Minimally Invasive Removal of Shrapnel Using a Tubular Retractor System
A B S T R A C T
Background: The removal of small, metallic shrapnel fragments can be challenging, but may be indicated for pain, migration, infection, toxicity, etc.
Methods: We report the novel use of minimally invasive spine surgery technology to remove a shrapnel fragment deep into the scapula.
Results: Use of fluoroscopy and a 16 mm minimally invasive spine surgery tubular retractor allowed removal of the fragment in 30 minutes as an outpatient with good results.
Conclusion: Minimally invasive spine surgical technology could be useful for removal of shrapnel fragments from the calf, thigh, buttocks and torso.
Keywords
Minimally invasive, shrapnel, foreign body
Introduction
Delayed removal of shrapnel can be indicated for pain, infection, toxicity, migration or other delayed reactions [1-6]. Localizing small metallic fragments at surgery for remo val has presented challenges. Use of adjuncts such as ultrasound, computer-guided surgery, metal detection technology, etc. have been beneficial in localizing and removing metallic shrapnel. We report the novel use of minimally invasive spinal surgery technology for the removal of a painful shrapnel fragment from the chest wall.
Case Report
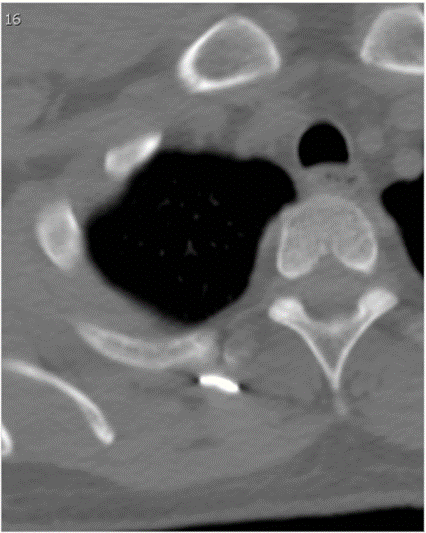
A 33-year-old soldier was injured in a rocket attack in Afghanistan. Among numerous retained shrapnel fragments, one medial to his right scapula was painful and annoying to him. He requested removal of the fragment. Neither general surgery nor plastic surgery felt comfortable removing the fragment from this location, so neurosurgical consultation was requested. The entrance wound was several centimeters lateral to the scapula. CT showed that the fragment has passed obliquely through the bone of the scapula and had come to rest against the head of the third rib (Figure 1).
Figure 1: Bone window CT showing the shrapnel fragment at the head of the right third rib.
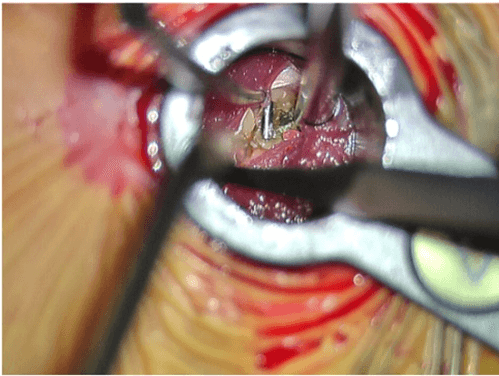
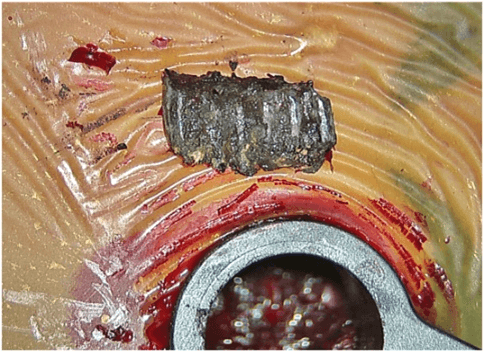
Under general anaesthesia, the patient was positioned prone on the Jackson OSI table (OSI Instruments, Ohio). The operative site was prepped and draped. An anterior-posterior fluoroscopy view was used to localize the skin incision. The intended incision was injected with bupivacaine with epinephrine. An 18 mm skin and fascial incision was made sharply. The first dilator from the METRx retractor set (Medtronic, Dublin, Ireland) was placed fluoroscopically directly onto the metallic fragment. Serial dilators were used to place a 4 cm by 16 mm final tube, which was attached to the table mount. The dilators were removed, and another AP fluoroscopy shot confirmed that the metal fragment was directly under the tube (Figure 2). The microscope was brought it. Under high magnification, the last remaining muscle fibers were separated longitudinally without cutting any muscle, revealing the fragment (Figure 3). The fragment was dissected free from surrounding scar and delivered from the tube (Figure 4). The wound was irrigated. The tube was withdrawn under the microscope and hemostasis was secured. The fascia and the dermis were closed with absorbable sutures. A single adhesive strip was placed on the wound. Operating time was less than 30 minutes. The patient was discharged to his pre-hospitalization rehabilitation setting. The preoperative pain was relieved after surgery.
Figure 2: Intra-operative AP fluoroscopy image showing the retractor tube in place and affixed to its table mounted arm with the shrapnel fragment visible directly beneath the lumen of the tube.
Figure 3: A muscle splitting approach showing the shrapnel being dissected free.
