Pirogoff Amputation with a Disappointing Outcome: A Case Report
A B S T R A C T
Case Presentation: A 53-year-old motorcyclist suffered trauma with an extensive foot injury. A Pirogoff amputation was performed. A hindfoot amputation might be considered as an alternative option rather than directly proceeding to a trans-tibial amputation.
Results: A Pirogoff amputation was performed with a disappointing course afterward. Subsequently, we performed a literature search on the Pirogoff amputation.
Conclusion: Further research is needed concerning the optimal amputation level for patients who need a hindfoot amputation since good studies are lacking. In general, a major advantage of the Pirogoff amputation is the possibility of some barefoot mobility. The disadvantages are fitting problems due to a bulbous stump and limited installation height for the incorporation of a prosthesis. A trans-tibial amputation might be considered in young and healthy patients because of the extensive possibilities for prosthetic fitting. The final decision of the amputation level should be made by an experienced surgical and rehabilitation team discussing the advantages and disadvantages with the patient involved. Currently, evidence from the literature is too limited to guide this discussion and the decision-making process.
Keywords
Pirogoff amputation, Hindfoot amputation, Rehabilitation
Introduction
In the case of extensive foot lesions where the foot cannot be reconstructed, amputation at different levels can be performed. The selection of the adequate amputation level involves an assessment of the medical possibilities and consideration of possibilities for prosthetic fitting and expected mobility. In case a distal partial foot amputation cannot be performed, a Pirogoff amputation might be considered among other procedures as an alternative option rather than directly proceeding to a major amputation, such as a trans-tibial amputation (TTA).
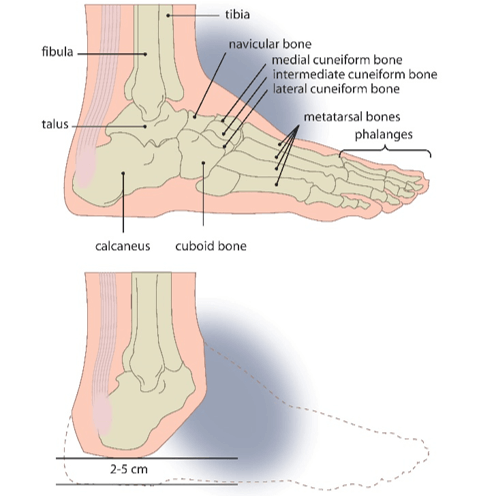
Pirogoff amputation, first described in 1854, results in an end-bearing stump with approximately 2-5cm of leg-length shortening (Figure 1), allowing limited barefoot mobility [1-9]. Indications for Pirogoff amputation include foot lesions that are too extensive for reconstruction or non-operative treatment [1, 3, 4]. Contraindications include inadequate circulation of the soft tissue and calcaneal region, a painful and non-vital heel-pad, osteomyelitis or irreversible destruction of the heel-pad and/or distal tibial metaphysis and/or the calcaneus [1, 3, 4]. Relative contraindications include uncontrolled diabetes mellitus and smoking [3, 4]. Severe neuropathy and performance of this amputation on diabetic and dysvascular patients are (relatively) contraindicated [3]. However, other authors show success rates in a selected group of patients [1, 4, 10].
We present a case description of a patient who underwent a Pirogoff amputation after a traumatic injury and who encountered a difficult course afterward. In consequence of this case, we reflect on literature concerning the Pirogoff amputation. Our aim was to achieve more knowledge of the advantages and disadvantages of this amputation level, so both the surgical team and the rehabilitation team could make a balanced judgement for future patients with extensive foot lesions that cannot be reconstructed.
Case Report
A 53-year-old, healthy, male motorcyclist suffered a trauma to his right foot in a collision with a car. Hence, he incurred a complicated Lisfranc luxation fracture with multiple fractures to the (meta) tarsal bones and tarso-metatarsal joints and loss of soft tissue. No additional injury was present.
Figure 1: Schematic figures illustrating the amputation according to Pirogoff (Figure copied and modified from the study of Zinger et al.; published in NTVG in 2007 [7]).
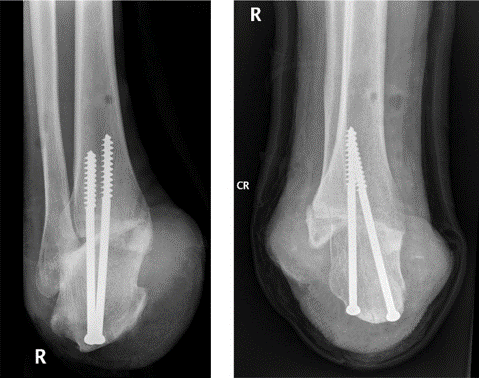
Figure 2: X-rays of the stump after Pirogoff amputation with presence of the two screws used for tibiocalcaneal arthrodesis.
