Journals
Mediastinal Lymphangiohemangioma: A Case Report and Review of the Literature with Focus on the Ambiguous Nomenclature
A B S T R A C T
The benign mediastinal vascular lesion is an area in medicine with ambiguous terminology and poor inter- and intra-disciplinary agreement. Lymphangiohemangioma of the mediastinum is a rare, benign entity with few previous reports in the US literature. We present a case of a 55-year-old woman with shortness of breath and chest pain who was found to have an anterior mediastinal mass on imaging. The MRI features favored a mediastinal hemangioma with a differential diagnosis that included thymoma. The multi-lobulated mass was surgically removed however the left phrenic nerve was sacrificed during the resection. Histologically the lesion consisted of dilated vascular spaces of varying sizes with intra-luminal, calcified phleboliths. A variety of equivocal diagnostic terms were considered for a benign, mediastinal vascular lesion. Subsequent immunohistochemistry (IHC) showed the vessel lining consisted of both vascular and lymphatic endothelium therefore the final diagnosis made was mediastinal lymphangiohemangioma.
Introduction
Mediastinal lymphovascular lesions are rare, with few descriptions of the radiologic-pathologic characteristics in the literature. Prior case reports are heavily weighted on the radiologic characteristics and surgical management of these lesions with less emphasis on the correlation between the histology and radiology [1, 2]. One issue pathologists and radiologists frequently come across when dealing with a primary lymphovascular lesion in the mediastinum is the lack of a consistent naming system. The distinction between lymphangiohemangioma and venous hemangioma is not clear in this area and has been used interchangeably given the overlapping clinical, histologic and imaging features. The typical behavior of these lesions is indolent, with the greatest morbidity being due to the anatomic relationship of the mass to vital structures.
Case Reports
A 55-year-old woman was referred to us from an outside hospital for a mediastinal mass found on imaging during a workup for shortness of breath and chest pain. Contrast CT at the outside hospital showed a 3.8 x 2.8 cm mass in the anterior mediastinum containing calcifications with a question of a draining vessel. To better evaluate the vasculature, CT with systemic contrast bolus timing or MRI was recommended. 4 days later, MR imaging was performed at our institution without and with contrast which showed a hyperintense vascular lesion. No pulmonary or systemic arterial feeding vessels were identified; however venous connection to the left brachiocephalic vein was present. The diagnostic impression based on the constellation of MRI features was a mediastinal venous hemangioma. Follow-up CT imaging at our institution 2 months later, performed without contrast upon referring physician request, demonstrated no interval change in size or appearance.
Given the stability of the lesion and the high likelihood of lesion benignity, continued periodic CT surveillance was suggested, but the patient expressed a preference for surgical excision of the lesion as the next step in her care. Intraoperatively, the surgeon found that the lesion entrapped the left phrenic nerve which was ultimately sacrificed during the removal of the mass. The gross pathologic specimen was a semi-firm mass with three separate nodules showing surface hyperemia admixed with yellow-lobular fat. The nodules were connected by cord-like structures that contained a lumen and thickened walls on cut surface. The cut surface of the nodules showed tubular structures of varying sizes filled with serosanguineous fluid. Histologic examination revealed dilated endothelial-lined vascular spaces and lymphatic channels with scattered phleboliths, intra-lesional calcifications and adjacent atrophic thymus. IHC showed a mixture of intralesional vascular and lymphatic endothelium therefore the final diagnosis rendered was lymphangiohemangioma.
Results
On both contrast-enhanced CT (Figure 1a) and subsequently performed non-contrast CT axial thin-section reconstructions, a lobulated, anterior mediastinal, soft tissue mass [yellow arrow] containing calcifications is present. The calcifications appear blurred in Figure 1a due to respiratory motion artifact. On both contrast-enhanced CT (Figure 1b) and non-contrast CT coronal reformatted images, a thin vertical structure (white arrow) extending from the mass to the left brachiocephalic vein (LBCV) is consistent with a small-caliber venous tributary. The mass appears slightly hypointense relative to skeletal muscle and has intermediate-to-high signal intensity on axial fat-saturated, T2-weighted imaging. Multiple foci of low T2 signal scattered throughout the mass correspond to areas of calcifications visible on non-contrast CT and are compatible with intralesional calcifications and phleboliths. Fat-saturated, multiphase, T1-weighted MR and post-contrast axial imaging with intravenous gadolinium chelate contrast demonstrates diffuse serpiginous enhancement on delayed-phase imaging, consistent with intralesional vascular channels.
