Necrotizing Fasciitis of The Abdominal Wall Following Colonoscopy with Fatal Outcome - A Case Report
A B S T R A C T
Necrotizing fasciitis (NF) is a serious and potentially life threatening soft tissue infection, usually caused by different types of bacteria such as group A streptococcus, staphylococcus spp. (type 1 infection) or mixed infection by aerobic and anaerobic bacteria (type 2 infection). Usually, the infection arises from skin injury, in injections or surgical procedures and effects the fascia as well as the subcutaneous tissue. Overwhelming progression and difficulties in diagnosing are very common. Mortality rate is up to 100% depending on the type of soft tissue infection and did not markedly decrease in the past decades [1]. Here we present a case of NF with fatal outcome following colonoscopy, which was primarily suspected to be a post polypectomy syndrome.
Keywords
necrotizing fasciitis, colonoscopy, post polypectomy syndrome, soft tissue infection
Case Report
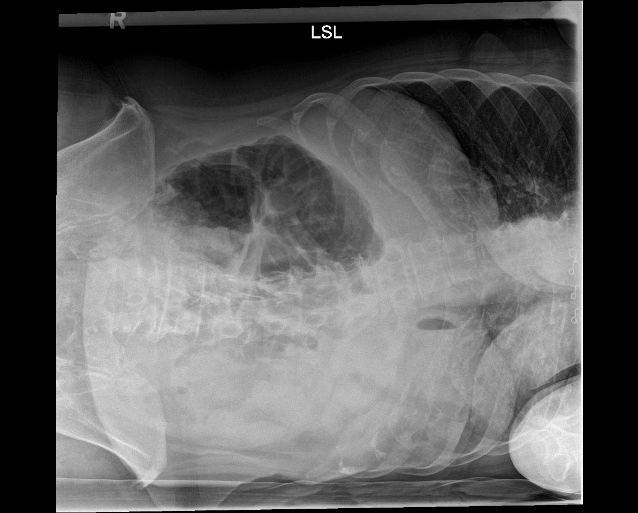
A 70-year-old woman was admitted to our hospital with sudden onset of right lower quadrant pain which started 7 hours ago. The day before she underwent elective colonoscopy for surveillance of sessile polyps in her right colon. A single sessile polyp was removed via snare without problems. Her past medical history revealed presence of type II diabetes and arterial hypertension. Clinical examination revealed tenderness on palpation in the right lower quadrant of her abdomen without signs of peritonism. There was no crepitation of the abdominal wall and no signs of sepsis, as she was not tachycardic, hypotonic or showing hyperventilation, her body temperature was normal (36,4°C). Her laboratory results were as followed: leukocytes: 17.9/nl, CRP: 12mg/dl, sodium 134 mmol/l, creatinin: 0.91 mg/dl, hemoglobin: 14,5 g/dl, blood glucose level 247 mg/dl. An abdominal X-ray examination was carried out to rule out a perforation of the large bowel (Figure 1). As the x-ray examination was negative for perforation, the patient was taken to the ward for close observation, administration of pain killers and i.v. fluids. As post polypectomy syndrome was suspected a first generation cephalosporine was administered.
About 7 hours after admission her clinical conditions significantly deteriorated as she developed peritonism in the right lower quadrant without local crepitations. An urgent CT scan (Figure 2) was performed to rule out a perforation of the colon. Unexpectedly, trapped air was seen in the right sided abdominal wall without signs of colonic perforation. Immediately antibiotic therapy was adapted to broad spectrum antibiotics and an emergency laparotomy was carried out. Intraoperatively, a local peritonitis was seen at the site of parietal peritoneum of the right lower abdominal wall. The trapped air, localized retroperitoneally, had the appearance of a gas filled bubble. The ascending colon was mobilized, and no perforation or lesion was seen at the colon, nor there was trapped air dorsally to the fascia of Toldt or in the meso of the colon. The parietal peritoneum was than incised and a fecal smell was noticed. Wound swabs were taken, and the typical aspect of a necrotizing fasciitis was noticed. Consecutively, the abdominal wall was debrided radically. The retroperitoneal air reached the pararectal space, and therefore a proctoscopy and a complete intraoperative colonoscopy was undertaken but could not detect a defect in the rectal nor in the colonic wall. There was no aspect of a Fournier’s gangrene in the perianal aspect.
