Journals
Inter-Arm Blood Pressure Difference Among Nigerian Primary Care Patients— the Need for Dual Arm Blood Pressure Measurement
A B S T R A C T
Background: For many decades, hypertension guidelines have recommended dual-arm blood pressure measurement. However, the practice is poor in Nigerian primary care and its significance largely unidentified. Hence, the need to determine the significance of detecting inter-arm blood pressure difference among primary care patients in our local population. This study was done to determine the point prevalence of inter-arm blood pressure difference and its relationship with hypertension and diabetes mellitus.
Methods: A cross-sectional study was conducted among 214 respondents at the general outpatient clinic of a tertiary hospital in Nigeria. Demographic characteristics and anthropometric indices were obtained. Blood pressure readings were obtained through sequentially repeated measurements in respondents’ arms.
Results: One hundred and eighty-six respondents had complete data given a completion rate of 86.9%. Systolic blood pressure was higher on the right and left arm in 102 (54.8%) and 56 (30.1%) of the respondents respectively. Diastolic blood pressure was higher on the right and left arm in 73 (39.2%) and 63 (33.9%) of the respondents respectively. The overall prevalence of significant systolic inter-arm difference (≥ 10 mmHg) and diastolic inter-arm difference (≥ 10 mmHg) were 24.2% and 18.8% respectively. Significant systolic inter-arm difference (p=0.033) and diastolic inter-arm difference (p=0.01) were significantly more among respondents with hypertension and/or diabetes mellitus.
Conclusion: The blood pressure readings in both arms were different among majority of the respondents, being higher on the right arm in more of them. The prevalence of significant inter-arm difference was high in the unselected primary care patients studied especially among patients with hypertension and/or diabetes mellitus. Blood pressure measurement in both arms should become a routine practice during initial patients’ visits in primary care.
Keywords
Inter-arm blood pressure difference (IAD), systolic inter-arm difference (sIAD), diastolic inter-arm difference (dIAD), blood pressure measurement (BPM), primary care, dual-arm blood pressure measurement, Nigeria
Introduction
Blood pressure (BP) is the most widely measured medical metric in primary care [1]. Accuracy in its measurement is vital to prevent mismanagement of patients. This is particularly important during patients’ initial visits because the decision to commence anti-hypertensives or not depends on accurate BP measurement. Aside from the human and instrument-related errors that may affect BP measurement, acknowledgement of the fact that patients may have different blood pressures in both arms (inter-arm difference) is essential for the accurate diagnosis and continuous management of hypertension in primary care. This formed the basis for the advocacy by various hypertension guidelines for sequential or simultaneous BP checks in both arms at the initial patients’ visits and the use of the arm with a higher reading for immediate and subsequent clinical judgements [2-4].
The measurement of BP in both arms has received growing attention in the last decade because inter-arm difference has also been associated with peripheral vascular disease, increased cardiovascular and all-cause mortality [5-7]. An IAD of a few millimetres of mercury (mmHg) are quite normal, but any difference more than 10 mmHg could significantly increase the risk for adverse cardiovascular outcomes [5-7].
Unfortunately, these research findings have largely not translated into an expanded routine dual arm BP measurement in Nigerian primary care settings [8, 9]. Reports have shown that BP measurements at initial clinic visits in Nigerian primary care settings are taken using one arm [8, 9]. Although, there had been no previous research on why health care workers do not follow dual arm BP measurement, an anecdotal report has suggested time constraints and lack of awareness.
Majority of the studies on inter-arm BP difference were done in the developed world among respondents with or without cardiovascular risk factors [1, 5-7, 10, 11]. The few Nigerian studies were among secondary care patients and they pointed in no direction [8, 9, 12]. The true prevalence of IAD in Nigerian primary care settings is unknown. The paucity of studies on this subject among Nigerian primary care patients may be one reason why Nigerian primary care health workers have not adhered to dual arm BP measurement. A review of major guidelines on BP measurement by Parker et al. showed that most General Practitioners are aware of the recommendations to measure BP in both arms at initial visit, but they are wary of the recommendations unless justification together with evidence is provided on the importance of detecting IAD [13]. Perhaps, a study on this theme among primary care patients in Nigeria may give more insights on this topic and sensitize Nigerian General Practitioners and other primary care health workers on the relevance of dual arm BP measurement. This prompted the investigators to carry out this study among a heterogeneous general practice population in Nigeria. This study was done to determine the point prevalence of IAD and its relationship to hypertension and diabetes.
Materials and Methods
I Study Setting
This study was carried out in the General outpatient clinic (GOPC) of the Family Medicine department of a tertiary hospital in South-West Nigeria. All adult patients excluding those who need emergency treatment are first seen at the GOPC, where diagnoses are made. Patients who require primary care are managed and followed up in the clinic, while those who need further care are referred to the appropriate linear specialist clinics. The GOPC attendance was 14,016 adult patients in the year 2016 and this translates to a monthly average of 1,168.
