Journals
Luc’s Abscess: First Reported Case with Coexisting Intracranial Abscess and/or Venous Sinus Thrombosis
A B S T R A C T
Objective: To present a novel case of Luc’s Abscess with coexisting intracranial abscess and venous sinus thrombosis.
Case Presentation: A 4-year-old male had fever for two weeks, left-sided otalgia and otorrhea for 1 week and then suddenly developed left temporal soft tissue swelling and papilledema. Computerized tomography scan revealed a 3.5 x 2.3 x 1.2cm subperiosteal temporal space (Luc’s) Abscess, a 4.6 x 2.7 x 2.5 cm temporal lobe abscess, and transverse plus sigmoid sinus thrombosis. The patient was successfully treated with surgical drainage, long-term intravenous antibiotics, and anti-coagulation.
Conclusion: To our knowledge, this is the first documented case of Luc’s abscess with a coexisting intracranial abscess and/or venous sinus thrombosis. Although Luc’s abscess is a rare and usually relatively benign complication of acute otitis media, early diagnosis and treatment remain essential in preventing potentially life-threatening disease progression.
K E Y W O R D S
Otitis Media, temporal bone, abscess, pediatrics
Introduction
Acute Otitis Media (AOM) has a global incidence rate of 10.85% and causes 21,000 worldwide deaths annually [1]. It is the most frequent indication for antibiotic therapy in children [2]. According to the most recent pediatric AOM guidelines, cases of uncomplicated unilateral AOM in otherwise healthy children over the age of 6 months (and bilateral over 24 months) do not actually require antibiotics as the disease course is usually self-limiting [2]. While it is imperative to be judicious regarding the prescription of antibiotics for most cases of AOM, close clinical observation with prompt treatment as needed remains essential to prevent the development of complications.
One such complication was first described in the early 1900’s by Dr. Henri Luc, who reported on the management of a sub-periosteal temporal abscess in a young patient with AOM without suppuration of the mastoid air cells. This extra-cranial complication of acute otitis media (AOM) later became known as a Luc’s abscess (LA) [3]. Dr. Luc hypothesized that bacteria travels under the mucous membrane of the epitympanum and then traverses the notch of Rivinus to arrive at the sub-periosteal space of the bony external ear canal causing suppuration in the sub-periosteal temporal space [3]. While our surgical forefathers described this entity as relatively benign, we present the first case of Luc’s Abscess with associated intracranial abscess formation with a focus on the patient’s medical and surgical management as well as a review of the contemporary medical literature.
Materials and Methods
After parental consent was obtained, the patient’s medical charts and imaging were retrospectively reviewed. A literature review was then conducted on MEDLINE and PubMed using the keywords: “Acute otitis media”, “AOM”, “Luc’s Abscess”, “temporal space abscess”, “Intracranial abscess”, and “sinus thrombosis”.
Case Report
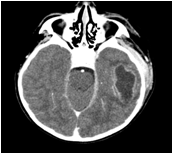
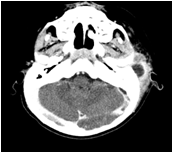
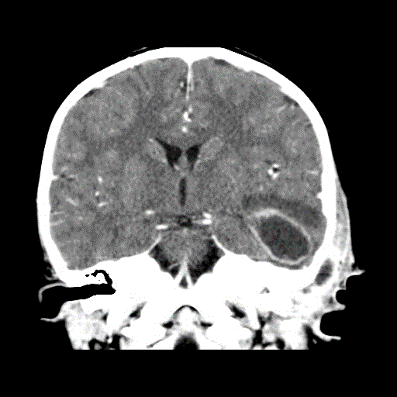
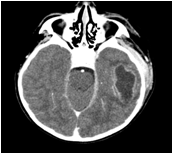
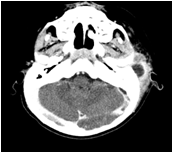
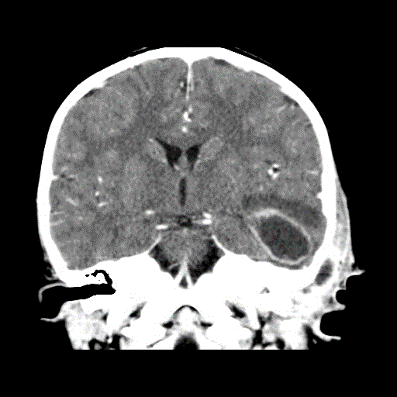
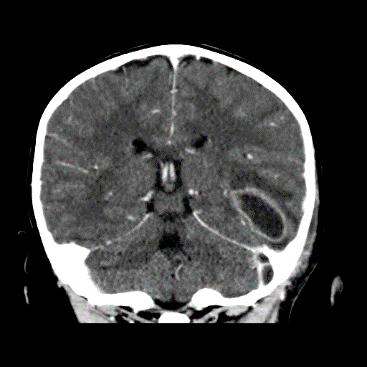
A previously healthy 4-year-old male presented with a 2-week history of fever and malaise followed by 1 week of left-sided otalgia and otorrhea. He was initially treated with antibiotic otic drops in the community but then developed left-sided headaches, peri-auricular swelling, and erythema and was brought to the hospital. Computerized Tomography (CT) scan revealed a 3.5 x 2.3 cm x 1.2cm left sub-periosteal temporal (Luc’s) abscess, an adjacent 4.6 x 2.7 x 2.5 cm temporal lobe abscess, and opacification of the left middle ear and mastoid air cells, without coalescence. Additionally, there was ipsilateral transverse and sigmoid sinus thrombosis extending to the jugular bulb (figure 1-5). There was no family history of hypercoagulability.