An intraperitoneal drainage was placed, and the abdomen closed consecutively. As the clinical aspect of necrotizing fasciitis was observed, the antibiotic treatment was amended to Meropenem, Clindamycine and Penicillin G. Postoperatively the patient directly was taken to intensive care unit. A 2nd look laparotomy was planned for the following day. Reevaluation of the patient at the day after primary surgery revealed hemodynamic stable conditions, the abdominal wall presented inconspicuous. Just one hour later, the patient presented with livid discoloration and crepitating of the right abdominal wall and septic conditions. She was about to be taken to the operating room when she had to be resuscitated twice and died. The blood samples, taken just before, were macroscopically hemolytic. The drainage showed hemolytic fluid, too.
Figure 1: plain abdominal X-ray showing no significant pathology.
Figure 2: CT scan of the abdomen showing trapped air in the right abdominal wall extending into the pelvis. A perforation of viscera was ruled out.
Discussion
Necrotizing fasciitis was primarily described in the 1950s by B. Wilson and is known to be associated with high mortality rates, which didn`t decrease significantly since [2, 3]. Clinical diagnosing remains to be difficult due to diagnostic pitfalls [1]. In our case, a postpolypectomy electrocoagulation syndrome (PPS) primarily was suspected as there was no reason to suspect NF in terms of the patient`s anamnesis. PPS usually occurs after polypectomy with electrocoagulation and refers to abdominal pain with local tenderness, leukocytosis and the absence of bowel perforation, which could be ruled out in plain X-ray examination. The incidence of PPS varies widely and ranges from 0,003% to 0,1 % in the literature and presents 1 to 5 days after colonoscopy [4-6]. As the PPS is the result of a transmural burn of the colon without perforation, due to the applied electrical current, it can result in local inflammation of the serosa with the signs of localized peritonitis or pain [7]. This is exactly what our patient presented with.
In the latest literature, scoring systems are supposed to be useful in recognizing NF. The LRINEC score (laboratory risk indicator for necrotizing fasciitis) published by Wong et al. is one of these and estimates the probability of NF and the necessity for surgical treatment [8]. In our case the LRINEC score equates to 4 points, which was low risk for NF. - Recently, a systematic literature review was published, showing a positive correlation between LRINEC score and a true diagnosis of NF [9]. Other authors argue, that clinical impression and presentation of the patient should trump this score which must be supported due to our case [10]. Putnam et al. reported a median LRINEC score of 3.7 involving children with NF [11].
From microbiological point of view, 2 types of NF can be distinguished. In type I infection at least one anaerobic bacterial species can be isolated combined with one or more facultative anaerobic streptococci (not group A) and enterobacteriaceae species [12-14]. Typically, NF of the head and neck region are caused by mouth anaerobes. Surprisingly, streptococcus mitis, a member of the oral flora was isolated in the blood cultures of our patient. This might lead to the assumption, that hematogenic spreading was etiologically, but in relation to time of colonoscopy and the beginning of clinical symptoms this is very implausible. Type II NF typically is a monobacterial infection. Among gram-positive organisms, group A streptococcus remains the most common pathogen followed by methicillin-resistant Staphylococcus aureus (MRSA) [1].
Radiological findings of primary plain X-ray were not helpful in the present case for the diagnose of NF as there was no fascial edema, fluid collections or gas seen tracking along the fascial planes. Finally, the non-contrast CT scan of the abdomen revealed trapped gas formation in right sided abdominal wall. Gas formation is a typical finding in type I NF in CT scan with a high specificity but low sensitivity [12]. The CT hallmark of soft-tissue air with deep fascial fluid collections is not always seen, and its absence should not prompt exclusion of necrotizing fasciitis because the patient may have early disease in which gas has not yet formed or reached detectable levels [15]. It needs to be remarked, that in the presence of clinical signs such as progressive soft tissue infection or crepitation of skin, radiographic imaging should not delay early surgical intervention when NF is suspected [16]. In our case there was no clinical evidence for progressive soft tissue infection, in particular there was no noticeable crepitation of the skin when the CT scan was performed.
Usually, factors as recent surgery, traumatic wounds, diabetes, immunosuppression and obesity are associated risk factors for NF whereas colonoscopy, in the context of polypectomy and NF of the abdominal wall is not reported in the literature [1, 12]. A breach of the gastrointestinal mucosa may result into Fournier`s gangrene, which begins abruptly with severe pain [1]. Consecutively, our patient was under risk as she was suffering from diabetes. Obviously, diabetes seems to be a particularly important risk factor for NF, as it occurs more frequently among diabetics. Retrospectively, in our case type I infection was present, as our patient had typical risk factors such as diabetes and the detection of non-group A streptococci in blood cultures. Furthermore, there was no presence of trauma. Apart from unspecific blood test results and mild pain in her right lower abdomen, there were no sensitive clinical signs which might have led to the early diagnosis of a necrotizing soft tissue infection.