Figure 4: The fragment displayed on the drape adjacent to the tubular retractor.
Discussion
Shrapnel injuries are no longer confined to military personnel – terrorism has brought the management of shrapnel injuries to civilian facilities, whether in the acute, subacute, or chronic phase of care [7]. Localizing retained metallic fragments at deep locations or adjacent to critical neural or vascular structures can be challenging. Plain radiographs, CT scanning, fluoroscopy, computerized fluoroscopy, ultrasound, navigation systems, and metal detection have been used to aid in localizing and safely approaching metallic shrapnel [5, 8-10].
Similarly to stereotactically guided cranial and spinal surgery in use by neurosurgeons since the 1990’s, computer-guided navigation for orthopaedic trauma surgery has been used for preoperative planning, fracture reduction, intramedullary nailing, percutaneous screw placement and plating for hardware removal, and for shrapnel removal [7, 8, 11]. These systems may require a skeletally fixed antenna for detection of the patient, which can require a second incision and an accessible bone anchor close to the fragment. Computerized fluoroscopy has also been reported to be useful and can reduce the radiation exposure from CT, obviate the need for a preoperative planning stage, and shorten operating times for shrapnel removal [8].
To our knowledge, the use of minimally access spinal surgery instrumentation to approach shrapnel outside the spine has not previously been reported. We are aware of a report on the use of minimally invasive instrumentation for intracranial fragment removal [12]. Only routine fluoroscopy is necessary for this procedure. These systems allow access through a 16 mm (or larger if needed) port which allows direct vision and use of a full range of instrumentation for dissection, manipulation, and extraction of the fragment. The use of serial blunt dilators allows gentle dilation and displacement of superficial structures during the approach. Muscles traversed are minimally damaged with the use of this technique. Dissection of adjacent critical structures, hemostasis, and suturing are all possible with the appropriate instruments. Structures outside the operating retractor are protected from injury by sharp edges of the shrapnel during removal. This technique would be appropriate for use in the calf, thigh, buttocks, paraspinous regions of the lumbar, thoracic, and cervical spine, and abdominal wall. By this report, we hope to interest others in the potential applications of this technology.
Article Info
Article Type
Case ReportPublication history
Received: Mon 28, Dec 2020Accepted: Wed 13, Jan 2021
Published: Fri 29, Jan 2021
Copyright
© 2023 Donald A. Ross. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.01.16
Author Info
Corresponding Author
Donald A. RossSection of Neurological Surgery, Operative Care Division, Portland Veterans, Portland, Oregon, USA
Figures & Tables

References
- Carija R, Busic Z, Bradaric N, Bulovic B, Borzic Z et al. (2014) Surgical removal of metallic foreign body (shrapnel) from the lumbosacral spine and the treatment of chronic osteomyelitis: a case report. West Indian Med J 63: 373-375. [Crossref]
- Eylon S, Mosheiff R, Liebergall M, Wolf E, Brocke L et al. (2005) Delayed reaction to shrapnel retained in soft tissue. Injury 36: 275-281. [Crossref]
- Fireman E, Shai AB, Lerman Y, Topilsky M, Blanc PD et al. (2012) Chest wall shrapnel-induced beryllium sensitization and associated pulmonary disease. Sarcoidosis Vasc Diffuse Lung Dis 29: 147-150. [Crossref]
- Harris RM, Williams TD, Hodges NJ, Waring RH (2011) Reactive oxygen species and oxidative DNA damage mediate cytotoxicity of tungsten-nickel-cobalt alloys in vitro. Toxicol Appl Pharmacol 250: 19-28. [Crossref]
- Shankar H, Cummings C (2013) Ultrasound imaging of embedded shrapnel facilitates diagnosis and management of myofascial pain syndrome. Pain Pract 13: 405-408. [Crossref]
- Squibb KS, Leggett RW, McDiarmid MA (2005) Predication of renal concentrations of depleted uranium and radiation dose in Gulf War veterans with embedded shrapnel. Health Phys 89: 267-273. [Crossref]
- Peyser A, Khoury A, Liebergall M (2006) Shrapnel management. J Am Orthop Surg 14: S66-S70. [Crossref]
- Mosheiff R, Weil Y, Khoury A, Liebergall M (2004) The use of computerized navigation in the treatment of gunshot and shrapnel injury. Comput Aided Surg 9: 39-43. [Crossref]
- Peleg E, Harari M, Liebergall M, Mosheiff R (2009) Implementing metal detector technology and a navigation system in the removal of shrapnel. Comput Aided Surg 14: 63-68. [Crossref]
- Rogers AJ, Light ED, Smith SW (2009) 3-D ultrasound guidance of autonomous robot for localization of ferrous shrapnel. IEEE Trans Ultrason Ferroelectr Freq Control 56: 13011303. [Crossref]
- Atesok K, Schemitsch EH (2010) Computer-assisted trauma surgery. J Am Acad Orthop Surg 18: 247-258. [Crossref]
- Rymarczuk GN, Davidson L, Severson MA, Armonda RA (2015) Use of a minimally invasive retractor system for retrieval of intracranial fragments in wartime trauma. World Neurosurg 84: 1055-1061. [Crossref]
