Pancreatogenic Splenic Pseudocysts: Pathogenesis, Diagnosis and Treatment
Pancreatogenic Splenic Pseudocysts: Pathogenesis, Diagnosis and Treatment
A B S T R A C T
Background: Pancreatogenic splenic pseudocysts are a relatively rare condition. Intra-splenic localization is of the splenic pseudocysts is dangerous because of the possibility of massive haemorrhage and organ rupture.
Aim: To analyse our experience in the diagnosis and treatment of pancreatogenic pseudocysts of the spleen.
Materials and Methods: The analysis of the short and long-term results of treatment of the 34 patients with pancreatogenic splenic pseudocysts (extrapancreatic localization) (1985-2019) was performed. In the study, the majority of male patients - 88.2%, the age of patients was 45 ± 7 years.
Results: Percutaneous drainage under US-control was performed in 11 (32.4%) patients, distal pancreatic resection with splenectomy was performed in 23 (67.6%) in the cases of pancreatic tail calcific pancreatitis. In all cases of percutaneous treatment, a high level of amylase was found in the fluid from pseudocysts. Bacteriological confirmation of the growth of any bacteria in the content was not obligatory. Suppuration of the fluid of the pseudocyst was observed in 85.3% of the cases.
Conclusion: Pancreatogenic pseudocysts of the spleen are one of the complications of destructive pancreatitis. They can remain undiagnosed for a long time, become infected and aggravate the course of the disease. They are often the cause of the development of sepsis and peritonitis due to the rupture of the organ capsule and bleeding into the abdominal cavity. The use of percutaneous minimally invasive methods of treatment for intra-organ pancreatogenic pseudocysts makes it possible to improve the results of treatment in this group of patients, and also, in the optimal case, be the final method of treatment.
Keywords
Pancreatogenic pseudocysts, localization, spleen, diagnosis, treatment
Introduction
Pancreatic pseudocysts are a common complication of acute and chronic pancreatitis. The localization of most pseudocysts is in the pancreas. Only 20% of pancreatogenic cysts are extrapancreatic (pleura, mediastinum, liver, spleen, stomach, pelvis, etc.) [1-3]. In rare cases, cysts move to the neck, mediastinum, chest cavity and scrotum [3]. Pseudocysts in these atypical areas are rare and present a complex diagnostic and clinical problem.
Spleen pseudocysts are rare diseases. Clinical observations of the literature are more often recorded as clinical cases [4]. The defeat of the spleen is associated with the proximity of the tail of the pancreas and gate of the spleen. The cause of pseudocysts of the spleen is the penetration of the parenchyma of the spleen by pseudocyst or penetration of pancreatic secretion into the spleen through the blood vessels [5]. Spleen lesions are often described in chronic pancreatitis [6-9]. In a study of 500 patients with chronic pancreatitis, only 5 (1%) patients with pseudocystic spleen were described [6]. R. Heider and K.E. Behrns in 2001 in their study of 238 patients (duration – 15 years), described only 14 (5.9%) pancreatogenic splenic pseudocysts [7]. Pseudocysts in the spleen are much less common in acute pancreatitis. In the study of K.J. Mortelé et al. in 100 patients with acute pancreatitis, not a single spleen pseudocyst was found according to MSCT data [10]. Most of the clinical observations of pancreatogenic splenic pseudocysts in the outcome of acute pancreatitis are isolated clinical cases [11, 12]. The main complications are perisplenic and intrasplenic pseudocysts, subcapsular and intrasplenic hematomas, splenic infarction and a ruptured spleen. The incidence of these complications has increased after the use of computed tomography for pancreatitis [13].
