Journals
Posterior Percutaneous Endoscopic Cervical Diskectomy as a treatment for cervical radiculopathy
A B S T R A C T
Anterior cervical diskectomy and fusion (ACDF) is the gold standard treatment for patients with cervical radiculopathy. However, the use of ACDF for patients with cervical radiculopathy can result in several disadvantages, such as limitation of motion and accelerating degeneration of adjacent segment. An alternative, less invasive endoscopic technique, posterior percutaneous endoscopic cervical diskectomy (P-PECD), was applied to address the above problems associated with ACDF. The patient presented with pain and weakness of the left arm for 2 years. P-PECD was applied and complete decompression of the nerve root was achieved. The symptoms were relieved after surgery. Postoperative MR showed the ruptured disk fragment was successful removed. No spinal instability or symptom relapse was observed in follow-up. P-PECD may be an option for patients with cervical radiculopathy
Keywords
cervical radiculopathy, endoscopic technique, posterior percutaneous endoscopic, cervical diskectomy
Introduction
Anterior cervical diskectomy and fusion (ACDF) is currently the standard surgery for patients with cervical radiculopathy. However, there are problems associated with ACDF, such as limitation of motion and accelerating adjacent segment degeneration [2]. Due to the development of endoscopic system, the minimally invasive spine surgery has become increasingly applied [3]. To solve the above problems, we performed posterior percutaneous endoscopic cervical diskectomy (PECD) for patient with cervical radiculopathy.
Presentation of the case
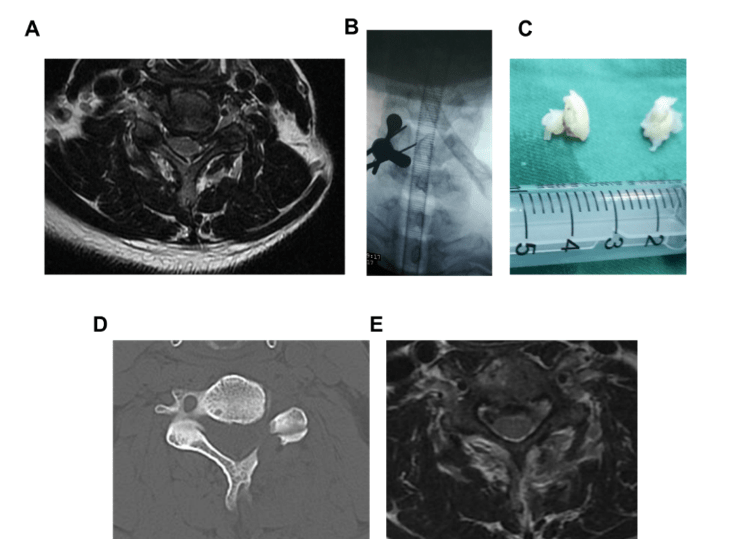
A 51 years old patient, male, presented with pain and weakness of the left arm for 2 years. The pain didn’t ameliorate after conservative treatments. Cervical MRI showed C5/6 cervical disk herniation (Figure 1A). Eaton and Spurling test of left arm is positive. This patient was diagnosed as cervical spondylotic radiculopathy and scheduled for posterior percutaneous endoscopic cervical decompression (PECD). Under general anesthesia, the patient was placed in a prone position. Neuromonitoring was applied during surgery. To widen the interlaminar window, the neck was mild flexed. 0.9% saline was continuous irrigated during surgery. A 6.9mm skin incision was made at the medial junction of the inferior and superior facet joint. Then, the obturator was introduced. The tip of the obturator was placed at the V-point (Figure 1B) and the endoscope was introduced. The soft tissue around the V-point was cleared out. A drilling was used to drill the medial margin of the interlaminar space and to expose the ligamentum flavum. The dura and nerve root were exposed after ligamentum flavum was removed. Ruptured fragments were removed after probing by nerve stripper. Decompression was confirmed by examining the inferior or superior of nerve root. A large disk fragment was removed during the surgery (Figure 1C).