II Study Design
This was a hospital-based, cross-sectional study.
III Study Population
All adult patients aged 18 years and above attending the GOPC.
IV Inclusion Criteria
Patients aged 18 years and above with or without a prior history of hypertension who consented to participate in the study.
V Exclusion Criteria
Patients with one arm, patients with an upper limb deformity, patients with severe illnesses that make it difficult for them to follow the study protocol and patients with major psychiatric illness were excluded from the study.
VI Sample Size
The sample size was estimated using the formula, n= z2 pq/d2; where n = sample size; p= proportion of respondents in previous Nigerian studies with IAD ≥ 10 mmHg which was 14.9% (0.149)8, q = 1-p (0.851); and d= the relative precision (0.05) [14]. The estimated minimum sample size was 194.84. However, in order to allow for missing data, an attrition value (10% of the estimated minimum sample size) was added. This gave a sample of 214 participants for the study.
VII Sampling Technique
Two hundred and fourteen respondents were selected from the patients that attended the GOPC using a systematic random sampling technique. The sampling interval ‘k’ of 6 (1168/214 = 5.5 ≈ 6) was used. The first person was selected from the first six patients arriving on each clinic day by balloting at the beginning of each clinic day. Thereafter, every consenting sixth person was recruited until the required number (214) was achieved.
VIII Data Collection
Data were obtained from patients who were eligible for the study. Data was collected using a questionnaire that consisted of socio-demographic variables, clinical variables, and physical examination. It contained information regarding patients’ demographic factors, co-morbid conditions like hypertension and diabetes mellitus, anthropometric variables and BP readings of the respondents. Hypertension was defined as the use of antihypertensive medication or one prior BP reading of ≥140/90 mmHg in addition to recruitment BP of ≥140/90 mmHg [15]. Patients were said to have diabetes mellitus if they were receiving oral hypoglycemic agents or insulin. Height (cm, converted to meter) and weight (kg) were measured according to the standard protocol [16, 17]. The body mass index (BMI) was calculated using the formula weight (kg)/height2 (m2) and stratification using the World Health Organization (WHO) classification of BMI was used: Normal 18.5-24.99kg/m2, Overweight 25.0-29.99kg/m2, and obese ≥ 30.0kg/m2 [16]. The waist circumference was also measured following the WHO protocol. A waist circumference of more than 40 inches (102 cm) in men and greater than 35 inches (88 cm) for women was considered abnormal [17].
BP measurement was done after the patient had rested for five minutes. The participants were made to sit comfortably in a chair with back support and both feet flat on the floor. The appropriately sized BP cuff was applied 2.5 centimeter above the ante-cubital fossa. Both palpatory and auscultatory methods were used to sequentially record the BP twice in each arm using a validated standard mercury sphygmomanometer. BP was first measured in one arm twice (with at least 2 minutes’ interval) without asking the patient which arm to start from. The cuff was then swapped to the other arm and two BP readings were also taken. The average of the two measurements for systolic and diastolic BP in each arm was calculated and recorded. The inter-arm systolic BP difference was the difference between average right arm systolic BP and the left. The inter-arm diastolic BP was also calculated. The IAD in blood pressure was taken as the absolute numeric character. Significant systolic and diastolic IAD were taken as systolic and diastolic blood pressure IAD of ≥10 mmHg [18].
IX Statistical Analysis
Data were analysed using the Statistical Package for Social Sciences™ (IBM Corp, Armonk, NY, USA) version 22.0. They were presented with tables and charts. Continuous variables were expressed as means±standard deviations. Categorical variables were described as frequencies and percentages. The comparison of patients’ parameters between patient groups divided by significant IAD (systolic/diastolic IAD ≥ 10mmHg) versus non-significant IAD (systolic/diastolic IAD < 10mmHg) was performed using the t-test or chi-squared test as appropriate. The difference in the mean blood pressures of the left and right arms was evaluated using the t-test. Statistical significance was defined as a p-value ≤ 0.05.
