Management of Squamous Cell Carcinoma in a Chronic Sacrococcygeal Pilonidal Cyst: A Case Report
A B S T R A C T
Introduction: Pilonidal disease is a chronic inflammatory process resulting from impaction of natal cleft hair into the subcutaneous tissues creating an abscess or a draining sinus over the sacrococcygeal area. Malignant transformation occurs in around 0.1%, mainly into squamous cell carcinoma (SCC) type. Wide excision with tumor-free margins remains the treatment of choice. Multiple closure techniques were settled and the best one ought to be chosen in a context malignancy and future radiological treatment.
Case Presentation: We describe the management of a case of a 69-year-old male with chronic pilonidal disease, recurrent after 25 years found on final pathology to undergo malignant transformation into SCC. Wide and aggressive excision were performed with new margins and with periosteal excision of the sacrum and coccyx. rotational myocutaneous gluteal flap was done for closure of the wound in order to ensure better satisfactory esthetic results without a delay in future treatment.
Conclusion: The progression of a chronic pilonidal disease into SCC is a rare but serious complication. The diagnosis is confirmed by biopsies. Workup for metastasis should be made before aggressive surgical excision. Oncoplastic surgeries is recommended for satisfactory results. Routine follow-up postoperatively should be considered due to high rate of recurrence by physical examination and imaging.
Keywords
Sacrococcygeal pilonidal disease, squamous cell carcinoma, rotational flap
Introduction
Pilonidal disease is a chronic inflammatory disorder that mainly affects Caucasians between 15 and 40 years of age, rarely over the age of 50 [1]. It is of male predominance and is believed to be an acquired infection of natal cleft hair follicles, that become distended and obstructed and ruptures into the subcutaneous tissues to create an abscess or a draining sinus over the sacrococcygeal area [2]. Untreated pilonidal disease may lead to cases of necrotizing wound infections, cellulitis, sacral osteomyelitis, meningitis, and malignant degeneration [3]. It was found that malignant transformation occurs in around 0.1% of patients and in 88% of these cases was of squamous cell carcinoma (SCC) as histological type. This transformation occurs in neglected primary lesions, generated by a chronic inflammatory process, thus it is most frequently seen in older people with longstanding disease [2].
Since 1900, less than 70 cases of malignancy arising in a pilonidal sinus have been published in the literature. The first case was reported by Wolff in 1900. In addition to SCC, basal cell carcinomas, adenocarcinomas and verrucous carcinomas have also been described [4]. Wide excision with tumor-free margins remains the treatment of choice. Radiotherapy and chemotherapy are of limited value. Closure of wound remains debatable. Secondary closure was associated with less rates of recurrence and primary closure was needed with more extensive disease due to loss of domain and the need of flaps from adjacent tissue. The primary closure techniques include the Z-plasty, V-Y advancement flap, rhomboid (Limberg) flap and Karydakis flap techniques [5]. We report a very rare case of SCC developing in a 69-year-old man with chronic pilonidal disease recurrent after 25 years found to be SCC on final pathology.
Case Presentation
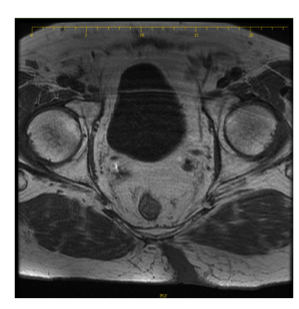
This is a case of 69-year-old male patient known to have hypertension, CAD status post angioplasty, prostate cancer status post prostatectomy and 25 sessions of radiotherapy 7 years ago. Patient has a history of recurrent sacrococcygeal pilonidal cyst to which he is admitted for re-excision. His first surgical excision of pilonidal cyst was done around 45 years prior to presentation; wound was left back then to heal by secondary intention. No reported pathology was provided back then, 2 months ago, he presented with recurrence of sacrococcygeal pilonidal cyst complicated by abscess formation. MRI done shows the sinus reaching the intergluteal region (Figure 1). Wide local Excision done, sample was sent to pathology and wound was left for secondary intention closure.
Figure 1: MRI showing the extent of the sinus reaching the gluteal muscle.
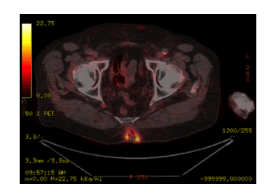
Figure 2: PET scan showing activity at the sacrococcygeal region.
