Management of Para-Aortic Lymph Node Metastasis in Rectal Squamous Carcinoma
A B S T R A C T
Background: Squamous cell carcinoma (SCC) of the rectum is a rare malignancy, and retroperitoneal nodal metastasis (RNM) represent 1-2% of colorectal cancer metastasis (CRC), and radical retroperitoneal lymphadenectomy (RRL) in this setting remains controversial. However, there are no reports in the literature on how to treat SCC retroperitoneal lymph node metastasis.
Case Presentation: The patient was a 47-years-old woman with SCC of the rectum. Concomitant chemoradiotherapy (CRT) followed by surgery was planned. After 8 weeks, CT of the abdomen for restaging showed a 6 cm para-aortic mass involving and obstructing the medium third of the left ureter. The patient was submitted to abdominoperineal rectal resection with left nephrectomy and en-bloc resection of para-aortic tumor (nodal bulking).
Conclusion: After a thorough review of the literature regarding RNM for rectal SCC, we found no mention of how to treat RNM for rectal SCC. The purpose of this paper is to report a very rare case of RNM for rectal SCC and to discuss the surgical approach. Surgery seems to be the best option for local control and improvement in overall survival (OS).
Keywords
Squamous carcinoma, rectal neoplasm, para-aortic, metastasis
Background
Rectal squamous cell carcinoma (SCC) is a rare malignancy of the gastrointestinal (GI) tract without a clarified pathogenesis mechanism and a rather aggressive clinical behaviour [1]. The incidence of this malignancy has been reported to be 0.25 to 1 per 1000 colorectal carcinomas [2]. The SCC of the rectum mainly affects individuals between the age of 39 and 93 years and is more frequently found in women [3].
The SCC tumors are associated with a worse overall 5- years survival than adenocarcinomas. Interestingly, squamous cell carcinomas presenting with more advanced stage disease showed a similar survival rate to adenocarcinomas of the same stage [4]. Retroperitoneal nodal metastasis (RNM) represent 1-2% of metastasis from colorectal cancer (CRC) and radical retroperitoneal lymphadenectomy (RRL) in this setting remains controversial; however, there is no mention in the literature on how to treat SCC retroperitoneal lymph node metastasis [5]. In this study, we report a 47-year-old woman with rectal metastatic SCC to the para-aortic lymph node, discussing the efficacy of aggressive surgery on survival and prognosis.
Case Report
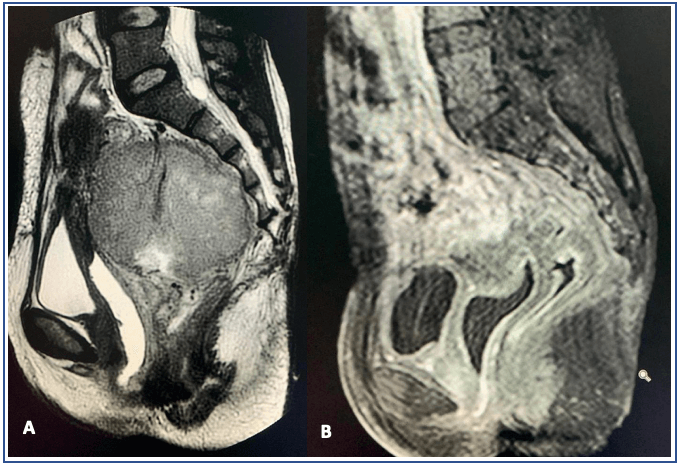
Our patient was a 47-year-old woman admitted to our Oncological Surgical department presenting with rectal pain and frequent bleeding. No history of any co-morbid illness or substance abuse was present. General physical examination was normal, except for a mild degree of pallor. The colonoscopy revealed an obstructive lesion in the medium rectum, at 7 cm from the anal margin. Biopsies were performed, and a histopathological examination (HPE) revealed moderately differentiated SCC. A magnetic resonance imaging of the pelvis and computed tomography (CT) of the chest and abdomen was performed as per institutional protocol, which was suggestive of lesion localized to rectum (Figure 1A). No evidence of nodal or distant disease was found. PET-CT was not available in our hospital.
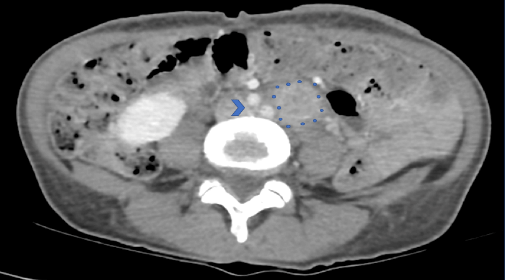
The case was discussed in the institutional tumor board and concomitant chemoradiotherapy (CRT) followed by surgery was planned. External beam radiotherapy with concomitant fluorouracil-based chemotherapy was delivered. The patient completed the treatment without any untoward event. After 8 weeks, CT of the abdomen for restaging showed a 6 cm para-aortic mass (Figure 2) involving and obstructing the medium third of the left ureter, with no excretion of venous contrast by the left kidney and thickening of the rectum (Figure 1B). The patient persisted with rectal pain.
