Nasal Septal Abscess Complicating Acute Sinusitis in an 8-Year-Old Child: A Case Report
A B S T R A C T
Introduction: Nasal septal abscess (NSA) in the pediatric population is an uncommon condition, but it can cause devastating complications (such as potentially life-threatening intracranial infections and cosmetic nasal deformity). The objective of this study is to report a case of an pediatric patient presenting with NSA in association with frontal-ethmoid acute sinusitis and intracranial abscess.
Method and Results: In this study, we report a case of an 8-year-old patient who progressed from spontaneous nasal septal abscess to sinusitis (maxillary, frontal and ethmoidal), cosmetic nasal deformity (destruction of septal cartilage) and intracranial complication. The purulent collection necessitated urgent surgical drainage and adequate medical treatment.
Conclusion: Nasal septal abscess in children is a rare condition that necessitates early appropriate drainage in order to prevent severe life-threatening complications. Furthermore, in the growing child, in case of total destruction of the cartilaginous septum, immediate reconstruction with autologous cartilage graft is essential for normal development of the nose and maxilla.
Keywords
Nasal septal abscess, acute sinusitis, head and neck infection, intracranial abscess, pediatric sinusitis
Introduction
Nasal septal abscess (NSA) is defined as a collection of pus between the nasal septal cartilage and the overlying mucoperichondrium or mucoperiosteum, with most cases affecting the anterior septal cartilage [1, 2]. This rare entity, usually presenting after trauma to the nose, can result in devastating complications. On clinical examination, the nasal septum appears swollen on one or both sides, with a bluish or reddish colour over the mucosa, with symptoms of nasal obstruction and facial pain. The surgical drainage must be prompt to prevent severe life-threatening complications, such as devascularization of the septal mucoperichondrium leading to cartilaginous destruction, osteomyelitis, orbital and intracranial abscess, meningitis, and cavernous sinus thrombosis [1-5]. We report the clinical, radiologic, and histopathologic findings for NSA in an 8-year-old boy complicated with a right maxillary, ethmoid and frontal sinusitis and intracranial abscess.
Case Report
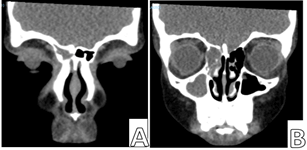
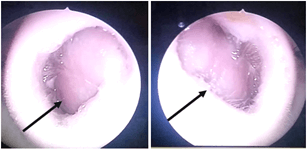
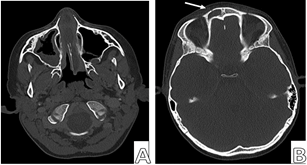
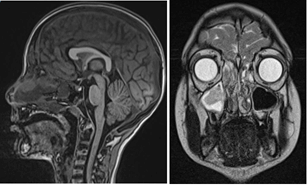
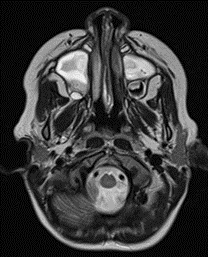
An 8-year-old boy presented to the Emergency department of our tertiary children’s hospital with a progressive, worsening and painful, right peri-orbital oedema extending over the right cheek and nasal ridge for five days. He also complained of bilateral nasal obstruction of seven days duration. The child was initially treated with systemic antibiotics (Amoxicillin/Clavulanate) and oral corticosteroids by his family physician, without benefits, for a diagnosis of acute monolateral pansinusitis (maxillary-ethmoid and frontal), made in another hospital with the use of CT scan (Figure 1). At the emergency room, the child was febrile with 38° Celsius. Blood study revealed a white cell count of 31.0×103 /uL with a differential count of 87.7% neutrophils. Physical examination revealed bilateral dull red-purple swelling of the nasal septum (Figure 2). Otoscopy, oral cavity and neck examination were unremarkable, such as the post-nasal space. A plain-axial urgent sinus computed tomography (CT) revealed NSA with opacified right maxillary, ethmoid and frontal sinuses. Bone abnormalities of the frontal sinus and continuity with the intracranial space are also observed (Figure 3). The magnetic resonance (MRI) with contrast confirmed the diagnosis of nasal septal abscess complicated by acute sinusitis and the presence of intracranial subdural abscess (Figure 4). The patient was started on intravenous ceftriaxone and systemic corticosteroid.
