Providing Arterial Supply to the Liver Graft with Recipient Splenic Artery in Living Donor Liver Transplantation: Case Report
A B S T R A C T
Hepatic arterial reconstruction is an important step in graft implantation in liver transplant procedure. Hepatic arterial anastomosis always demands meticulous and highly skilled surgical techniques to provide adequate blood supply to the graft. Hepatic arterial intimal dissection in liver transplantation is although a rare but documented complication, with incidence of less than 5%, but having dreadful complications. To overcome this complication of Recipient hepatic artery dissection, various techniques have been described by different authors. Here, in this case report we are describing technique of utilization of transposed recipient splenic artery for graft arterial inflow where native hepatic artery was dissected up to common hepatic artery. Post-operative recovery was uneventful and on follow up, patient was absolutely fine. So, recipient splenic artery is a safe alternative option in such complex situations for providing arterial blood flow to the graft and moreover it avoids the burden of extra anastomosis which is required in conduit technique.
Keywords
Living donor liver transplantation, splenic artery, hepatic artery dissection, graft, arterial supply
Introduction
Liver transplantation is the recommended treatment for patients with end‐stage liver disease, hepatic metabolic disorders and hepatocellular carcinoma [1]. Hepatic arterial reconstruction between recipient and graft hepatic arteries is an important step in graft implantation in liver transplant procedures. Hepatic arterial anastomosis always demands meticulous and highly skilled surgical techniques to provide adequate blood supply to the graft [2].
Hepatic arterial intimal dissection in liver transplantation is although a rare but documented complication, with incidence of less than 5%, but having dreadful complication of graft loss initially and biliary complications later on. Hepatic arterial reconstruction in living donor liver transplantation is a challenging job for transplant surgeons due to short stump, small diameter of donor hepatic artery, and also due to discrepancy in vessels size of the graft and recipient hepatic arteries. Selecting an appropriate vessel for hepatic arterial reconstruction and applying microsurgical techniques are crucial steps in reducing the risk of hepatic artery thrombosis during living donor liver transplantation [3]. To overcome this complication of Recipient hepatic artery dissection, various techniques have been described by different authors like using of an extra-anatomic jump graft with a conduit [4, 5]. Here, in this case report we are describing a rare technique of utilization of transposed recipient splenic artery for graft arterial inflow in spite of using extra-anatomic jump graft with a conduit, in a recipient with dissected hepatic artery. Post-operative recovery was uneventful and on follow up, patient was absolutely fine.
Case Presentation
A 44-year-old male, with HCV related decompensated chronic liver disease, with MELD-Na score of 22 and child score of C; 10/15. Living donor liver transplantation was planned for this patient. Preoperative assessment and work up of both donor and recipient were done. Donor Right Hepatectomy was done first and graft with normal right hepatic artery was provided for implantation. During graft implantation, reconstruction of the venous outflow and portal vein inflow was done first as usual, followed by the anastomosis of recipient hepatic artery with the right hepatic artery of the graft. Intra-operative Doppler study was unsatisfactory. Recipient hepatic arterial dissection was found on re-opening of anastomosis. So, it was decided to give arterial inflow to the graft with recipient Splenic artery (central branch of the celiac trunk), which is the most nearby located artery with easier access, as well as having wide lumen and good flow.
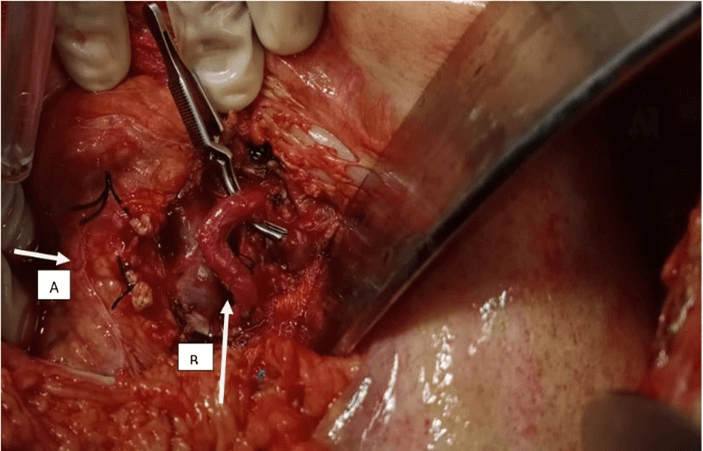
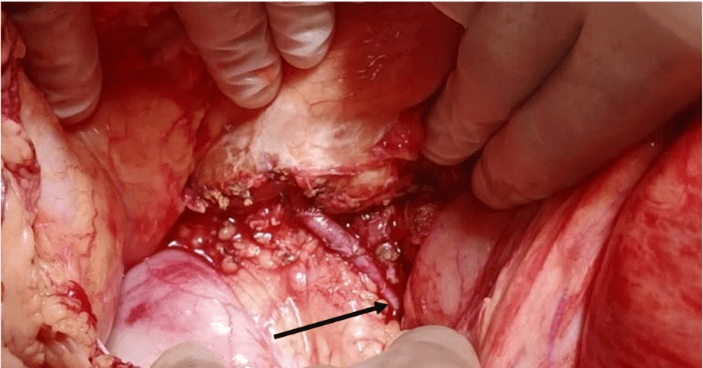
Meticulous dissection around the splenic artery was done. Splenic artery up to splenic hilum was skeletonized and almost 8cm length of splenic artery was achieved. Splenic vein was identified and preserved. Major bleeding or any difficulty during skeletonization of splenic artery was not faced. After getting proper length, bulldog clamp was applied at splenic artery origin site from celiac trunk, and ligation done with silk sutures on the distal end near the splenic hilum. Transposition of splenic artery behind the stomach to graft hilum was done, and a tension free end to end anastomosis with Proline 7/0 was performed between the splenic artery and right hepatic artery of the graft. Intra-operative doppler ultrasound was having normal velocity and resistance index with good arterial inflow to the graft as required for the implanted graft. Post-operative recovery was uneventful and daily Doppler ultrasound for five days showed normal parameters of vascular inflow and outflow. Patient was discharged on 11th post-operative day with CT angiogram showing good arterial inflow to the liver parenchyma. Patient remained in close follow up. At the end of first month Doppler ultrasound was done which was again normal.