Figure 1: (a) Contrast-enhanced CT of a lymphangiohemangioma (Yellow arrowhead) showing intralesional calcifications and phleboliths; (b) Vascular connection to the left brachiocephalic vein is present (white arrow).
Figure 2: (a) Gross appearance of the multinodular lymphangiohemangioma; (b) A Hematoxylin-eosin section illustrating endothelial lined vascular spaces and a large central phlebolith (arrow); CD31 and D2-40 immunostains (c, d) highlighting vascular and lymphatic endothelium respectively (Hematoxylin-eosin original magnification x100 (b), Immunostains x100 (c,d).
Gross and histologic representation of the lesion is illustrated in (Figure 2). The mass is composed of dilated vascular channels with intraluminal phleboliths (Figure 2b), dystrophic calcifications and secondary osseous metaplasia. The vascular walls contained entrapped adipocytes, hemosiderin laden macrohpages and scattered aggregates of chronic inflammation. The vascular channels vary in size and thickness and are the predominant component in all three of the gross nodules. The CD31 immunostaining is less specific and highlights some lymphatic endothelium as well as vascular endothelium (Figure 2c). The D2-40 immunostaining highlights the lymphatic endothelium exclusively (Figure 2d).
Discussion
Lymphovascular lesions of the mediastinum make up a very small percentage of mediastinal tumors and can be difficult to diagnose, even with modern imaging techniques. Some authors have reported that patients with mediastinal vascular lesions present with symptoms greater than 50% of the time which can include dyspnea, cough, stridor, hoarseness, dysphagia and rarely, Horner’s syndrome [3]. It has been speculated that lymphovascular lesions of the mediastinum are embryologically derived, possibly from lymphovenous sacs and this is also supported by the fact that the majority of patients with symptomatic lesions present at a young age [13, 14]. Direct communication with the major venous system may also suggest these lesions arise during fetal development. The majority of cases occur in the anterior mediastinum with compression symptoms related to the anatomic location as previously described in the literature. Total resection is thought to be curative and recurrence likely indicates that total resection was not achieved during the initial surgery [5]. In the patients where follow-up was documented, no recurrence had been reported after total resection was achieved (Table 1).
A literature review of case studies (14 cases) with lesions classified as either mediastinal lymphangiohemangioma or mediastinal hemangioma was performed (PubMEd Medline) (Table 1). 12/14 lesions reviewed were located in the anterior mediastinum and 3/14 cases reported radiographic presence of phleboliths. All of the cases with contrast enhanced evaluation of the vascularity documented enhancing lesions with major venous system communication. 5/8 cases diagnosed as venous hemangioma documented the presence of vascular endothelium but did not report the presence or absence of lymphatic endothelium using immunohistochemical techniques. Reported cross-sectional imaging features for our patient include contrast enhancement on both CT and MR, punctate calcifications on CT, and slow blood flow in vascular channels resulting in increased signal intensity on T2-weighted MR images. This constellation of features favors the diagnosis of a mediastinal hemangioma, or lymphangiohemangioma. The presence of larger phleboliths is nearly diagnostic when associated with the preceding findings. Lymphatic-predominant tumors, such as lymphangiomas, typically show radiologic characteristics of intermediate-to-high intensity on T2 imaging along with the associated preceding findings. The protein content of the lymphangioma will typically determine the degree of signal intensity on T2-weighted MR imaging with increased protein content translating to a lower T2 signal intensity [15].
Histologically, our patient’s mass was composed of dilated vascular channels with vessel wall thickening that varied (Figure 2b). Scattered phleboliths and calcifications were present throughout the lesion and a mixture of CD31 and D2-40 positive endothelium lining the lymphovascular spaces was identified histologically. The presence or absence of lymphatic endothelium appears to have little impact on the prognosis of these lesions however; documentation of this could resolve the issue physicians face with differing nomenclature between specialties. In the rare instance that these tumors occur, perhaps an approach of combining a vascular IHC marker (CD34, CD31 or Factor VIII) with a more specific lymphatic marker (D2-40) may address the issue of identifying these lesions with a common label that is accepted by surgeons, radiologists and pathologists alike. As described in the past, intralesional vessels composed of separate lymphatic and vascular components would qualify as a lymphangiohemangioma, whereas the absence of intralesional D2-40-staining endothelium would qualify the lesion as a venous hemangioma.