Figure 1: Coronal CT scan of the paranasal sinuses which demonstrates the right frontal A) maxillary-ethmoid sinus B) opacification.
Figure 2: Right and left nostril: obstruction due to significant septal swelling (arrow).
Figure 3: Axial CT scan of the paranasal sinuses; A) nasal septal abscess; B) presence of bone interruption and continuity with the intracranial space (white narrow).
Figure 4: Magnetic resonance imaging studies performed on the day of TC. The imagines confirmed the presence of nostril obstruction and intracranial abscess.
On the second day of hospitalization, the patient was taken to the operating room: after local infiltration of 2% lidocaine and 1:80 000 adrenaline into the left nasal septal mucosa, a septal incision was made and the nasal abscess was drained (Figure 5). An aspirate from mucopurulental secretions was sent to the laboratory for culture, but this did not grow any pathogens. After, a nasal endoscopy was performed to ensure the drainage of maxillary-ethmoid and frontal sinuses and a Jackson Pratt drain was inserted into the frontal sinus to prevent a re-accumulation of fluid [6]. At the end of procedure, bilateral n° 8 Merocel nasal packing was inserted. The frontal sinus drain was kept in situ for six days. Ten days post-treatment MRI of the paranasal sinuses also showed resolution of the nasal septal abscess and of the intracranial subdural abscess (Figure 6). The patient responded well to drainage of pus and medical management and was discharged after full recovery in 3 weeks on oral antibiotic therapy for a week.
Figure 5: Septal incision and nasal abscess was drained.
Figure 6: MRI of the paranasal sinuses performed 10 days after intervention showed resolution of the nasal septal abscess intracranial subdural abscess.
Discussion
Nasal septum abscess (NSA) is defined as a collection of pus in the subperichondrial/subperiosteal plane of the septum. In the antibiotics era, NSA is a rare condition that occurs mostly in children, with a male predominance (male: female ratio ranging from 2:1 to 6:1) [7]. According to the literature, the majority (>70%) of NSA cases typically result from trauma that induces hematoma that become infected, separating the mucoperichondrium from the nasal septum, leading to ischaemia and necrosis of the septal cartilage [3, 7, 8]. Major causes of non-traumatic NSA are sinusitis, vestibulitis, dental pathologies and, more rarely, spontaneous cases [8]. NSA, when associated with acute sinusitis (AS) has been proposed to result from contiguous spread of infection along tissue planes and/or under the periosteum/perichondrium [8, 9]. According to the literature, the majority of AS-associated NSA cases involved the ethmoid and sphenoid sinuses, more rarely the frontal sinus [9, 10]. Generally, NSA patients present with nasal obstruction, facial pain, fever, general malaise and, in case of delayed diagnosis, cosmetic deformity of the nose or intracranial complication [7, 10]. The characteristic appearance of NSA on anterior rhinoscopy and nasal endoscopy is septal swelling, usually bilateral due to septal cartilage reabsorption as a consequence of ischaemia and necrosis [10, 11]. Our patient’s case shows that a timely diagnosis is important in case of NSA because delayed treatment may lead to life-threatening complications such as intracranial abscess or cosmetic deformities [9, 11-13]. After appropriate radiological investigation, immediate surgical bilateral drainage of abscess is necessary, along with parenteral antibiotic therapy. In our case, the septal cartilage destruction was minimal and no reconstruction was needed at the time of drainage.
Conclusion
The most common presentation of NSA is bilateral nasal obstruction. Sinus CT-scan is an excellent diagnostic tool for detection of the presence of the subperichondrial/subperiosteal abscesses, and identification of possible causes and complications. Although, to date is an uncommon pathology, NSA can lead to important complications, so early diagnosis and immediate surgical intervention are mandatory, along with parental antibiotics treatment.