Initially, reposition and external fixation was applied. Ten days after trauma, reconstruction of the tarsus was performed, and a vacuum-assisted closure system was applied. Due to progressive necrosis of the forefoot, a Pirogoff amputation was indicated, which was the most distal amputation possible. Because of excessive pus discharge, first, a guillotine amputation was performed, followed by the definitive Pirogoff amputation one week later. Two screws were used for tibio-calcaneal arthrodesis (Figure 2). Because of infection, antibiotics were prescribed, and flushing of the wound was applied for a couple of months. The first screw was removed 2.5 months after the definitive amputation, due to continuous wound problems. Afterward patient was first fitted with a temporary orthopedic shoe because of the wound problems and varying stump volume.
Approximately five months after the amputation, the wounds were closed, and the stump volume was fairly stable, so the process for prosthetic fitting was started. Prosthetic fitting was a very difficult process in which a lot of adaptations to the prosthesis were needed, and different prosthetic concepts were tried out. Problems encountered were difficulties in proper fitting of the stump due to a bulbous and irregular, bony shape, and a decreasing stump volume, accompanied by local pain and skin problems. During mobilising, the patient experienced pain during weight-bearing caused by the second screw. This screw was removed 13 months after amputation, which partially resolved the pain. It took approximately two years until the first prosthesis was made to the satisfaction of the patient. This prosthesis consisted of a polyform soft socket, a hard socket and a 1E57 Lo Rider foot (Ottobock). Because this prosthesis was longer than the 3.9 cm difference in leg-length, the patient needed a 5 mm inlay in his left shoe (Figure 3). The patient experienced this whole process as exhausting and frustrating.
Figure 3: An overview of the current situation presenting the stump and prosthesis.
Nowadays, five years after the initial trauma, the patient has still not reached his desired level of functioning. He can wear his prosthesis the whole day without pain, but he experiences limitations in longer walking and standing. He can walk 2-3 kilometres without walking aids and can stand for maximum one hour, because otherwise local skin problems arise. He only walks barefoot at night-time for toileting, using a walking frame due to experienced instability. Driving a car or bicycle is unlimited and he fully returned to work as an administrative worker.
Discussion
A major advantage of the Pirogoff amputation is the ability to bear weight on the distal stump allowing limited indoor mobility without a prosthesis. Besides, patients ambulate well with the longer stump and have a better gait pattern with less energy expenditure compared to patients with major amputations [11, 12]. Nevertheless, most of these patients wind up with severely altered gait patterns due to the non-shock absorbing nature of the final surgical construct. Furthermore, hindfoot amputations have advantages to more proximal amputations, because morbidity and mortality significantly increase as the level of amputation is more proximal, due to increased energy demands on the cardiovascular system [12-14]. Those studies predominantly included dysvascular and/or diabetic patients, and these effects probably would not apply to trauma patients.
In literature, different outcomes of Pirogoff amputation have been described. As for all amputation levels, the majority of patients requiring a foot amputation, suffer from distal foot gangrene, infection, or ischemia instead of a trauma. Complication rates for Pirogoff amputation vary from 29% to 45%, leading to major lower limb amputation in 15% to 33% of the patients [8, 15, 16]. In those studies, only 3/11 patients and 2/20 patients underwent a Pirogoff amputation after a trauma, and none of those patients suffered complications [8, 15]. In Pirogoff amputation wound healing and beginning consolidation of the tibio-calcaneal arthrodesis should be awaited before partial weight-bearing can start and be gradually increased to fully weight-bearing [3, 9, 17].
The disadvantage of the Pirogoff amputation is the limited installation height, resulting in limited choices in prosthetic feet. The limited prosthetic feet also have no shock absorbing construct, so these patients usually end up with calluses on the plantar or anterior aspect of the distal stump. Therefore, a new prosthesis should be developed, meeting the demands of restoring ankle and foot mobility together with a low installation height [18]. Besides the low installation height, the prosthetic fitting is, in our opinion, also complicated due to the bulbous distal end, compared to a conical shape in TTA. These fitting problems were the major problem in the case described, but we could not find literature concerning this problem. An experienced prosthetist should be involved early in the treatment of patients with (partial) foot amputations. Prosthetic fitting in TTA is easier, more fitting techniques are available, and, most important, there is an extensive choice in prosthetic feet to complement the requirements of different patients. Therefore, in young and healthy patients in whom there is an indication for a hindfoot amputation, a TTA could also be considered to meet the higher prosthetic demands these patients have. Obviously, these patients need to realise they will lose barefoot mobility. Little is known about the long term effects of Pirogoff amputation or TTA on elderly people who have been amputated in their younger years.
Reflecting his own situation, our patient is now content with his situation and with the ability of barefoot weight-bearing, but he regrets the fact that there is only limited choice in prosthetic feet. In literature, there is a lack of good qualitative studies, making it impossible to make a balanced judgement between the different amputation levels that can be chosen. In general, the published studies involve a small number of patients or case reports, and both good and poor results can be found. Probably, the experience of both the surgical team and the rehabilitation team will have a major influence on the outcomes of these rare amputations.