A pseudocyst of the spleen most often does not have any specific signs and symptoms; most patients have only abdominal pain. The presence of discomfort in the left subcostal area or pleural effusion on the left may indicate spleen involvement in pancreatitis [5-7]. Pancreatogenic splenic cysts have a high amount of amylase homogeneous fluid content due to their susceptibility to infection. Spleen abscess is a complication of destructive pancreatitis. It can often remain undiagnosed for a long time, due to the fact that the attention of surgeons is focused on eliminating pancreatogenic fluid accumulations in the parapancreatic fiber, which aggravates the course of acute pancreatitis, is the cause of the development of hemoperitoneum due to rupture of the spleen capsule and bleeding into the abdominal cavity [14]. Mortality rates in selenium pseudocysts are relatively low. R. Heider and K.E. Behrns described 14 cases; only 1 death was described after the patient was treated with external drainage [7]. Treatment of pancreatogenic splenic pseudocysts is multivariate. There is no exact cure due to the rare occurrence of this disease.
Aim
To analyse our experience in the diagnosis and treatment of pancreatogenic pseudocysts of the spleen.
Materials and Methods
The analysis of the short and long-term results of the treatment of 34 patients with pancreatogenic splenic pseudocysts (extrapancreatic localization) (1985-2019) was performed. In the study, the majority of male patients – 88.2%, the age of patients was 45 ± 7 years.
All patients underwent ultrasound examination (ultrasound) to determine the state of the spleen parenchyma, blood flow in the splenic artery and vein, as well as intra-organ blood flow. When studying the pseudocyst, were determined: localization in the organ, size, presence, and condition of the capsule, the contents of the formation, relationship with the surrounding intraorganic arteries and veins. The condition of the pancreas and retroperitoneal space was assessed too. Computed tomography or magnetic resonance imaging was used in patients with difficulties in diagnosing pseudocysts based on ultrasound results. Cyst fluid amylase was very high in pancreatogenic splenic pseudocysts.
Results
In the study, the main cause of the development of pancreatogenic splenic pseudocysts was alcoholic pancreatitis in 31 (91.2%) patients, idiopathic – 3 (8.8%). Spleen pseudocysts were diagnosed in 5 (14.7%) patients with acute pancreatitis, in 29 (85.3%) patients with chronic pancreatitis. Signs and symptoms were typical for acute and exacerbation of chronic pancreatitis. Patients in most cases had pain in the left abdomen 27 (79.4%), left hypochondrium 7 (20.6%), or a combination of both. Fever was observed in 11 (32.4%) patients and laboratory signs of inflammation, as well as in combination with pleural effusion in 29 (85.3%) patients.
The signs of pancreatitis were the most in the pancreatic tail and parapancreatic fiber in 30 (88.2%) patients, total lesion was in 4 (11.8%). 28 (82.4%) patients have pseudocysts of other localization (body-tail and / or extrapancreatic). Chronic calcific pancreatitis with a predominant lesion of the pancreatic tail was detected in 19 (65.5%) patients, in 10 (52.6%) – pancreatic hypertension and virsungolithiasis. Spleen lesion was combined with a splenic infarction in 10 (29.4%) patients, splenic vein thrombosis – in 8 (23.5%), extrahepatic portal hypertension – in 15 (44.1%) patients.
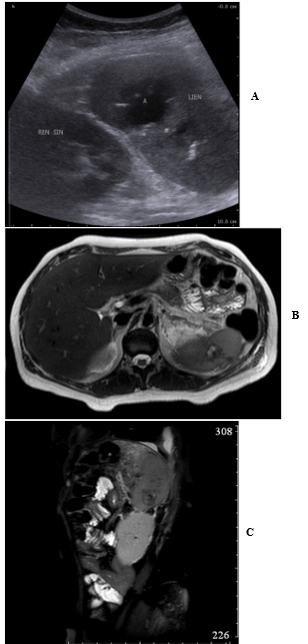
Figure 1: Patient А, 41 y. Pancreatogenic abscess of the spleen before the treatment: A) US е; B) T-2 TSE MRI; C) T2 SPAIR MRI.