Results
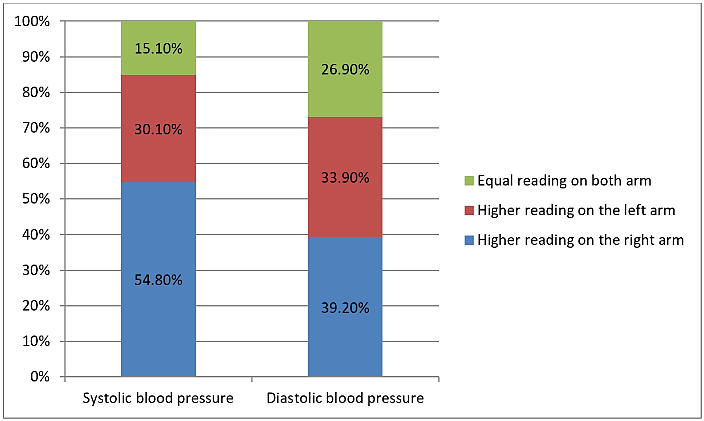
Sequential pairs of BP readings were taken from 214 participants. One hundred and eighty-six of them had complete data giving a completion rate of 86.9%. The mean age of the respondents was 48.16±14.59 years. Majority of them were female [n=112 (60.2%)]. The BMI (p<0.001) and waist circumference (p=0.031) were significantly higher in female respondents (Table 1). For the entire sample, the mean systolic BP and mean diastolic BP were higher in the right arm than the left arm. However, only the difference between the mean systolic BP readings in the 2 arms was significant (p=0.004) (Table 2). Systolic BP was higher in the right arm in 102 (54.8%) participants while 56 (30.1%) had higher left arm systolic BP readings. Twenty-eight (15.1%) had equal systolic BP in both arms. Seventy-three (39.2%) participants had higher right diastolic BP readings while 63 (33.9%) had higher left diastolic BP readings. The diastolic BP readings were equal in both arms in 50 (26.9%) participants (Figure 1).
Table 1: Baseline characteristics of the respondents.
|
Variables |
All patients N=186 |
Male N=74 |
Female N=112 |
p-value |
|
Age (years) |
48.16±14.59 |
47.28±14.36 |
48.74±14.77 |
0.506 |
|
Height (meter) |
1.64±0.09 |
1.71±0.08 |
1.60±0.06 |
0.349 |
|
Weight (kilogram) |
71.03±14.55 |
72.21±12.68 |
70.25±15.27 |
p<0.001 |
|
Body mass index(kg/m2) |
26.38±5.37 |
24.78±4.42 |
27.43±5.70 |
p<0.001 |
|
Waist circumference (cm) |
90.00±13.10 |
87.57±11.27 |
91.61±14.00 |
0.031 |
|
Right arm systolic blood pressure (SBP) (mmHg) |
130.35±23.99 |
126.53±20.16 |
132.88±25.99 |
0.077 |
|
Right arm diastolic blood pressure (DBP) (mmHg) |
81.10±14.09 |
80.76±13.61 |
81.32±14.45 |
0.790 |
|
Left arm systolic blood pressure (mmHg) |
128.79±24.37 |
124.18±20.04 |
131.84±26.50 |
0.035 |
|
Left arm diastolic blood pressure (mmHg) |
80.52±13.57 |
80.68±12.94 |
80.42±14.03 |
0.900 |
|
SBP inter-arm difference(mmHg) |
5.54±5.19 |
5.07±4.88 |
5.85±5.39 |
0.317 |
|
DBP inter-arm difference(mmHg) |
4.35±4.53 |
3.38±3.53 |
5.00±4.99 |
0.010 |
|
Diabetes mellitus |
18 (9.70%) |
4 (5.41%) |
14 (12.50%) |
0.109 |
|
Hypertension |
80 (43.01%) |
25 (33.8%) |
55 (49.1%) |
0.039 |
Table 2: Comparison of blood pressure measurement in both arms.
|
Blood pressure |
Right arm |
Left arm |
T |
P |
|
Systolic BP (mmHg) |
130.35±23.99 |
128.79±24.37 |
2.957 |
0.004 |
|
Diastolic BP (mmHg) |
81.10±14.09 |
80.52±13.57 |
1.282 |
0.201 |
Table 3: Prevalence of inter-arm blood pressure difference (IAD) among different groups.
|
Population |
Significant sIAD |
Significant dIAD |
||
|
No |
Yes |
No |
Yes |
|
|
No hypertension or diabetes (N=100) |
82 (82.0%) |
18 (18.0%) |
88 (88.0%) |
12 (12.0%) |
|
Hypertension only(N=67) |
46 (68.7%) |
21 (31.3%) |
53 (79.1%) |
14 (20.9%) |
|
Diabetes mellitus only (N=5) |
4 (80.0%) |
1 (20.0%) |
3 (60.0%) |
2 (40.0%) |
|
Hypertension coexisting with diabetes mellitus (N=14) |
9 (64.3%) |
5 (35.7%) |
7 (50.0%) |
7 (50.0%) |
|
All respondents (N=186) |
141 (75.8%) |
45 (24.2%) |
151 (81.2%) |
35 (18.8%) |
The mean absolute sIAD was 5.54±5.19 mmHg while the mean absolute dIAD was 4.35±4.53 mmHg (Table 1). Forty-five (24.2%) respondents showed significant sIAD (≥10 mmHg) while 35 (18.8%) respondents showed significant dIAD (≥10 mmHg). The prevalence of significant sIAD (18.0%) and dIAD (12.0%) was least among respondents without hypertension and diabetes mellitus (Table 3). Respondents with sIAD of ≥10 mmHg had a significantly higher mean right arm systolic BP than respondents with sIAD of < 10 mmHg (p=0.011) (Table 4).