Figure 1: After skeletonization. Arrow A (pancreas), Arrow B (splenic artery).
Figure 2: After hepatic arterial reconstruction. Arrow marks towards anastomotic site.
Discussion
Different techniques have been reported in literature to deal with the complication of recipient hepatic artery intimal dissection, like the use of an extra-anatomic jump graft from Aorta with a conduit [4, 5]. The use of saphenous vein graft as a conduit, is a common technique used for giving arterial inflow to the graft [6]. But this technique involves major dissection around abdominal aorta, which put the patient at risk of bleeding and lymph leakage [7]. Few studies have also mentioned alternative to extra-anatomic jump graft in cases of dissected hepatic artery, like interposed left gastric and right gastroepiploic arteries for hepatic arterial inflow. There is advantage of single anastomosis in cases of maintaining inflow with interposed artery in comparison to extra-anatomic jump graft from Aorta [8]. Several other authors have reported various other options of vascular grafts for hepatic arterial flow reconstruction like iliac artery and inferior epigastric artery in liver transplantation [9, 10].
As mentioned above, we used recipient splenic artery for maintaining hepatic arterial inflow, which is the most nearby located artery with easier access, as well as having wide lumen and good flow. Therefore, splenic artery transposition, without the need of conduit seems to be a more appropriate method for hepatic arterial reconstruction and graft inflow, with less chance of developing post-operative hepatic arterial thrombosis. So, recipient splenic artery is a safe alternative option in such complex situations for providing arterial blood flow to the graft and moreover it avoids the burden of extra anastomosis which is required in conduits technique.
Author Contributions
Shams Uddin: Study Conception and Design; Hala Izzu: Acquisition of Data; Kaleem Ullah: Critical Revision and Overall Supervision; Abdul Wahab Dogar: Drafting of Manuscript; Syed Hasnain: Review of Discussion; Abdul Ghaffar: Analysis and Interpretation of Data.
Conflicts of Interest
None.
Grant Support and Financial Disclosure
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 27, Nov 2020Accepted: Tue 08, Dec 2020
Published: Thu 24, Dec 2020
Copyright
© 2023 Kaleem Ullah. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.TCR.2020.02.06
Author Info
Shams Uddin Hala Izzu Kaleem Ullah Abdul Wahab Dogar Syed Hasnain Abdul Ghaffar
Corresponding Author
Kaleem UllahConsultant, Organ Transplant Unit, Pir Abdul Qadir Shah Jillani Institute of Medical Sciences, Gambat, Sindh, Pakistan
Figures & Tables
References
- Tamura S, Sugawara Y, Kishi Y, Akamatsu N, Kaneko J et al. (2005) Living‐related liver transplantation for Wilson's disease. Clin Transplant 19: 483-486. [Crossref]
- Cherqui D, Riff Y, Rotman N, Julien M, Fagniez PL (1994) The recipient splenic artery for arterialization in orthotopic liver transplantation. Am J Surg 167: 327-330. [Crossref]
- Yang Y, Zhao JC, Yan LN, Ma YK, Huang B et al. (2014) Risk factors associated with early and late HAT after adult liver transplantation. World J Gastroenterol 20: 10545-10552. [Crossref]
- Vijay K, Naidu CS, Rao P, Sharma S, Godara R et al. (2013) Extra anatomic hepatic artery reconstruction in deceased donor liver transplantation–Feasibility and outcome. Ind J Transplant 7: 6-9.
- Dokmak S, Aussilhou B, Landi F, Dondéro F, Termos S et al. (2015) The recipient celiac trunk as an alternative to the native hepatic artery for arterial reconstruction in adult liver transplantation. Liver Transpl 21: 1133-1141. [Crossref]
- Garcia Valdecasas JC, Grande L, Rimola A, Fuster J, Lacy A et al. (1990) The use of the saphenous vein for arterial reconstruction in orthotopic liver transplant. Transplant Proc 22: 2376-2377. [Crossref]
- Vanderlan WB, Abouljoud MS, Yoshida A, Kim DY (2008) Experience with recipient splenic artery inflow in adult liver transplantation: a case series. Cases J 1: 82. [Crossref]
- Steinbrück K, Fernandes R, Enne M, Vasconcelos R, Bento G et al. (2014) Right gastroepiploic artery as an alternative for arterial reconstruction in living donor liver transplantation. Case Rep Hepatol 2014: 616251. [Crossref]
- Sansalone CV, Colella G, Rondinara GF, Rossetti O, De Carlis L et al. (1994) Iliac artery graft interposition in liver transplantation: our experience in 72 cases. Transplant Proc 26: 3535-3536. [Crossref]
- Nakatsuka T, Takushima A, Harihara Y, Makuuchi M, Kawarasaki H et al. (1999) Versatility of the inferior epigastric artery as an interpositional vascular graft in living-related liver transplantation. Transplantation 67: 1490-1492. [Crossref]