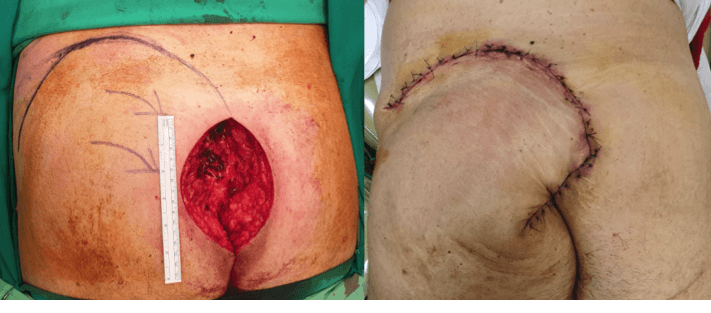
On final pathology invasive squamous cell carcinoma, regular type, and well differentiated measuring 5 cm in largest dimension with invasion of the dermis and subcutaneous adipose tissue with no lympho-vascular invasion and with positive margins was detected. This pathology is classified as Clark level V. Patient underwent PET scan (Figure 2) for better staging and it showed increased FDG uptake at the sacrococcygeal region that may represent postsurgical changes however no distant metastasis reported. Abdominopelvic CT-scan done for metastatic workout was negative (Figure 3). Decision was made to perform re-excision in order to take additional margins. Reconstruction with rotational myocutaneous gluteal flap was performed. Patient was referred for 25 sessions of radiotherapy as continuation of his treatment (Figure 4).
Figure 3: CT-scan showing absence of inguinal or presacral lymph nodes enlargement.
Figure 4: The picture on the left shows the extensive excision picture; the one on the right shows the rotational flap in place.
Discussion
Pilonidal disease arises from frictional impaction of a loose hair into the depth of a natal cleft in the sacrococcygeal area. It can manifest as an asymptomatic sinus, as an abscess or it may include cellulitis or a chronically draining sinus or fistula [1]. Malignant transformation is rare and occurs in 0.1% of the cases and is thought to be due to a long-standing or recurrent sacrococcygeal pilonidal disease [1, 2]. SCC is the most common carcinoma although basal cell carcinoma, verrucous carcinoma, and sweat gland adenocarcinoma were also been reported [1]. The mechanism of malignant transformation is believed to be like other chronic ulcerative and scarifying cutaneous disorders [1, 2]. It is thought to be due to the release of free oxygen radicals by activated inflammatory cells, that leads to genetic damage and malignant transformation [1]. In addition, the DNA repair mechanism is impaired in chronic inflammation resulting in neoplastic changes [6]. Immunosuppression and human papilloma virus infection may as well be predisposing factors inducing this transformation [1]. Therefore, the duration of the disease is one of the main factors in the malignant transformation of a pilonidal sinus [1]. It is reported that the mean duration of pilonidal disease malignant transformation is over 20 years [2, 4]. In addition, the average age at presentation of any malignant transformation is 49 years of age [2, 4].
The diagnosis of pilonidal carcinoma is done by coupling gross inspection and by biopsy. Inspection may reveal a friable ulcer with necrotic and fungating margins [1, 2]. In the present case, malignant transformation was suspected due to recurrence and chronicity, delay in healing and extensive wound edge. This transformation was confirmed by final pathology. Thus, the recommendation to send routinely all sacrococcygeal pilonidal removed specimen for histopathological evaluation to rule out malignancy. In case of high suspicion for malignant transformation, preoperative investigations should be completed. These compromise careful palpation of inguinal lymph nodes, rectal and proctosigmoidoscopic inspections in order to determine if it had spread to the rectum. Physical and endoscopic examination should be completed by CT-scan or MRI images in order to determine local extent. CT-scan and MRI may detect intra-abdominal metastases and any possible spread to the iliac or para-aortic lymph nodes [1, 4]. Lumbosacral and coccyx spine x-rays should also be performed to rule out osteomyelitis or bone invasion by the tumor [2, 4]. In our case, malignancy was confirmed by biopsy; MRI and PET scan were negative for metastasis when done prior to the re-excision.
In case of sacrococcygeal pilonidal sinus, the treatment of choice remains surgical excision which compromise all sinus tracts. Wider surgical excision using oncologic techniques of en-bloc resection is recommended in case of malignant transformation of the sacrococcygeal cyst or sinus. It includes presacral fascia, gluteal muscle with good margins of skin and subcutaneous tissue. We did a periosteal excision of sacrum and coccyx in order to exclude bone involvement. It is important to note that no proven benefit was seen with prophylactic inguinal node dissection [1].
Closure after sacrococcygeal pilonidal excision has long been debatable whether by primary or secondary intention. While secondary intention showed less recurrence rates, primary intention displayed more appealing results and was more beneficial in extensive wounds. Primary closure includes midline or off-midline techniques which further includes skin grafts or local flaps. Z-plasty, V-Y advancement flap, rhomboid (Limberg) flap and Karydakis flap represent the most used techniques [5, 7]. In the present case, it was a challenge to perform the most adequate reconstruction technique knowing that the wound was very extensive and that it will be followed by radiotherapy that may delay wound healing. Gluteal musculocutaneous flap was the technique chosen which allows good blood supply to our flap with the inferior gluteal artery, along with adequate filling of the defect with an appropriate thickness taken, and closure of the wound for continuation of treatment [8]. Oncoplastic surgery has become more involved in surgeries that require excision of a malignancy along with a reconstruction of the wound that meets the requirements of a better wound healing and postoperative care and medical treatment.
