Journals
Ipsilateral proximal and distal clavicle fractures combined with coracoid base fracture: A case report
A B S T R A C T
Ipsilateral fractures of the proximal and distal clavicle are quite rare. Double clavicle fractures are extremely rare. We report a case of ipsilateral fractures of the proximal and distal clavicle combined with a coracoid base fracture, a combination which has not been reported before. These injuries disrupt the superior shoulder suspensory complex (SSSC) by breaking the coracoid base and distal clavicle. This would normally be a surgical case, but all fractures were non-displaced. We discussed the treatment options with the patient, and he chose conservative treatment with sling immobilization. He achieved full range of shoulder motion in 3 months.
Case Report
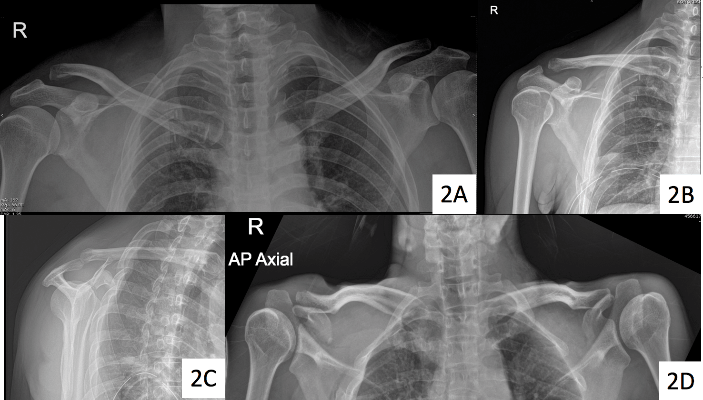
A 43-year-old Thai male had a motorcycle accident. He was initially unconsciousness at the scene and regained full consciousness at the emergency room. He had a hemothorax which was treated with chest tube insertion. When he was clinically stable, a complete physical examination was done, which found tender points at the proximal and distal parts of the right clavicle and also at the coracoid process. There was an abrasion wound 4x3 cm at the superior aspect of his right shoulder (Figures 1A, 1B, 1C). He was sent for a plain radiograph and computer tomography which revealed non-displaced fractures of the proximal and distal clavicle and also at the coracoid base (Figures 2A, 2B, 2C, 2D, 3A, 3B, 3C). Because all of the fractures were non-displaced, we discussed the treatment options with the patient. He chose conservative treatment with sling immobilization followed by a rehabilitation program. He was instructed to perform range-of-motion exercises of the elbow and wrist and pendulum exercises of the shoulder joint. At the 2 weeks follow-up, abduction and forward elevation 45 degrees exercises were added, and after 6 weeks active shoulder motion as tolerated.
Figure 1: The patient’s initial appearance in (A) anterior view, (B) posterior view and (C) lateral view.
Discussion
69% of clavicular fractures occur in the middle-third of the bone, 28% distally, and 3% proximally [1]. Ipsilateral proximal and distal clavicle fractures are rare with less than ten reports in the literature. Hagino reported two cases, one with middle and distal clavicular fractures and the other with the proximal and extra-articular distal clavicular fractures [2]. Our patient had a very unusual presentation, with fractures in the distal and proximal parts of the clavicle combined with the coracoid process fracture, a combination which has not previously been reported.
Figure 2: The initial radiographic imaging, (A) anteroposterior view of both clavicles, (B) anteroposterior view, (C) lateral transcapular view of the right shoulder and (D) serendipity view of both clavicles.
Figure 3: Initial computed tomography reconstruction, (A) frontal view, (B) lateral view and (C) top view.
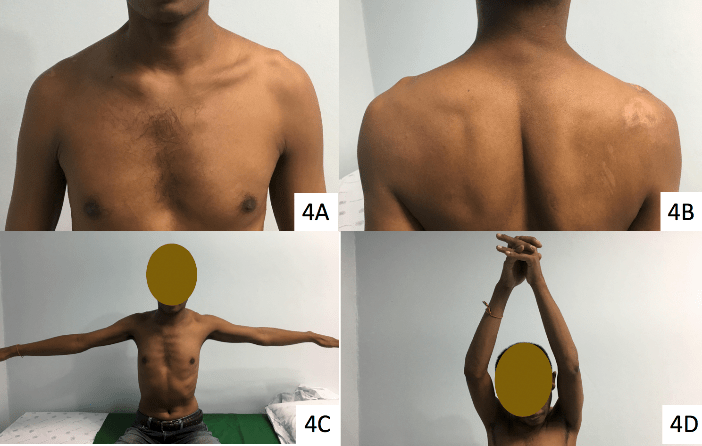
Figure 4: The patient’s appearance in (A) anterior view and (B) posterior view at 8-week follow up. The patient’s with (C) arm abduction and (D) arm forward flexion at 8-week follow up.
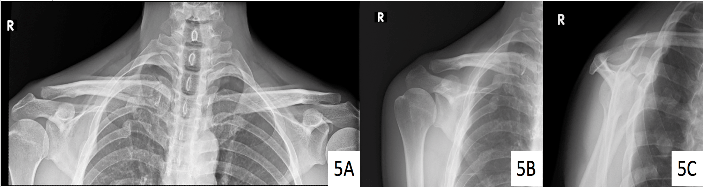
Figure 5: A radiographic imaging in (A) anteroposterior view of both clavicles, (B) anteroposterior view and (C) lateral transcapular view of the right shoulder at 8-week follow up.