Conclusion
The current case dramatically represents the consequences of NF and underlines the high mortality rate. In conclusion interventional procedures, such as polypectomies whilst colonoscopy might be comparable with surgical procedures as a triggering cause of NF and therefore should be taken in consideration as a potential differential diagnosis to bowel perforation or post polypectomy syndrome. Clinical suspicion and symptoms should trigger early CT scan, in particular when plain X-ray examination is inconspicuous, and patient is not in septic conditions and risk factors for NF are present. Though, early surgical intervention combined with antibiotic treatment should be performed immediately and unnecessary diagnostics should be avoided when necrotizing soft tissue infection is clinically suspected. To our knowledge and as per Medline search using the MeSH terms “NF” and “colonoscopy”, this is the very first case of NF after colonoscopy in published English literature.
Conflicts of interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Tue 24, Sep 2019Accepted: Wed 09, Oct 2019
Published: Wed 30, Oct 2019
Copyright
© 2023 Daniel Matz. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.05.06
Author Info
Corresponding Author
Daniel MatzDepartment of General, Visceral and Thoracic Surgery, AGAPLESION Diakonie Hospital Rotenburg (Wuemme), Elise Averdieck-Str. 17, 27356 Rotenburg (Wuemme), Germany
Figures & Tables

References
- Stevens DL, Bryant AE (2017) Necrotizing Soft-Tissue Infections. N Engl J Med 377: 2253-2265. [Crossref]
- Wilson B (1952) Necrotizing fasciitis. Am Surg 18(4): 416-431. [Crossref]
- Leitch HA, PalepuA, Fernandes CM (2000) Necrotizing fasciitis secondary to group A streptococcus. Morbidity and mortality still high. Can Fam Physician 46: 1460-1466. [Crossref]
- Cha JM, Lim KS, Lee SH, Joo YE, Hong SP et al. (2013) Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy 45: 202-207. [Crossref]
- Ko CW, Dominitz JA (2010) Complications of colonoscopy: magnitude and management. Gastrointest Endosc Clin N Am 20: 659-671. [Crossref]
- Kim HW (2014) What Is Different between Postpolypectomy Fever and Postpolypectomy Coagulation Syndrome? Clin Endosc 47: 205-206. [Crossref]
- Christie JP, Marrazzo J 3rd (1991) "Mini-perforation" of the colon--not all postpolypectomy perforations require laparotomy. Dis Colon Rectum 34: 132-135. [Crossref]
- Wong CH, Khin LW, Heng KS, Tan KC, Low CO (2004) The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 32: 1535-1541. [Crossref]
- Bechar J, Sepehripour S, Hardwicke J, Filobbos G (2017) Laboratory risk indicator for necrotising fasciitis (LRINEC) score for the assessment of early necrotising fasciitis: a systematic review of the literature. Ann R Coll Surg Engl 99: 341-346. [Crossref]
- Wilson MP, Schneir AB (2013) A case of necrotizing fasciitis with a LRINEC score of zero: clinical suspicion should trump scoring systems. J Emerg Med 44: 928-931. [Crossref]
- Putnam LR, Richards MK, Sandvall BK, Hopper RA, Waldhausen JH et al. (2016) Laboratory evaluation for pediatric patients with suspected necrotizing soft tissue infections: A case-control study. J Pediatr Surg 51: 1022-1025. [Crossref]
- Anaya DA, Dellinger EP (2007) Necrotizing soft-tissue infection: diagnosis and management. Clin Infect Dis 44: 705-710. [Crossref]
- Brook I, Frazie EH (1995) Clinical and microbiological features of necrotizing fasciitis. J Clin Microbiol 33: 2382-2387. [Crossref]
- Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL et al. (2003) Necrotizing fasciitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 85: 1454-1460. [Crossref]
- Turecki MB, Taljanovic MS, Stubbs AY, Graham AR, Holden DA et al. (2010) Imaging of musculoskeletal soft tissue infections. Skeletal Radiol 39: 957-971. [Crossref]
- Stevens DL, Tanner MH, Winship J, Swarts R, Ries KM et al. (1989) Severe group A streptococcal infections associated with a toxic shock-like syndrome and scarlet fever toxin A. N Engl J Med 321: 1-7. [Crossref]