Pain of the left aim he had experienced preoperatively had disappeared soon after surgery. Postoperative CT showed that the medical facet was minimally removed (Figure 1D). Postoperative MR indicated that the ruptured disk fragment was successful removed (Figure 1E).
Discussion
Cervical radiculopathy is one of the most common diseases of the cervical vertebra. Surgery may become necessary if conservative treatment is ineffective. Anterior cervical diskectomy and fusion (ACDF) is the gold standard in the treatment of cervical radiculopathy. However, there are problems associated with ACDF, such as loss of motion due to bony fusion, complications and adjacent segment disease. There are several surgical techniques to address the above problems, such as posterior foraminotomy and discectomy. Posterior approach has several advantages, such as preserving the movement of disk and reducing adjacent segmental disease. However, traditional posterior approach has disadvantages, such as axial pain and paraspinal muscle spasm.
A minimally invasive surgical technique, posterior PECD was used to address the above problems [5]. Continuous fluid and endoscopic lighting system were applied during operation to improve the definition of the visual field. In addition, surgical trauma is markedly reduced using a 6.9 mm incision. In a word, PECD has several advantages, such as less trauma, less bleeding, faster recovery and shorter duration of hospital stay compared with traditional surgery [1]. However, PECD has several disadvantages, such as a limited view, indication limitations and a high learning curve [3]. In addition, complications associated with PECD, such as root injury, wound infection and instability should be avoided [4]. The following tips should be undergone strictly when performing PECD. The nerve electrophysiology monitoring is necessary during the operation to avoid nerve injury. In addition, the surgeon should avoid pulling the nerve beyond its limitations. The surgeon should have a flexible grasp of the full-endoscopic technique of the lumbar spine before performing PECD.
Figure 1: Preoperative magnetic resonance (MR) image showed a herniated disk at C5–6 (A). The obturator was placed at the medial edge of the articular facet joint confirmed by X ray (B). A large disk fragment was removed after the surgery (C). Postoperative CT image showed that the medical facet was minimally removed (D). Postoperative MR image showed complete removal of the ruptured disk fragment (E).
Conclusion
The PECD is an effective treatment for patients with cervical radiculopathy by complete nerve root decompression.
Article Info
Article Type
Case ReportPublication history
Received: Mon 27, May 2019Accepted: Thu 13, Jun 2019
Published: Thu 20, Jun 2019
Copyright
© 2023 Hao Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.03.08
Author Info
Zha Dingsheng Fernando Cardoso Gomes Hao Wu Lek Hang Cheang Shijun Chen Wuyan Xu Yaqi Li Zhen Lin
Corresponding Author
Hao WuDepartment of orthopedics, First Affiliated Hospital of Jinan University, Guangzhou, Guangdong, China
Figures & Tables
References
- Komp M, Oezdemir S, Hahn P, Ruetten S (2018) Full-endoscopic posterior foraminotomy surgery for cervical disc herniations. Oper Orthop Traumatol 30: 13-24. [Crossref]
- Lan Z, Huang Y, Xu W (2019) Relationship Between T1 Slope Minus C2-7 Lordosis and Cervical Alignment Parameters After Adjacent 2-Level Anterior Cervical Diskectomy and Fusion of Lower Cervical Spine. World Neurosurg 122: e1195-e1201. [Crossref]
- Wu PF, Li YW, Wang B, Jiang B, Tu ZM et al. (2019) Posterior Cervical Foraminotomy Via Full-Endoscopic Versus Microendoscopic Approach for Radiculopathy: A Systematic Review and Meta-analysis. Pain Physician 22: 41-52. [Crossref]
- Wu PF, Liu BH, Wang B, Li YW, Dai YL et al. (2018) Complications of Full-Endoscopic Versus Microendoscopic Foraminotomy for Cervical Radiculopathy: A Systematic Review and Meta-Analysis. World Neurosurg 114: 217-227. [Crossref]
- Zheng C, Huang X, Yu J, Ye X (2018) Posterior Percutaneous Endoscopic Cervical Diskectomy: A Single-Center Experience of 252 Cases. World Neurosurg 120: e63-e67. [Crossref]