Conflicts of Interest
The study has not received funding from any organization or institution and does not involve any potential conflict of interest (financial and non-financial).
Ethical Approval
Procedure performed in the study was in accordance with the ethical standards of the institution and with the 1964 Helsinki declaration and its later amendments.
Article Info
Article Type
Case ReportPublication history
Received: Sat 20, Nov 2021Accepted: Tue 07, Dec 2021
Published: Thu 30, Dec 2021
Copyright
© 2023 Fabrizio Cialente. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.12.02
Author Info
Fabrizio Cialente Giovanni Carlo De Vincentiis Sara Santarsiero Trozzi Marilena
Corresponding Author
Fabrizio CialenteSurgery Unit, Derpartment of Surgical Specialties, Bambino Gesù Children's Hospital, Piazza Sant'Onofrio, Rome, Italy
Figures & Tables

References
1. Kop EA, Lodder WL,
de Visscher JG, van den Berge H (2020) Nasal Septal Abscess Caused by
Protrusion of a Dental Implant Into the Nasopalatine Duct: A Case Report. Ann
Otol Rhinol Laryngol 129: 633-636. [Crossref]
2. Gradoni P, Fois P
(2010) Nasal septal abscess complicating isolated acute sphenoiditis: case
report and literature review. B-ENT 6: 303-305. [Crossref]
3. Pang KP, Sethi DS
(2002) Nasal septal abscess: an unusual complication of acute
spheno-ethmoiditis. J Laryngol Otol 116: 543-545. [Crossref]
4. Lin IH, Huang IS
(2007) Nasal septal abscess complicated with acute sinusitis and facial
cellulitis in a child. Auris Nasus Larynx 34: 241-243. [Crossref]
5. Magnano M, Ferrero
V, Morra B, Bussi M (1992) Orbital and endocranial complications in acute
sinusitis in childhood. Acta Otorhinolaryngol Ital 12: 565-573. [Crossref]
6. Minni A, Roncoroni
L, Cialente F, Zoccali F, Colizza A et al. (2021) Surgical Approach to Frontal
and Ethmoid Sinus Osteomas: The Experience of 2 Metropolitan Italian Hospitals.
Ear Nose Throat J 28: 1455613211016895. [Crossref]
7. Alshaikh N, Lo S
(2011) Nasal septal abscess in children: from diagnosis to management and
prevention. Int J Pediatr Otorhinolaryngol 75: 737-744. [Crossref]
8. Canty PA, Berkowitz
RG (1996) Hematoma and abscess of the nasal septum in children. Arch
Otolaryngol Head Neck Surg 122: 1373-1376. [Crossref]
9. Tien DA, Krakovitz
P, Anne S (2016) Nasal septal abscess in association with pediatric acute
rhinosinusitis. Int J Pediatr Otorhinolaryngol 91: 27-29. [Crossref]
10. Ambrus PS, Eavey
RD, Baker AS, Wilson WR, Kelly JH (1981) Management of nasal septal abscess. Laryngoscope
91: 575-582. [Crossref]
11. Hyo Y, Fukushima H,
Harada T, Hara H (2018) Nasal septal abscess caused by anaerobic bacteria of
oral flora. Auris Nasus Larynx 46: 147-150. [Crossref]
12. Maan AS, Kaur G, Arora R, Kaur J, Devi KJ et al. (2020) An Unusual Case of a Pediatric Nasal Septal Abscess with Life-Threatening Complications in COVID-19 Pandemic. Indian J Otolaryngol Head Neck Surg 11: 1-4. [Crossref]
13. Dispenza C, Saraniti C, Dispenza F, Caramanna C, Salzano FA (2004) Management of nasal septal abscess in childhood: our experience. Int J Pediatr Otorhinolaryngol 68: 1417-1421. [Crossref]