Table 1: A literature review (PubMed Medline) of mediastinal lymphangiohemangioma and venous hemangioma with radiologic features, histologic classification and patient outcome.
|
Reference Number |
Location |
Radiologic Features |
Diagnosis |
Age |
Histology |
Outcome |
|
1 |
Anterior Mediastinum |
-High intensity T2 signal -Drains into Left Brachiocephalic vein -Sparse Calcifications |
Lymphangiohemangioma |
60 |
Lymph + Venous component |
No follow-up available |
|
2 |
Anterior Mediastinum |
- High intensity T2 signal -Originated from left innominate vein -Scattered Calcifications and phleboliths |
Lymphangiohemangioma |
17 |
Lymph + Venous component |
No follow-up available |
|
3 |
Anterior Mediastinum |
- CT contrast enhancement not reported - Cyst with smooth surface |
Venous Hemangioma |
23 |
Venous Component* |
No follow-up available |
|
4 |
Anterior Mediastinum |
-Dense vascular enhancement -Communicating off left innominate vein -Two prominent calcifications |
Lymphangiohemangioma |
10 |
Lymph + Venous component |
No follow-up available |
|
5 |
Anterior Mediastinum |
-CT contrast enhancement not reported -Originating from left innominate vein |
Lymphangiohemangioma |
30 |
Lymph + Venous component |
No follow-up available
|
|
5 |
Anterior Mediastinum |
- Contrast enhancing -Numerous vessels connecting to the vena cava -No calcifications |
Lymphangiohemangioma |
15 |
Lymph + Venous component |
No recurrence |
|
5 |
Anterior Mediastinum |
- Contrast enhancing -Originating from left innominate vein -A few calcifications |
Lymphangiohemangioma |
18 |
Lymph + Venous component |
Local Recurrence; initially; No recurrence after complete resection |
|
6 |
Anterior Mediastinum |
-High intensity T2 signal -Venous communication not documented |
Venous Hemangioma |
56 |
Venous component* |
No Recurrence at 15 months |
|
7 |
Posterior Mediastinum |
-homogenous well circumscribed mass -Contrast contraindicated |
Venous Hemangioma |
54 |
Venous component/D240 neg. |
No follow-up available |
|
8 |
Anterior Mediastinum |
-High intensity T2 signal -Small calcifications
|
Venous Hemangioma |
58 |
Venous component* |
No recurrence |
|
9 |
Anterior Mediastinum |
-attached to SVC and extensive vessel connection to chest wall |
Venous Hemangioma |
12 |
Cavernous Venous hemangioma* |
No follow-up available |
|
10 |
Anterior Mediastinum |
-Significant contrast enhancement -Phleboliths or calcifications were not mentioned |
Venous Hemangioma |
21 |
Venous Component* |
No follow-up available |
|
11 |
Middle Mediastinum |
-Heterogenous with hyperintense T2 vascular area and low intesnsity T2 hemorrhagic or proteinaceous area. -hemizygous or thoracic duct origin
|
Venous Hemangioma |
48 |
Venous component/D240 negative |
No recurrence at 24 months |
|
12 |
Anterior Mediastinum |
-Branches extend from pulmonary trunk to left BCV -Phleboliths and calcifications |
Cavernous Hemangioma |
25 |
Venous component |
No follow-up available |
SVC – Superior Vena Cava
*Immunohistochemical staining for a lymphatic component (D2-40) was not documented in the report
Conclusion
Our case report is the first report to correlate detailed histologic and radiologic features of a primary lymphovascular tumor of the mediastinum to improve nomenclature between radiologists, surgeons and pathologists. We expanded our case report with a literature review in order to find a trend in the imaging features and to unify the histologic classification of mediastinal lesions containing intralesional venous and/or lymphatic components. From the literature review we found that >60% of the cases diagnosed as venous hemangioma did not have IHC staining for lymphatic endothelium performed. Although clinically lymphangiohemangioma and venous hemangioma are similar and have been used interchangeably, use of the diagnosis lymphangiohemangioma is likely warranted in most cases. The diagnostic term lymphangiohemangioma better describes the histologic findings, is recognized in the literature, and is perhaps applicable to the majority of mediastinal vascular lesions reported as venous hemangioma.