The diameter of pseudocysts in the spleen was from 3 to 12 cm. 2 groups of formations can be identified according to the results of the ultrasound. The first group (21 (61.8%) patients) included lesions with inhomogeneous fluid contents of various echogenicity without sequestration; the capsule of the lesion was insignificant (Figure 1). In second group (13 (38.2%) patients), the liquid content was more heterogeneous with the presence of gas bubbles and a solid component (the structure of the formation of the type of "honeycomb"). The second group included infected pseudocysts. With prolonged infection, a capsule of uneven thickness was visualized. In 14 (41.1%) patients, more than 50% of the spleen parenchyma was replaced by non-uniform cellular cavities.
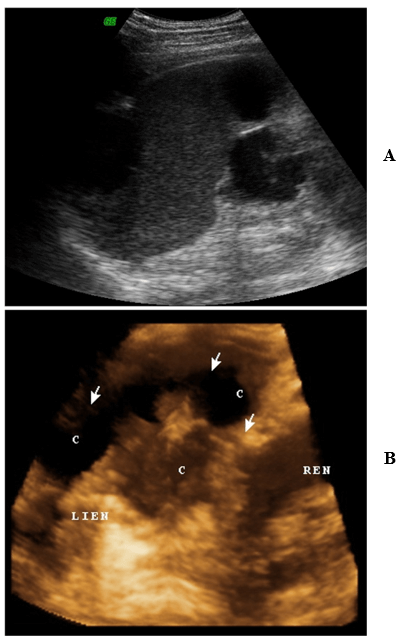
Figure 2: Patient B, 35 y. Ultrasound image of pancreatogenic spleen cysts in B-mode: A) in a two-dimensional study: B) in a three-dimensional reconstruction of a US image (c - cyst (indicated by arrows), LIEN - spleen, REN - kidney).
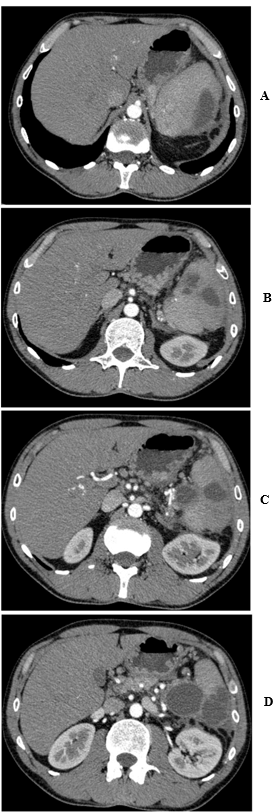
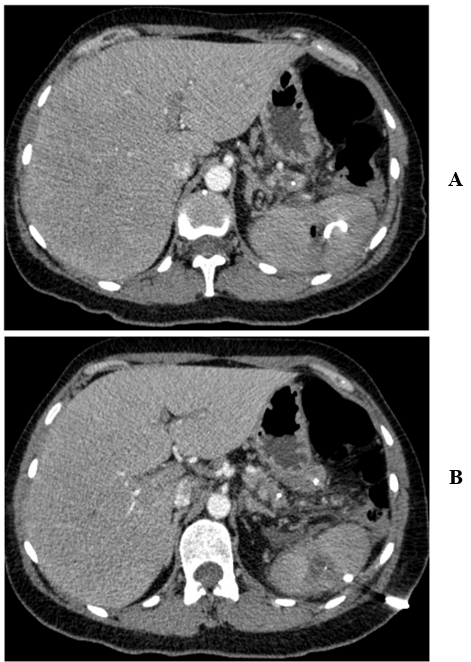
It is important to accurately determine the localization and prevalence of spleen lesions, its relationship with intraparenchymal vessels, according to ultrasound, CT and MRI data, with the possibility of using three-dimensional modeling for choosing a method of treating a patient (Figures 2 & 3). For the treatment of patients with pseudocysts of the spleen, they were divided into two groups. In the first group of patients (the presence of the ultimate path and safety of the placement of the final drainage catheter for percutaneous drainage), the first stage was percutaneous drainage of pseudocysts (Figure 4). Percutaneous drainage was the definitive method of treatment in 11 (52.4%) patients, 2 patients required stenting of the pancreatic duct. In 10 patients in the delayed period, surgical intervention was required: due to the developed bleeding into the cyst cavity – in 2; pronounced pathology in the tail of the pancreas (presence of additional cysts and calcific pancreatitis, pronounced clinical symptoms, persistent pancreatic fistula) – in 8. All patients with percutaneous treatment in the received fluid from pseudocysts revealed a high level of amylase, while bacteriological confirmation of the growth of any microflora the content was not obligate.