There are two mechanisms of injury in clavicular fractures, a direct force that impacts the shoulder girdle from a fall, or a shearing force by an indirect injury from the humerus to the sternum by falling down in an out-stretched arm position. Although the mechanism that induced the proximal and distal clavicular fractures in our patient was not clearly understood, it seems probable that there was a combination of forces resulting in the ipsilateral injuries on the shoulder joint. Some direct force led to the distal clavicular fracture, a theory given further weight considering he also had a head injury. Proximal clavicle fractures can occur by an indirect force, either on the anterolateral or posterolateral aspect of the shoulder joint. Fractures of the proximal clavicle are difficult to diagnose from radiographic studies because the proximal part of the clavicle overlies the chest. Two studies have reported missing proximal clavicle fractures in cases of ipsilateral proximal and distal clavicle fractures. The doctor can detect a proximal clavicle fracture through clinical symptoms and radiographic investigations. The clinical symptoms include tenderness, swelling and ecchymosis around the proximal area of the clavicle. The doctor can also assess clavicular fractures using a serendipity radiographic view (Figure 2D). If the fracture cannot be evaluated through radiography, computed tomography can be used to identify the fracture and degree of displacement (Figures 3A, 3B, 3C). A patient with non-displaced ipsilateral proximal and distal clavicle fractures can be treated with conservative treatment with an arm sling. Displaced fractures, of course, should have surgery.The incidence of coracoid fractures is quite small, 3-13% of all scapular fractures and 5% of fractures around the shoulder joint [3]. The treatment options depend on the fracture pattern. This type of fracture is usually divided into two groups based on a classification system suggested by Ogawa and colleagues using the location of the fracture line. Fractures located behind the ligament attachment are classified as type I, while fractures anterior to the coracoclavicular (CC) ligaments are classified as type II. Type I fractures are usually unstable and normally require surgery, while type II fractures are usually stable, and the patient is usually treated with sling immobilization and physical therapy.
The combined fracture of the ipsilateral coracoid base and clavicular injury of the shoulder is quite rare. Latarjet et al. reported two cases of combined avulsion coracoid and clavicular fractures [4]. Baccarani et al. reported a single case of a clavicle with a displaced coracoid fracture that was treated with percutaneous two K-wire coracoid fixation, and at 4 months follow-up, the patient had regained full motion of the shoulder joint [5]. Seven cases of coracoid base fracture in a series by Martin-Herreo et al., reported one case combined with a clavicle fracture, and all seven cases were treated with conservative treatment with satisfactory results [6]. Ogawa et al. reported on 14 cases of ipsilateral clavicular and coracoid process fractures in which all of the coracoid process fractures were type II. The treatment of combined fractures around the shoulder joint is different from isolated fractures. Treatment must be based on the injury to the superior shoulder suspensory complex which consists of the glenoid bone, the coracoid process, the CC ligaments, distal clavicle, acromioclavicular joint and acromion. Injury of two structures in the SSSC is defined as a floating shoulder which should be treated operatively.
In the current case, the patient had injured two parts of the SSSC, the coracoid process and the distal clavicle, and one part of the proximal clavicle. In non-displaced fractures, the normal choice is conservative treatment with sling immobilization and early physical therapy. In our case, the results of this treatment were good. When healing was completed, the external appearance of the fracture sites was not different from the contralateral side (Figures 4A, 4B). The patient achieved near normal activity as shown in (Figures 4C, 4D). The follow-up radiographs are shown in (Figures 5A, 5B, 5C).
Conclusions
We present this case because there are no previous reports on this particular combination pattern. Conservative treatment was successful in this case.
Acknowledgements
The authors sincerely thank Virat Sakulvong for allowing us to disclose the information and Dave Patterson for English proofreading.
Article Info
Article Type
Case ReportPublication history
Received: Fri 08, Mar 2019Accepted: Fri 15, Mar 2019
Published: Tue 02, Apr 2019
Copyright
© 2023 Chaiwat Chuaychoosakoon. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.02.05
Author Info
Chaiwat Chuaychoosakoon Korakot Maliwankul Prapakorn Klabklay Ranaichanok Thongwichian Tanarat Boonriong Wachirapan Parinyakhup Yada Duangnumsawang
Corresponding Author
Chaiwat ChuaychoosakoonDepartment of Orthopaedic Surgery and Physical Medicine, Faculty of Medicine, Prince of Songkla University, 15 Karnjanavanich Road, Hat Yai, Songkhla 90112, Thailand
Figures & Tables


References
- Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br 80: 476-484. [Crossref]
- Hagino T, Ono T, Hamada Y (2002) Unusual double clavicle fracture complicated by ipsilateral scapular neck fracture. J Orthop Sci 7: 417-419. [Crossref]
- McGinnis M, Denton JR (1989) Fractures of the scapula: a retrospective study of 40 fractured scapulae. J Trauma 29: 1488-1493. [Crossref]
- Latarjet M, Michoulier J, Kohler R (1975) Fracture of the clavicle with avulsion of the coracoid plaque. Apropos of 2 cases. Chirurgie 101: 245-249. [Crossref]
- Baccarani G, Porcellini G, Brunetti E (1993) Fracture of the coracoid process associated with fracture of the clavicle: description of a rare case. Chir Organi Mov 78: 49-51. [Crossref]
- Martin-Herrero T, Rodriguez-Merchan C, Munuera-Martinez L (1990) Fractures of the coracoid process: presentation of seven cases and review of the literature. J Trauma 30: 1597-1599. [Crossref]
