Vilar CF, Sayão LB, Diniz PRB et al. (2018) Diagnostic accuracy of magnetic resonance imaging in post-traumatic brachial plexus injuries: A systematic review. Clin Neurol Neurosurg 164: 5-10. [Crossref]
- Laohaprasitiporn P, Wongtrakul S, Vathana T, Limthongthang R, Songcharoen P (2018) Is Pseudomeningocele an Absolute Sign of Root Avulsion Brachial Plexus Injury? J Hand Surg Asian Pac Vol 23: 360-363. [Crossref]
- Kumar Y, Hayashi D (2016) Role of magnetic resonance imaging in acute spinal trauma: A pictorial review. BMC Musculoskelet Disord 17: 310. [Crossref]
- Dubuisson AS, Kline DG (2002) Brachial plexus injury: a survey of 100 consecutive cases from a single service. Neurosurgery 51: 673-682. [Crossref]
- Karalija A, Novikova LN, Oradd G, Wiberg M, Novikov LN (2016) Differentiation of Pre- and Postganglionic Nerve Injury Using MRI of the Spinal Cord. PLoS One 11: e0168807. [Crossref]