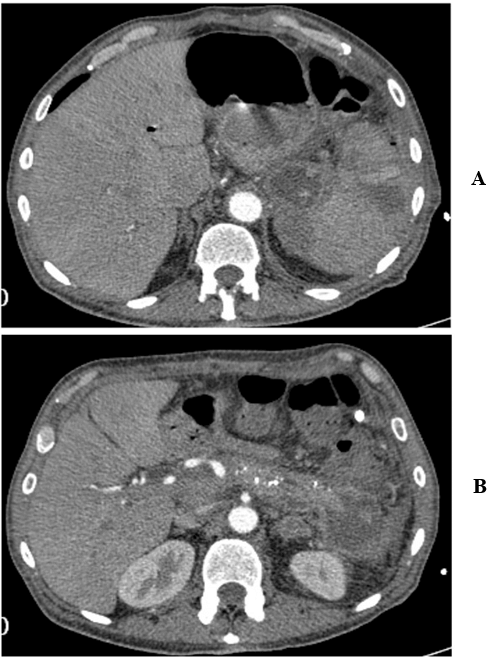
Figure 3: Patient B, 35 y. CT image of pancreatogenic spleen cysts (arterial phase of the study): A-D) sequential CT scans.
In group 2, spleen pseudocysts were abscesses, had sequesters in the cavity or a cellular nature of the formation, and/or the lesion area exceeded 50%. However, the use of percutaneous drainage is not indicated. These patients most often had a significant lesion of the distal pancreas with clinical symptoms. In this regard, this category of patients in all cases underwent distal pancreatic resection with splenectomy (Figure 5). The rate of postoperative complications was 43.4%, class III, according to Clavien-Dindo – 34.7%, 8 patients in the postoperative period required additional transcutaneous puncture and drainage. The mortality rate was 0%.
Figure 4: Patient A, 41 y. Pancreatogenic abscess of the spleen after percutaneous drainage (CT image): A) drainage in the abscess cavity; B) drainage on the anterior abdominal wall.
Figure 5: CT scans. A) Chronic calcific pancreatitis with B) spleen pancreatogenic cysts.
Discussion
Pancreatic necrosis and pseudocysts, with damage to the tail of the pancreas, can lead to complications in the spleen [15]. The frequency of the spread of pseudocysts to the spleen is from 2.2% to 5.9% [6, 7, 15]. Splenic complications in chronic pancreatitis are common in men. The etiology of pancreatitis is usually alcohol, followed by idiopathic pancreatitis, which is consistent with our results [7, 16].
The anatomical cause of spleen lesion in chronic pancreatitis is the relationship between the tail of the pancreas and the hilum of the spleen [15]. The peritoneum covers the spleen from all sides except the gate of the organ. The fibrous capsule is closely connected with the visceral peritoneum, which covers it and from the inside with the trabeculae. The distal part of the tail of the pancreas is close to the splenic vessels and enters the gate of the spleen between the two layers of the peritoneum passing into the pancreas-splenic ligament, part of the phrenicocolic ligament. The peritoneum, covering the anterior surface of the pancreas and splenic vessels, is closely connected with the spleen capsule at the hilum of the spleen. These anatomical relationships are important for determining the pathways of pancreatic secretion along the splenic vessels, reaching the splenic hilum and capsule [15, 17].