Figure 1: Pelvic MRI before neoadjuvant CRT A) showing infiltrative rectal tumor, and after B) showing thickness in rectum.
Figure 2: Contrasted CT showing para-aortic lymph node bulking (limited by blue dots), just below aortic bifurcation (blue arrow), visible after neoadjuvant CRT.
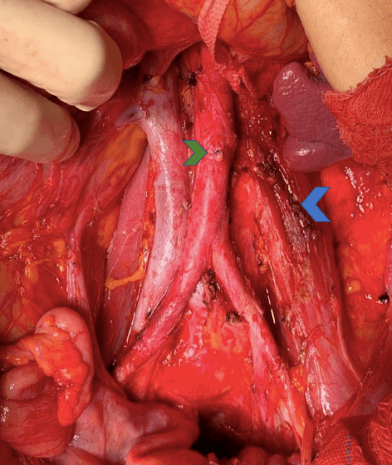
Figure 3: Para-aortic lymphadenectomy. AMI stump (green arrow); left psoas with margin of resection of lymph node bulking.
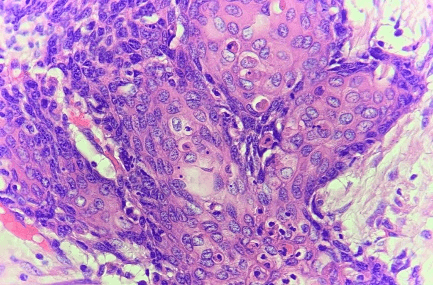
The patient was submitted 14 weeks after neoadjuvant CRT to abdominoperineal rectal resection with left nephrectomy (renal exclusion), en-bloc resection of the para-aortic tumor and retroperitoneal lymphadenectomy (Figure 3). Histopathological examination showed a complete pathological response in the rectum, and squamous carcinoma metastasis in the para-aortic mass (Figure 4), with R0 resection. The patient had no postoperative morbidity, with complete relief of symptoms, and was discharged from hospital 6 days after surgery.
Figure 4: Histopathological of the para-aortic lymph node with islands of squamous epithelium with atypical cells and dyskeratosis; 40x augmentation; hematoxylin and eosin.
Discussion
SCC is one of the rarest forms of rectal cancer. Pure SCC is a very rare histological diagnosis and clinical occurrence [6]. Furthermore, many supposed rectal SCC may be an extension of anal or gynecological carcinoma. For that reason, Williams et al. established guidelines before a definitive diagnosis of SCC can be made [7]. These criteria include:
Exclusion of primary SCC from distant sources;
Exclusion of a squamous lined fistula from bowel tumor;
Tumor must originate from the rectum and not be an extension of anal SCC;
Confirmation of SCC by histology.
To fulfill the above criteria, we decided to proceed with magnetic resonance, which confirmed its origin from the rectal wall with enlarged perirectal lymph node and no local spread to adjacent pelvic organs. Due to its rarity, the natural history and progression of SCC are not well established.
The treatment of rectal SCC has traditionally involved surgery, in some cases preceded or followed by adjuvant radiotherapy or chemotherapy. The definite therapy is surgical resection of the affected rectum, either by low anterior resection or by abdominoperineal resection, depending on the location of the tumor [8]. However, in the last decade, there has been increasing interest in the response of rectal SCC to definitive chemoradiotherapy, with very encouraging results [9]. Clinical examination is not a reliable predictor of tumor response after treatment. Our decision on surgical rescue was based on the persistence of symptoms and significant rectal thickening 12 weeks after the end of CRT.
Several studies for colorectal cancer have suggested that surgery for retroperitoneal nodal metastasis is the only potentially curative treatment and can achieve long-term overall survival in selected patients with acceptable postoperative morbidity. Median OS in operated patients was 34-46 months, compared with 3-33 months in those who did not have surgery, and five-year OS was 15-53% versus 0-12% respectively [10, 11]. Because of that, extrapolating these results to rectal SCC, we chose to perform surgical resection for retroperitoneal metastasis. Furthermore, the efficiency of systemic treatment for squamous rectal tumor metastasis has not been established to improve outcomes. There is no literature regarding maintenance chemotherapy for persistent metastatic disease [12].
Conclusion
In summary, we described a very rare case of RNM for SCC rectal cancer, and the surgical approach seems to be the best option for local control and improvement in OS. Further research, including prospective trials and large observational studies, is needed to better define the role of surgery in the management of these patients.