When tumors are adherent to the sacrum or has perforated sacral fascia curative intent during excision may become unachievable due to inability to achieve negative margins. In these cases, recurrence of malignancy may reach 50% and may appear 9 to 16 months after the surgery, thus requiring closer follow-ups [9]. Adjuvant radiotherapy with good surgical margin can reduce local recurrence to 30%; however, adjuvant chemotherapy did not show similar beneficence [6]. A pilonidal disease complicated by SCC has a 5-year survival rate of 55-61%. No relationship was reported between the degree of tumor differentiation and survival [1]. Regular check-ups postoperatively every 3 months during the first 2 years, every 6 months for the next 3 years, and yearly afterwards should be done due to the high recurrence rate [8]. It comprises examination of the sacrococcygeal and inguinal area, and abdominal CT-scan in order to exclude local recurrence or distant metastasis [2].
Conclusion
The progression of a chronic pilonidal disease into SCC is a rare but serious complication [1]. The diagnosis is usually confirmed by histological examination of the specimen. All specimens of pilonidal disease should be sent routinely for histopathological evaluation and when malignant transformation is confirmed endoscopic investigations, lymph node inspection and imaging are required before aggressive re-excision [1, 2]. It may be followed by adjuvant radiotherapy [1]. With the advancement of plastic surgery, oncological surgeries for such entities result in more esthetic outcome. Routine follow-up postoperatively should be considered due to high rate of recurrence by physical examination and imaging [1, 2, 4].
Acknowledgements
We acknowledge the contribution the department of general surgery, plastic surgery and radiology departments at the Saint George Hospital University Hospital.
Competing Interests
None.
Consent for Publication
An informed consent was obtained from the patient to disclose medical information and imaging.
Article Info
Article Type
Case ReportPublication history
Received: Tue 26, May 2020Accepted: Tue 09, Jun 2020
Published: Fri 19, Jun 2020
Copyright
© 2023 Ziad El Rassi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.18
Author Info
Charbel Aoun Hani Maalouf Saleem Abdel Backi Toufic Saber William Watfa Ziad El Rassi
Corresponding Author
Ziad El RassiProfessor of General Surgery, Head of General Surgery Department, Saint Georges Hospital University Medical Center, University of Balamand, Beirut, Lebanon
Figures & Tables

References
- Michalopoulos N, Sapalidis K, Laskou S, Triantafyllou E, Raptou G et al. (2017) Squamous cell carcinoma arising from chronic sacrococcygeal pilonidal disease: a case report. World J Surg Oncol 15: 65. [Crossref]
- Parpoudi SN, Kyziridis DS, Patridas DC, Makrantonakis AN, Iosifidis P et al. (2015) Is histological examination necessary when excising a pilonidal cyst? Am J Case Rep 16: 164-168. [Crossref]
- Eryılmaz R, Bilecik T, Okan I, Ozkan OV, Coşkun A et al. (2014) Recurrent squamous cell carcinoma arising in a neglected pilonidal sinus: report of a case and literature review. Int J Clin Exp Med 7: 446-450. [Crossref]
- Taylor SA, Halligan S, Bartram CI (2003) Pilonidal sinus disease: MR imaging distinction from fistula in ano. Radiology 226: 662-667. [Crossref]
- de Bree E, Zoetmulder FA, Christodoulakis M, Aleman BM, Tsiftsis DD (2001) Treatment of malignancy arising in pilonidal disease. Ann Surg Oncol 8: 60-64. [Crossref]
- Almeida JC (2012) A curative cryosurgical technique for advanced cancer of sacrococcygeal pilonidal sinuses. J Surg Oncol 106: 504-508. [Crossref]
- Alvandipour M, Zamani MS, Ghorbani M, Charati JY, Karami MY (2019) Comparison of Limberg Flap and Karydakis Flap Surgery for the Treatment of Patients With Pilonidal Sinus Disease: A Single-Blinded Parallel Randomized Study. Ann Coloproctol 35: 313-318. [Crossref]
- Erkent M, Şahiner İT, Bala M, Kendirci M, Yıldırım MB et al. (2018) Comparison of Primary Midline Closure, Limberg Flap, and Karydakis Flap Techniques in Pilonidal Sinus Surgery. Med Sci Monit 24: 8959-8963. [Crossref]
- Kovacevic P, Visnjic M, Vukadinovic M (2007) Carcinoma arising in pilonidal disease – Report of two cases. Facta Univ 14: 133-137.