Conclusion
Our patient experienced the prosthetic fitting process as exhausting and frustrating, and he has not reached his desired level of functioning, but in the end, accepted his current status. In general, a major advantage of Pirogoff amputation is the possibility of barefoot mobility. The disadvantages are fitting problems due to a bulbous stump and limited installation height for the incorporation of a prosthesis. A TTA could be considered as an alternative amputation, with the major advantage of extensive possibilities for prosthetic fitting and prosthetic feet, which might be especially beneficial in young and healthy patients with higher prosthetic demands. The final decision of the amputation level should be made by an experienced surgical and rehabilitation team, including an experienced prosthetist, discussing the advantages and disadvantages with the patient involved. Currently, evidence from the literature is too limited to guide this discussion and the decision-making process.
Consent
Informed consent was obtained from the patient for the publication of this case.
Acknowledgments
We would like to thank the patient for his collaboration.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Tue 14, Jan 2020Accepted: Fri 31, Jan 2020
Published: Fri 07, Feb 2020
Copyright
© 2023 Annelies van der Vegt. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.02.01
Author Info
Annelies van der Vegt Joannes H.B. Geertzen Maria A. Paping
Corresponding Author
Annelies van der VegtUniversity of Groningen, University Medical Center Groningen, Department of Rehabilitation Medicine, Groningen, The Netherlands
Figures & Tables

References
- Rammelt S, Olbrich A, Zwipp H (2011) Hindfoot amputations. Oper Orthop Traumatol 23: 265-279. [Crossref]
- Malakhova O (2004) Nikolay Ivanovich Pirogoff (1810-1881). Clin Anat 17: 369-372. [Crossref]
- Langeveld AR, Meuffels DE, Oostenbroek RJ, Hoedt MT (2011) The Pirogoff amputation for necrosis of the forefoot: surgical technique. J Bone Joint Surg Am 93 Suppl 1: 21-29. [Crossref]
- Warren G (1997) Conservative amputation of the neuropathic foot- The Pirogoff procedure. Oper Orthop Traumatol 9: 49-58. [Crossref]
- Einsiedel T, Dieterich J, Kinzl L, Gebhard F, Schmelz A (2008) Lower limb salvage using Pirogoff ankle arthrodesis: minimally invasive and effective fixation with the Ilizarov external ring fixator. Orthopade 37: 143-152. [Crossref]
- Gessmann J, Citak M, Fehmer T, Schildhauer TA, Seybold D (2013) Ilizarov external frame technique for pirogoff amputations with ankle disarticulation and tibiocalcaneal fusion. Foot Ankle Int 34: 856-864. [Crossref]
- Zinger W, Holtslag HR, Verleisdonk EJ (2007) Serious foot injury: consider partial amputation designed to preserve leg-length and a weight-bearing stump. Ned Tijdschr Geneeskd 151: 789-794. [Crossref]
- Taniguchi A, Tanaka Y, Kadono K, Inada Y, Takakura Y (2003) Pirogoff ankle disarticulation as an option for ankle disarticulation. Clin Orthop Relat Res 414: 322-328. [Crossref]
- Rijken AM, Raaymakers EL (1995) The modified Pirogoff amputation for traumatic partial foot amputations. Eur J Surg 161: 237-240. [Crossref]
- Nather A, Wong KL, Lim AS, Zhaowen Ng D, Hey HW (2014) The modified Pirogoff's amputation in treating diabetic foot infections: surgical technique and case series. Diabet Foot Ankle 5. [Crossref]
- Waters RL, Perry J, Antonelli D, Hislop H (1976) Energy cost of walking of amputees: the influence of level of amputation. J Bone Joint Surg Am 58: 42-46. [Crossref]
- Pinzur MS, Gold J, Schwartz D, Gross N (1992) Energy demands for walking in dysvascular amputees as related to the level of amputation. Orthopedics 15: 1033-1036. [Crossref]
- Dillon MP, Quigley M, Fatone S (2017) Outcomes of dysvascular partial foot amputation and how these compare to transtibial amputation: a systematic review for the development of shared decision-making resources. Syst Rev 6: 54. [Crossref]
- Pohjolainen T, Alaranta H, Wikstrom J (1989) Primary survival and prosthetic fitting of lower limb amputees. Prosthet Orthot Int 13: 63-69. [Crossref]
- Bueschges M, Ottomann C, Mauss K, Muehlberger T, Bruck JC (2013) Pirogow's amputation as an alternative to lower leg amputation? Handchir Mikrochir Plast Chir 45: 67-72. [Crossref]
- Chang BB, Bock DE, Jacobs RL, Darling RC 3rd, Leather RP et al. (1994) Increased limb salvage by the use of unconventional foot amputations. J Vasc Surg 19: 341-348. [Crossref]
- Nakhgevany KB, Rhoads JE Jr (1984) Ankle-level amputation. Surgery 95: 549-552. [Crossref]
- Mulder IA, Holtslag HR, Beersma LF, Koopman BF (2014) Keep moving forward: a new energy returning prosthetic device with low installation height after Syme or Pirogoff amputation. Prosthet Orthot Int 38: 12-20. [Crossref]