There are three types of pancreatogenic fluid accumulations: perisplenial, intrasplenic and combined. In the case of perisplenial accumulations, the fluid is located between the visceral layer of the peritoneum and the spleen capsule, without damaging it. In the case of intrasplenic pancreatic fluid accumulations, enzymatic destruction of the spleen capsule. The fluid accumulation then enters the spleen parenchyma through the destroyed capsule. Intra-splenic pseudocysts can occur due to the separation and migration of the pancreatic pseudocyst or the spread of extrapancreatic fluid through the splenic vessels. They may also appear due to pancreatitis occurring in ectopic, intrasplenic pancreatic tissue or fusion of previous splenic infarctions [18].
Damage of the tail of pancreas is the cause of the development of splenic vein thrombosis, which leads to complications from the spleen [6]. Spleen infarctions and subcapsular haemorrhages are common in acute pancreatitis [10]. Compression of the splenic artery and veins by an extensive inflammatory process can lead to local or diffuse splenic infarction, a wedge-shaped lesion is formed with an apex emanating from the hilum of the spleen and a subcapsular base [19]. In a delayed period, it can lead to subcapsular hematoma. Splenic pseudocysts, subcapsular hematomas, and ruptured spleen are common in patients with chronic pancreatitis [6, 7].
Pancreatogenic pseudocysts due to enzymatic erosion can lead to splenic vein thrombosis, splenic arterial bleeding and splenic infarction [15]. Pancreatic enzymes entering the spleen can destroy the spleen parenchyma, small intrasplenic vessels or vessels of the splenic hilus, which induces intrasplenic haemorrhage. Blood can be within the pseudocyst (intrasplenic pseudocyst) or subcapsularly in the spleen, and then a subcapsular hematoma is formed. Pancreatic enzymes can also separate the subcapsular space and cause bleeding from the splenic parenchyma. With extensive damage, destruction of the capsule or, a ruptured spleen may occur [19]. The average duration of development of splenic complications is approximately 2 years from the diagnosis of chronic pancreatitis [6]. Complications and mortality are 79% and 8% in patients with complications from the spleen, compared with complications (39%) and mortality (3.5%) and in patients without them [7].
Most patients with splenic complications of pancreatitis have symptoms of pancreatitis or pseudocysts. Signs of spleen involvement are severe pain in the left hypochondrium and pain left-sided referred shoulder pain, or the presence of a mass or an enlarged spleen on examination.
Tachycardia and hyperthermia, together with an enhanced blood tests for inflammatory markers, occur in more than half of the cases. Fluid in the left pleural sinus is a sign of splenic complications. In our study, such clinical manifestations as pain in the upper left quadrant of the abdomen and left hypochondrium left-sided referred shoulder pain prevailed. Clinical symptoms were supplemented by fever and enhanced blood tests for inflammatory markers, as well as pleural effusion [6, 15, 20, 21].
The use of ultrasound (US), computed and magnetic resonance imaging (MRI) in diagnostics is important due to the non-specificity of clinical symptoms in splenic complications [13, 22-24]. According to ultrasound examination, CT and MRI, pancreatogenic pseudocysts in the spleen are different. Literature data and observations have shown that the presence of two variants of pseudocysts is possible: heterogeneous fluid content of different echogenicity without sequestration in the cavity, the capsule of the formation is poorly expressed; more pronounced heterogeneous liquid content with the presence of gas bubbles and a solid component (structure of the formation of the type of "honeycomb"), a capsule of uneven thickness. Ultrasound is the method of choice for primary imaging. However, ultrasound may have some imaging limitations, especially in the patient which the presence of acute pancreatitis. In this case, MRI is the method of choice, since in the absence of radiation, the patient excludes the risk of nephrotoxicity and anaphylactic reactions from contrast agents. MRI is effective in clearly identifying the various components of a pseudocyst and can also detect vascular complications such as pseudoaneurysms and venous thrombosis. The application of magnetic resonance cholangiopancreatography is necessary to visualize the pancreatic duct and the presence/absence of its connection with the pseudocyst. In some cases, endo-ultrasound is also a useful method for assessing the structure of cysts, the possible presence of necrotic sequesters, especially in the case of a polycyclic form of formation with leaks. It is useful for determining the choice of treatment method, as well as in navigation [13, 20, 21].