Acknowledgements
We would like to thank the Surgical Oncology and the Pathology departments of Hospital de Câncer de Pernambuco, as well as the Surgical Oncology residents for assisting in the patient’s operation and postoperative care.
Author Contributions
Cecília Araújo Carneiro Lima and Mário Rino Martins drafted the manuscript, Juliana Karine Ferreira Santos Lessa provided the original pictures and Rogério Luiz dos Santos and Luciana Mata da Silva reviewed the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of Data and Materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Ethics Approval and Consent to Participate
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
Competing Interests
None.
Abbreviations
SCC: Squamous Cell Carcinoma
RNM: Retroperitoneal Nodal Metastasis
CRC: Colorectal Cancer
RRL: Radical Retroperitoneal Lymphadenectomy
GI: Gastrointestinal
HPE: Histopathological Examination
CT: Computed Tomography
CRT: Chemo-Radiotherapy
Article Info
Article Type
Case ReportPublication history
Received: Mon 01, Jun 2020Accepted: Fri 12, Jun 2020
Published: Fri 19, Jun 2020
Copyright
© 2023 Mário Rino Martins. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.03.06
Author Info
Cecília Araújo Carneiro Lima Juliana Karine Ferreira Santos Lessa Luciana Mata da Silva Mário Rino Martins Rogério Luiz dos Santos
Corresponding Author
Mário Rino MartinsDepartment of Surgical Oncology, Hospital de Câncer de Pernambuco, Recife-PE, Brazil
Figures & Tables
References
- Glen R Guerra, Cherng H Kong, Satish K Warrier, Andrew C Lynch, Alexander G Heriot et al. (2016) Primary squamous cell carcinoma of the rectum: An update and implications for treatment. World J Gastrointest Surg 8: 252-265. [Crossref]
- Zaied Sonia, Daldoul Amira, Bhiri Hanene, Ammar Nouha, Khechine Wiem et al. (2017) Complete Pathologic Response After Chemoradiotherapy in a Patient With Rectal Squamous Cell Carcinoma: A Case Report. Cancer Biol Med 14: 414-417. [Crossref]
- Daryl Ramai, Kinesh Changela, Jonathan Lai, Ghulamullah Shahzad, Madhavi Reddy (2017) Interval Squamous Cell Carcinoma of the Rectum. Case Rep Gastroenterol 11: 396-401. [Crossref]
- Hakjung Kang, Jessica B O'Connell, Michael J Leonardi, Melinda A Maggard, Marcia L McGory et al. (2007) Rare tumors of the colon and rectum: a national review. Int J Colorectal Dis 22: 183-189. [Crossref]
- J Gagnière, A Dupré, S Chabaud, P Peyrat, P Meeus et al. (2015) Retroperitoneal nodal metastases from colorectal cancer: Curable metastases with radical retroperitoneal lymphadenectomy in selected patients. Eur J Surg Oncol 41: 731-737. [Crossref]
- F A Frizelle, K S Hobday, K P Batts, H Nelson (2001) Adenosquamous and squamous carcinoma of the colon and upper rectum: a clinical and histopathologic study. Dis Colon Rectum 44: 341-346. [Crossref]
- G T Williams, A J Blackshaw, B C Morson (1979) Squamous carcinoma of the colorectum and its genesis. J Pathol 129: 139-147. [Crossref]
- Theodosios K Theodosopoulos, Athanasios D Marinis, Nikolaos A Dafnios, John G Vassiliou, Lazaros D Samanides et al. (2006) Aggressive treatment of metastatic squamous cell carcinoma of the rectum to the liver: a case report and a brief review of the literature. World J Surg Oncol 4: 49. [Crossref]
- Deepak Sundriyal, Nikhil Shirsi, Sumedha Kotwal, Ramesh Dawar (2015) Squamous Cell Carcinoma of Rectum: How to Treat? Indian J Surg Oncol 6: 300-302. [Crossref]
- Byung Soh Min, Nam Kyu Kim, Seung Kook Sohn, Chang Hwan Cho, Kang Young Lee et al. (2008) Isolated paraaortic lymph-node recurrence after the curative resection of colorectal carcinoma. J Surg Oncol 97: 136-140. [Crossref]
- David Shibata, Philip B Paty, Jose G Guillem, W Douglas Wong, Alfred M Cohen (2002) Surgical management of isolated retroperitoneal recurrences of colorectal carcinoma. Dis Colon Rectum 45: 795-801. [Crossref]
- Farshad Bozorgnia, Hossein Akhondi, Ann Wierman (2018) Squamous Cell Carcinoma of the Rectum. SL Clin Med Oncol 2: 113.