The patient was started on intravenous (IV) Ceftazidime and Gentamicin, was air-transferred to our center. He underwent an ultrasound-guided drainage of the intracranial collection via a small burr hole by the Neurosurgery team. They noticed pus emanating from the external auditory canal (EAC) with gentle pressure on the superior preauricular soft tissues. Thirteen cc of pus was obtained and sent for culture and sensitivity. Micro-otoscopy revealed a dehiscence in the EAC, which was used to drain 10 cc of pus by applying pressure over the temporalis muscle. In addition, a tympanic membrane perforation was identified, and further purulence was suctioned, followed by instillation of ciprofloxacin/dexamethasone drops. We elected to allow drainage through this perforation rather than place a tube.

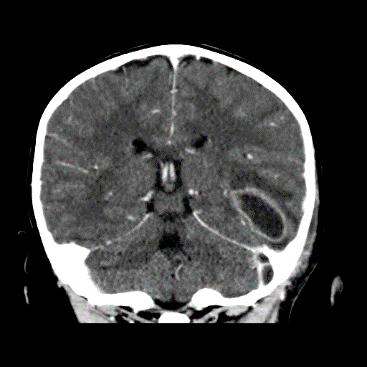

The patient tolerated the procedure well and was afebrile, hemodynamically, and neurologically stable on Ciprofloxicin / Dexamethasone otic drops, IV Vancomycin, Cefotaxime, and metronidazole. Repeat contrast-enhanced CT scan on post-operative day 1 revealed sufficient drainage of both abscesses, but persistent venous sinus thrombosis and the patient was started on subcutaneous enoxaparin anticoagulation. Streptococcus pyogenes was detected via direct 16S ribosomal gene sequencing of the intracranial pus and antibiotic coverage was narrowed to IV Cefotaxime and metronidazole. The patient was transferred back to his regional hospital on post-operative day 7 where he completed a total of 7 weeks of intravenous antibiotic and 14 weeks of anticoagulation.
At 14 weeks follow-up the patient was clinically well with a normal otologic and neurological examination. Magnetic Resonance Imaging (MRI) revealed resolution of both abscesses and significant improvement in the dural venous sinus thromboses. A left temporal lobe scar was evident (figure. 6).
Discussion
This patient presented with several complications of AOM: an intracranial abscess, sigmoid and transverse sinus thrombosis, and a large Luc’s abscess. His otologic disease was successfully treated with trans-canal incision and drainage (I+D), systemic antibiotics, and anticoagulation without pressure equalization tube or cortical mastoidectomy. It is important to ask how this management compares to protocols used at other centers. This is a difficult question given the rarity of this condition. Historically, in 1900, Dr. Luc managed a 9-year-old girl with a sub-periosteal temporal abscess by local drainage, cortical mastoidectomy, and three weeks of dressing changes [3]. The child made a full recovery, and since no mastoid pathology had been found intra-operatively, Dr. Luc deemed the mastoidectomy to have been unnecessary [3]. He later reported the successful treatment of an adult male patient with only I+D of the sub-periosteal temporal space abscess [3].