Article Info
Article Type
Case ReportPublication history
Received: Mon 31, Dec 2018Accepted: Fri 08, Feb 2019
Published: Wed 27, Feb 2019
Copyright
© 2023 Candice C. Black. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.01.005
Author Info
Candice C. Black Harvinder S Jagait Jesse S Bond Julianna M Czum
Corresponding Author
Candice C. BlackDepartment of Pathology and Laboratory Medicine
Figures & Tables
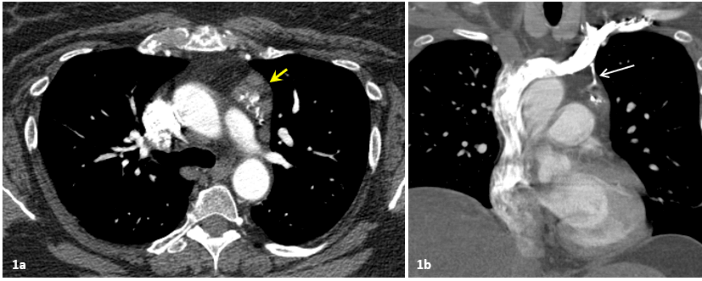
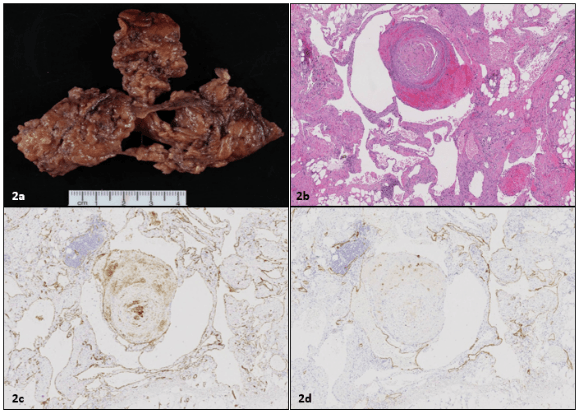
Table 1: A literature review (PubMed Medline) of mediastinal lymphangiohemangioma and venous hemangioma with radiologic features, histologic classification and patient outcome.
|
Reference Number |
Location |
Radiologic Features |
Diagnosis |
Age |
Histology |
Outcome |
|
1 |
Anterior Mediastinum |
-High intensity T2 signal -Drains into Left Brachiocephalic vein -Sparse Calcifications |
Lymphangiohemangioma |
60 |
Lymph + Venous component |
No follow-up available |
|
2 |
Anterior Mediastinum |
- High intensity T2 signal -Originated from left innominate vein -Scattered Calcifications and phleboliths |
Lymphangiohemangioma |
17 |
Lymph + Venous component |
No follow-up available |
|
3 |
Anterior Mediastinum |
- CT contrast enhancement not reported - Cyst with smooth surface |
Venous Hemangioma |
23 |
Venous Component* |
No follow-up available |
|
4 |
Anterior Mediastinum |
-Dense vascular enhancement -Communicating off left innominate vein -Two prominent calcifications |
Lymphangiohemangioma |
10 |
Lymph + Venous component |
No follow-up available |
|
5 |
Anterior Mediastinum |
-CT contrast enhancement not reported -Originating from left innominate vein |
Lymphangiohemangioma |
30 |
Lymph + Venous component |
No follow-up available
|
|
5 |
Anterior Mediastinum |
- Contrast enhancing -Numerous vessels connecting to the vena cava -No calcifications |
Lymphangiohemangioma |
15 |
Lymph + Venous component |
No recurrence |
|
5 |
Anterior Mediastinum |
- Contrast enhancing -Originating from left innominate vein -A few calcifications |
Lymphangiohemangioma |
18 |
Lymph + Venous component |
Local Recurrence; initially; No recurrence after complete resection |
|
6 |
Anterior Mediastinum |
-High intensity T2 signal -Venous communication not documented |
Venous Hemangioma |
56 |
Venous component* |
No Recurrence at 15 months |
|
7 |
Posterior Mediastinum |
-homogenous well circumscribed mass -Contrast contraindicated |
Venous Hemangioma |
54 |
Venous component/D240 neg. |
No follow-up available |
|
8 |
Anterior Mediastinum |
-High intensity T2 signal -Small calcifications
|
Venous Hemangioma |
58 |
Venous component* |
No recurrence |
|
9 |
Anterior Mediastinum |
-attached to SVC and extensive vessel connection to chest wall |
Venous Hemangioma |
12 |
Cavernous Venous hemangioma* |
No follow-up available |
|
10 |
Anterior Mediastinum |
-Significant contrast enhancement -Phleboliths or calcifications were not mentioned |
Venous Hemangioma |
21 |
Venous Component* |
No follow-up available |
|
11 |
Middle Mediastinum |