Management of patients with pseudocysts of the spleen can be conservative, minimally invasive - ultrasound control percutaneous drainage under or endoscopic drainage or surgical [7]. Management depends on the size of the pancreatogenic pseudocyst of the spleen, its topography and the presence/absence of a connection with the pancreatic duct. For small cysts, a conservative approach is considered effective [20]. Conservative therapy should be preferred, if possible, due to the high incidence of infectious complications after splenectomy. Patients with minimal symptoms and positive dynamics can be treated conservatively in order to preserve the spleen. Evaluation of the dynamics is carried out according to the data of ultrasound, CT or MRI [25]. The time for regression of a splenic cyst ranges from one week to four months, depending on the severity of the manifestations of underlying pancreatitis [7]. For large cysts, percutaneous drainage, endoscopic drainage (if the cyst is adjacent to the stomach) or splenectomy (open or laparoscopic) is used [7]. Most authors prefer minimally invasive percutaneous drainage of such patients; however, there are no clear indications in which cases the use of this method of treatment is indicated, and in which it is indicated surgical [26-28]. In our study, 32.4% of patients underwent only minimally invasive treatment.
Endoscopic drainage of a pseudocyst is becoming more and more important. It is a safe and effective minimally invasive method of treating spleen pseudocysts, especially in the absence of infection and there are no large necrotic sequestrations. Endoscopic drainage depends on the anatomy and topography of the pseudocyst and can be performed transpapillary (using endoscopic retrograde cholangiopancreatography) or transmurally. Transpapillary drainage is safer and more effective than transmural drainage, but the cyst must communicate with the pancreatic duct [20, 29].
Open surgery is used for extensive lesions of the spleen, the presence of a cyst with a cellular structure (abscess) or a cyst in the hilum of the spleen, there are several cysts, as well as for significant manifestations of extrasplenic pancreatitis [21]. In our study, the indications for performing distal resection of the pancreas with splenectomy were heterogeneous cyst contents with a predominance of the cellular component and an area of spleen lesion of more than 50% in 39.4% of cases.
In the case of ruptured spleen due to the presence of a pancreatogenic pseudocyst or hemoperitoneum and the patient's severe condition, emergency care is indicated - laparotomy and either splenectomy or distal pancreatosplenectomy, which can potentially reduce the risk of bleeding or fistula formation [7]. If a patient has stable hemodynamics, the decision on the method of intervention should be based on clinical evidence. Patients with splenic vein thrombosis and local (segmental) portal hypertension are at high risk of ruptured spleen and expectant management can be dangerous [6]. In patients with massive damage to the splenic parenchyma or signs of perisplenal bleeding, it may be necessary to embolize the splenic artery [20].
For determining the tactics of managing, a multidisciplinary approach is required for a correct and complete assessment of all manifestations and their severity due to the fact that the cause of the development of pancreatogenic pseudocyst of the spleen is pancreatitis, which can have various manifestations, in addition to this cyst. It is advisable to involve a gastroenterologist, a radiologist, an interventional radiologist, an endoscopist and a surgeon. Such a multidisciplinary approach to assessing the clinical situation will allow you to choose the most effective treatment tactics for a particular patient.
Conclusion
The course of acute and chronic pancreatitis can be with the formation of post necrotic cysts. Pancreatogenic cysts in the spleen are uncommon. More often, they are not detected immediately, since their clinical manifestations are masked by the manifestations of the underlying disease – pancreatitis. Their manifestations can be different: from pain in the left upper abdominal square to haemorrhagic shock with rupture of the spleen in the case of localization in the spleen and septic manifestations in the case of localization in the liver. Evaluation of signs and symptoms, results of radiation research methods will give an understanding of complications from the spleen and liver.