Review of the contemporary literature revealed only 6 individual cases of Luc’s abscess managed over the past 30 years. In 1997, Knappe and Gregor treated a 15-year old patient with cholesteatoma and LA with trans-canal incision and drainage, cortical mastoidectomy (for excision of cholesteatoma), Penrose drain, and 5 days of IV antibiotics [4]. Upon mastoidectomy, there was evidence of cholesteatoma but no suppuration of the air cells [4]. In 2010, Weiss and colleagues reported on two 5-year-old patients with LA [5]. Both underwent external I+D of the abscess, myringotomy and tube (M+T) placement, as well as IV antibiotic therapy. One patient had a CT scan demonstrating a well-aerated mastoid while the other had a cortical mastoidectomy, which was later deemed to have been unnecessary (Weiss et al. 2010) [5]. In 2012, Santhi and collaborators successfully managed a 5-year-old boy with LA secondary to congenital cholesteatoma with post-auricular I+D and modified radical mastoidectomy [6]. In 2014, a group in the UK managed a 4-year-old patient who presented with LA as well as CT-confirmed acute coalescent mastoiditis with I+D, M+T, Penrose drainage for 48 hours, and 4 weeks of topical and systemic antibiotics [7]. They argued that LA with concurrent acute mastoiditis is a different clinical entity requiring more aggressive surgery and that a CT scan is essential in delineating this pathology [7]. Finally, in 2017 an interesting case of LA with septic arthritis of the temporomandibular joint (TMJ) was effectively treated with M+T, external I+D of the temporal abscess, TMJ arthrotomy and lavage, and a 6-week course of IV antibiotics [8]. Of note, no mastoidectomy was performed and the patient received the prolonged course of antibiotics to cover for septic arthritis and possible osteomyelitis [8].
Table 1: Summary of cases of Luc’s abscess managed over the last 30 years
|
Age |
Sex |
Organism |
Cholesteatoma |
Dural venous sinus thrombosis |
Treatment |
|
|
1 |
15 |
M |
S. Pyogenes |
Yes |
No |
I+D, mastoidectomy, IV antibiotics |
|
2 |
5 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, IV antibiotics |
|
3 |
5 |
M |
F. Necrophorum |
No |
No |
I+D, M+T, mastoidectomy, IV antibiotics |
|
4 |
5 |
M |
n/a |
Yes |
No |
I+D, mastoidectomy |
|
5 |
4 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, mastoidectomy, IV antibiotics |
|
6 |
5 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, arthrotomy and lavage, prolonged IV antibiotics |
* I+D: incision and drainage, M+T: myringotomy and tube, IV: intravenous
When examining these 6 cases, certain trends are evident (see table 1). The majority of patients are male, aged 4-5, and infected with S. Pyogenes. The present case is also a 5-year-old male whose ribosomal gene sequencing revealed S. pyogenes. This bacterium is actually uncommon in AOM; however, reports have associated it with acute mastoiditis and increased local aggressivity, which appears to have been corroborated by the Luc’s abscess literature and may account for our patient’s complicated course [9]. Management in the literature varied from addressing the sub-periosteal temporal abscess alone, to myringotomy, to cortical mastoidectomy. In the majority of cases, however, cortical mastoidectomy was reserved for cholesteatoma excision and there was general consensus that it was unnecessary for isolated sub-periosteal temporal abscesses.
While this is the first reported case in which a LA was associated with an intracranial abscess, sigmoid vein thrombosis is a common suppurative complication of AOM [10]. To our knowledge, there are no cases in the literature reporting Luc’s Abscess in concurrence with a venous sinus thrombosis. Regarding the management of venous sinus thrombosis, a previous report has shown that tympanostomy tube insertion – or myringotomy alone – is usually sufficient surgical therapy (in addition to IV antibiotics and consideration of anticoagulation therapy) [11]. In this case, a cortical mastoidectomy, or perhaps even more extensive surgery, would have been considered had there been evidence of coalescence, cholesteatoma and/or an abscess adjacent to the venous sinus thrombosis [12].
A final point that must be stressed, especially as the medical community becomes more reserved in the prescription of antibiotic therapy, is the notion of appropriate follow-up and escalation of treatment as needed. This patient’s initial treatment with optic drops alone was insufficient as the standard of care for severe AOM with tympanic membrane perforation is systemic antibiotics in addition to topical therapy [2]. This patient’s initial treatment was insufficient as the standard of care for severe AOM with tympanic membrane perforation is systemic antibiotics in addition to topical therapy [2]. If the patient had presented before his intracranial abscess had reached 2.5 cm maximum diameter, his condition may have been treatable with IV antibiotics guided by culture results obtained from stereotactic aspiration [13]. In cases of suspected severe AOM in which the reliability of follow-up is uncertain, hospitalization should also be considered.
Conclusion
To our knowledge, this is the first reported case of Luc’s abscess with a coexisting intracranial abscess and/or venous sinus thrombosis. Early diagnosis and treatment remain essential in preventing life-threatening complications of AOM, such as those presented in the current case. Although most cases of AOM in children 6 months or older resolve without antibiotics, proper diagnosis, treatment, and especially close clinical observation and follow-up of all cases of suspected severe or complicated cases of AOM is vital.