-Heterogenous with hyperintense T2 vascular area and low intesnsity T2 hemorrhagic or proteinaceous area. -hemizygous or thoracic duct origin
|
Venous Hemangioma |
48 |
Venous component/D240 negative |
No recurrence at 24 months |
|
12 |
Anterior Mediastinum |
-Branches extend from pulmonary trunk to left BCV -Phleboliths and calcifications |
Cavernous Hemangioma |
25 |
Venous component |
No follow-up available |
SVC – Superior Vena Cava
*Immunohistochemical staining for a lymphatic component (D2-40) was not documented in the report
References
- Kadota Y, Utsumi T, Kawamura T, Inoue M, Sawabata N, et al. (2011) Lymphatic and Venous Malformation or “Lymphangiohemangioma” of the Anterior Mediastinum: case report and literature review. Gen Thorac Cardiovasc Surg 59: 575-578. [Crossref]
- Xu M, Luo D, Lei W, Zhang H, Wu N, et al. (2005) Mediastinal Lymphangiohemangioma Communicating with the Left Innominate Vein. J Comput Assist Tomogr 29: 650-652. [Crossref]
- Yoshino N, Takizawa T, Terashima M, Honma K (2001) Vascular Tumor in the Mediastinum Jpn J Thorac Cardiovasc Surg 49: 181-184. [Crossref]
- Angtuaco EJC, Jimenez JF, Burrows P, Ferris E (1983) Lymphatic-Venous (Lymphangiohemangioma) of Mediastinum. J Comput Assist Tomogr 7: 895-897. [Crossref]
- Riquet M, Briere J, Pimpec-Barthes F, and Puyo P (1997) Lymphangiohemangioma of the Mediastinum. Ann Thorac Surg 64: 1476-1478. [Crossref]
- Hyrai K, Takeuchi S, Bessho R, Ohaki Y, Koizumi K, et al. (2010) Venous Hemangioma of the Anterior Mediastinum. J Nippon Med Sch 77: 115-118. [Crossref]
- Yoshino N, Okada D, Ujiie H, Akiyama H, Nishimura Y, et al. (2012) Venous Hemangioma of Posterior Mediastinum. Ann Thorac Cardiovasc Surg 18: 247-250. [Crossref]
- Nishikawa H, Osaki T, Tajima Y, Yoshimatsu T, Nagashima A, et al. (2003) Hemangioma in the Anterior Mediastinum. Jpn J Thorac Cardiovasc Surg 51: 442-444. [Crossref]
- Kalicinski ZH, Joszt W, Predzynski W, Kotarbinska-Stefanowska B (1982) Hemangioma of the Superior Caval Vein. J Pediatr Surg 17: 178-179. [Crossref]
- Zalcman G, Jancovici R, Paraf F, Vilan C, Gontier C (1990) A Rare Tumor of the Mediastinum: Benign Hemangioma. Rev Pneumol Clin 46: 31-34. [Crossref]
- Odaka M, Nakada T, Asano H, Yabe M, Kamiya N, et al. (2011) Thoracoscopic Resection of a Mediastinal Venous Hemangioma: Report of a Case. Surgery Today: 1455-1457. [Crossref]
- Dijkstra J, van Leeuwen H, Marsman JWP, Verbeeten jr. BA (1984) Cavernous Hemangioma of the Mediastinum. Fortschr. RÖntgenstr 140: 97-99.
- Sabin FR (1909) The lymphatic system in human embryos, with a consideration of the morphology of the system as a whole. American J Anatomy 9 :43-91.
- Jackson IT, Carreno R, Potparic Z, Hussain K (1993) Hemangiomas, vascular malformations, and lymphovenous malformations: classification and methods of treatment. Plast Reconstr Surg 9: 1216-1230. [Crossref]
- McAdams HP, Rosado-de-Christenson ML, Moran CA (1994) Mediastinal hemangioma: radiographic and CT features in 14 patients. Radiology 2: 399-402. [Crossref]