When a pancreatogenic cyst is localized in the spleen, it is indicated to begin the treatment of stable patients conservatively (percutaneous drainage if necessary). Active surgical tactics are indicated in the presence of a cyst with a cellular structure (abscess), massive damage to the spleen parenchyma, fistula of a pseudocyst with a duct system, splenic vein thrombosis or partial portal hypertension. Preventive embolization of the splenic artery is indicated in hemodynamically unstable patients as a first step. If a patient has stable hemodynamics with a ruptured spleen and hemoperitoneum, require urgent surgery. The management of these patients will depend on the availability of percutaneous and surgical treatment, and, if necessary, the patient should be referred to a multidisciplinary specialized institution.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 17, Aug 2020Accepted: Fri 11, Sep 2020
Published: Fri 25, Sep 2020
Copyright
© 2023 Stepanova Yulia Aleksandrovna. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.09.11
Author Info
Stepanova Yulia Aleksandrovna Ionkin Dmitry M.Z. Alimurzaeva O.I. Zhavoronkova Ya.Ya. Gavrilov A.A. Olifir
Corresponding Author
Stepanova Yulia AleksandrovnaA.V. Vishnevsky National Medical Research Center of Surgery, Russia
Figures & Tables
References
- Hamm B, Franzen N (1993) Atypically located pancreatic pseudocysts in the liver, spleen, stomach wall and mediastinum: their CT diagnosis. Rofo 159: 522-527. [Crossref]
- Guesmi F, Zoghlami A, Saidi Y, Najeh N, Dziri C (2009) Pancreatic pseudocysts located in the liver: a systematic review of the literature. Tunis Med 87: 801-804. [Crossref]
- Accetta P, Accetta I, Accetta R, Campos K B, Rodrigues M F O (2010) Pancreatic pseudocyst with splenic involvement. Case report. Rev Col Bras Cir 37: 457-459. [Crossref]
- Rana S S, Chaudhary V, Sharma V, Sharma R, Dutta U et al. (2014) Infected pancreatic pseudocyst of spleen successfully treated by combined endoscopic transpapillary stent placement and transmural aspiration. Gastrointest Endosc 79: 360-361. [Crossref]
- Patil P V, Khalil A, Thaha M A (2011) Splenic parenchymal complications in pancreatitis. JOP 12: 287-291. [Crossref]
- Malka D, Hammel P, Lévy P, Sauvanet A, Ruszniewski P et al. (1998) Splenic complications in chronic pancreatitis: prevalence and risk factors in a medical-surgical series of 500 patients. Br J Surg 85: 1645-1649. [Crossref]
- Heider R, Behrns K E (2001) Pancreatic pseudocysts complicated by splenic parenchymal involvement: results of operative and percutaneous management. Pancreas 23: 20-25. [Crossref]
- Siu T L T (2004) Percutaneous drainage of spontaneous subcapsular haematoma of the spleen complicating chronic pancreatitis. Surgeon 2: 52-55. [Crossref]
- Fung H Y, Chiu H H, Li J H, Huang C C (2009) Pancreatic tail pseudocyst associated with spontaneous resolution of intrasplenic pancreatic pseudocyst. Am J Surg 197: e46-e47. [Crossref]
- Mortelé K J, Mergo P J, Taylor H M, Ernst M D, Ros P R (2001) Splenic and perisplenic involvement in acute pancreatitis: determination of prevalence and morphologic helical CT features. J Comput Assist Tomogr 25: 50-54. [Crossref]