Acknowledgements
To our knowledge, this is the first reported case of Luc’s abscess with a coexisting intracranial abscess and/or venous sinus thrombosis. Early diagnosis and treatment remain essential in preventing life-threatening complications of AOM, such as those presented in the current case. Although most cases of AOM in children 6 months or older resolve without antibiotics, proper diagnosis, treatment, and especially close clinical observation and follow-up of all cases of suspected severe or complicated cases of AOM is vital.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Article Info
Article Type
Case ReportArticle History
Received 25 August, 2018Accepted 12 September, 2018
Published 20 September 2018
Copyright
© 2018 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.03.005
Author Info
Corresponding author
Ardalan AkbariDivision of Otolaryngology – Head & Neck Surgery, BC Children's Hospital, 603 Kenwood Road, West Vancouver, British Columbia, Canada, V7S 1S7;
Figures & Tables
Table 1: Summary of cases of Luc’s abscess managed over the last 30 years
|
Age |
Sex |
Organism |
Cholesteatoma |
Dural venous sinus thrombosis |
Treatment |
|
|
1 |
15 |
M |
S. Pyogenes |
Yes |
No |
I+D, mastoidectomy, IV antibiotics |
|
2 |
5 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, IV antibiotics |
|
3 |
5 |
M |
F. Necrophorum |
No |
No |
I+D, M+T, mastoidectomy, IV antibiotics |
|
4 |
5 |
M |
n/a |
Yes |
No |
I+D, mastoidectomy |
|
5 |
4 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, mastoidectomy, IV antibiotics |
|
6 |
5 |
M |
S. Pyogenes |
No |
No |
I+D, M+T, arthrotomy and lavage, prolonged IV antibiotics |
* I+D: incision and drainage, M+T: myringotomy and tube, IV: intravenous


References
1. Monasta L, Ronfani L, Marchetti F, Montico M, Brumatti L, et al. (2012) Burden of Disease Caused by Otitis Media: Systematic Review and Global Estimates. PLoS One 7: e36226. [Crossref]
2. Lieberthal A, Carroll A, Chonmaitree T, Ganiats T, Hoberman A, et al. (2013) The Diagnosis and Management of Acute Otitis Media. Pediatrics 131: E964-E999. [Crossref]
3. Luc H. (1913) The Sub-Periosteal Temporal Abscess of Otic Origin Without Intra-Osseous Suppuration*. The Laryngoscope 23: 999-1003.
4. Knappe MV, Gregor RT (1997) Luc's abscess - a rare complication of middle-ear infection. J Laryngol Otol 111: 461-464. [Crossref]
5. Weiss I, Marom T, Goldfarb A, Roth Y (2010) Luc's Abscess: The Return of an Old Fellow. Otol Neurootol 31:776-779. [Crossref]
6. Santhi K, Tang IP, Nordin A, Prepageran N (2012) Congenital cholesteatoma presenting with Luc's abscess. J Surg Case Rep 2012: rjs026-rjs026. [Crossref]
7. Scrafton DK, Qureishi A, Nogueria C, Mortimore S (2014) Luc’s abscess as an unlucky complication of mastoiditis. Ann R Coll Surg Engl 96: e28-e30. [Crossref]
8. Tsai C, Deramo J, Shen X, Vandiver K, Mittal V (2017) Lucʼs Abscess and Temporomandibular Joint Septic Arthritis: Two Rare Sequelae of Acute Otitis Media. Pediatr Emerg Care 1-3. [Crossref]
9. Segal N, Givon-Lavi N, Leibovitz E, Yagupsky P, Leiberman A, et al. (2005) Acute Otitis Media Caused by Streptococcus pyogenes in Children. Clin Infect Dis 41: 35-41. [Crossref]
10. Thorne MC, Chewaproug L, Elden LM (2009) Suppurative complications of acute otitis media: changes in frequency over time. Arch Otolaryngol Head Neck Surg 135: 638-41. [Crossref]
11. Wong L, Kozak FK, Poskitt K, Ludemann JP, Harriman M (2005) Pediatric Lateral Sinus Thrombosis: retrospective case series and literature review. J Otolaryngol 34: 79-85. [Crossref]
12. Ludemann J, Poskitt K, Singhal A (2010) Intracranial Hypertension Secondary to Sigmoid Sinus Compression by a Group A Streptococcal Epidural Abscess. J Laryngol Otol 124: 93-95. [Crossref]
13. Frazier J, Ahn E, Jallo G (2008) Management of brain abscesses in children. Neurosurg Focus 24: E8. [Crossref]