- Lee H N, Lee T H, Ryu K H, Rim S M, Jeong I B et al. (2012) A case of splenic pseudocyst complicated by acute pancreatitis. Korean J Gastroenterol 59: 193-196. [Crossref]
- Trivedi H, Shuja A, Shah B B (2015) Intrasplenic Pancreatic Pseudocyst: A Rare Complication of Acute Pancreatitis. ACG Case Rep J 2: 202-203. [Crossref]
- Rypens F, Devière J, Zalcman M, Braudé P, Stadt J V D et al. (1997) Splenic parenchymal complications of pancreatitis: CT findings and natural history. J Comput Assist Tomogr 21: 89-93. [Crossref]
- Herrera H B, Lledó J B, Navarro S C, Soto A S, Burgueño M D J (2011) Ruptured spleen due to a pancreatic pseudocyst. Cir Esp 89: 120-122. [Crossref]
- Lankisch P G (1990) The spleen in inflammatory pancreatic disease. Gastroenterology 98: 509-516. [Crossref]
- Hokama A, Maeda K, Tomiyama R, Hirata T, Kinjo F et al. (2004) Intrasplenic pancreatic pseudocysts. JOP 5: 235-236. [Crossref]
- Fishman E K, Soyer P, Bliss D F, Bluemke D A, Devine N (1995) Splenic involvement in pancreatitis: spectrum of CT findings. Am J Roentgenol 164: 631-635. [Crossref]
- Wang S J, Chen J J, Changchien C S, Chiou S S, Tai D I et al. (1993) Sequential invasions of pancreatic pseudocysts in pancreatic tail, hepatic left lobe, caudate lobe, and spleen. Pancreas 8: 133-136. [Crossref]
- Vujic I (1989) Vascular complications of pancreatitis. Radiol Clin North Am 27: 81-91. [Crossref]
- Goyal S, Goyal S, Garg M K, Garg U (2014) Pseudopancreatic cyst invasion into spleen: Case report and review. J Mahatma Gandhi Inst Med Sci 19: 151-154.
- Rodriguez E, Silva J M, Astani S A (2017) Giant splenic pseudocyst. Appl Radiol 46: 40-42.
- Miller F H, A L, Dalal K, Ly J N, Kamler V A et al. (2004) MRI of pancreatitis and its complications: Part 1, Acute pancreatitis. AJR Am J Roentgenol 183: 1637-1644. [Crossref]
- Fung H Y, Chiu H H, Li J H, Huang C C (2009) Pancreatic tail pseudocyst associated with spontaneous resolution of intrasplenic pancreatic pseudocyst. Am J Surg 197: e46-e47. [Crossref]
- Stepanova Y A, Panchenkov D N (2009) The private section of diagnostics and treatment with application of the ultrasonic and/or combined navigation. In book: “Minimally invasive technologies under ultrasonic navigation in modern clinical practice". Ed. A V Borsukov, V N Sholokhov. Practical guidance for postdegree vocational training of doctors. - Smolensk: Smolensk city printing house 141-231.
- Patel V G, Eltayeb O M, Zakaria M, Fortson J K, Weaver W L (2005) Spontaneous subcapsular splenic hematoma: a rare complication of pancreatitis. Am Surg 71: 1066-1069. [Crossref]
- Onopriyev V I, Shcherbina I I (1999) Way of surgical treatment of the infected pancreatic pseudo-cysts of a spleen. The patent of Russian Federation №2143286.
- Neri V, Ambrosi A, Fersini A, Tartaglia N, Valentino T P (2009) Minimally Invasive Treatment of Acute Intrahepatic Fluid Collections with Acute Biliary Pancreatitis. JSLS 13: 269-272. [Crossref]
- Melekhina O V, Zhavoronkova O I, Stepanova Y A, Ionkin D A (2014) Pancreatogenic pseudocysts of the liver and spleen: pathogenesis, diagnosis and treatment tactics. Ann Surg Hepatol 4: 39-47.
- Rana S S, Sharma R, Chhabra P, Sharma V, Gupta R et al. (2016) Endoscopic management of splenic pseudocysts associated with acute and chronic pancreatitis. Ann Gastroenterol 29: 373-377. [Crossref]