Table 4: Association between participants’ characteristics and significant IAD (continuous data).
|
Variables |
Significant sIAD |
|
Significant dIAD |
|
||
|
No (N=141) |
Yes (N=45) |
p-value |
No (N=151) |
Yes (N=35) |
p-value |
|
|
Mean age (years) |
48.01±14.19 |
48.62±15.94 |
0.808 |
47.63±14.18 |
50.46±16.24 |
0.303 |
|
Mean height (m) |
1.64±0.09 |
1.64±0.08 |
0.580 |
1.65±0.09 |
1.62±0.07 |
0.065 |
|
Mean weight (kg) |
71.56±14.64 |
69.38±14.28 |
0.382 |
71.78±14.22 |
67.80±15.67 |
0.145 |
|
Mean BMI (kg/m2) |
26.52±5.44 |
25.95±5.20 |
0.534 |
26.47±5.26 |
25.98±5.91 |
0.622 |
|
Mean waist circumference (cm) |
90.39±12.83 |
88.80±13.98 |
0.479 |
90.00±13.01 |
90.01±13.66 |
0.996 |
|
Mean left arm SBP (mmHg) |
126.96±22.97 |
134.51±27.82 |
0.070 |
127.94±24.13 |
132.46±25.41 |
0.344 |
|
Mean right arm SBP (mmHg) |
127.84±22.79 |
138.22±26.13 |
0.011 |
129.15±23.63 |
135.54±25.18 |
0.156 |
|
Mean left arm DBP (mmHg) |
80.06±13.35 |
81.98±14.31 |
0.410 |
80.74±13.56 |
79.57±13.78 |
0.647 |
|
Mean right arm DBP (mmHg) |
80.06±13.66 |
84.36±15.04 |
0.075 |
80.98±13.84 |
81.60±15.33 |
0.815 |
Table 5: Association between participants’ characteristics and significant IAD (categorical data).
|
Variable |
|
Significant sIAD |
|
Significant dIAD |
|
||
|
Categories |
No (N=141) |
Yes (N=45) |
p-value |
No (N=151) |
Yes (N=35) |
p-value |
|
|
Age grouped |
Young Middle age Adult |
40 (75.5) 72 (75.8) 29 (76.3) |
13 (24.5) 23 (24.2) 9 (23.7) |
0.996 |
42 (79.2) 82 (86.3) 27 (71.1) |
11 (20.8) 13 (13.7) 11 (28.9) |
0.115 |
|
Gender |
Male Female |
61 (82.4%) 80 (71.4%) |
13 (17.6%) 32 (28.6%) |
0.086 |
66 (89.2%) 85 (75.9%) |
8 (10.8%) 27 (24.1%) |
0.023 |
|
Presence of hypertension or diabetes |
Yes No |
59 (68.6%) 82 (82.0) |
27 (31.4%) 18 (18.0%) |
0.033 |
63 (73.3%) 88 (88.0%) |
23 (26.7%) 12 (12.0%) |
0.01 |
|
JNC 7 stage of high blood pressure |
Normal Prehypertension Stage 1 Stage 2 |
52 (83.9%) 41 (82.0%) 31 (68.9%) 17 (58.6%) |
10 (16.1%) 9 (18.0%) 14 (31.1%) 12 (41.4%) |
0.028 |
53 (85.5%) 42 (84.0%) 35 (77.8%) 21 (72.4%) |
9 (14.5%) 8 (16.0%) 10 (22.2%) 8 (27.6%) |
0.422 |
Figure 1: Systolic and diastolic blood pressure measurement of both arms (Bar chart showing the systolic and diastolic blood pressure measurement of both arms).
Explanatory Legend for Figure 1: Participants with systolic and diastolic BP greater than 140 mmHg and 90 mmHg were regarded as having hypertension. Among the 214 participants, 54.8% of the participants had a higher systolic BP in the right arm, whereas 30.1% had higher systolic BP in the left arm. 15.1% had equal systolic BP in both arms. 39.2% participants had higher right diastolic BP readings while 33.9% had higher left diastolic BP readings. The diastolic BP readings were equal in both arms in 26.9% participants.
Respondents with hypertension and diabetes mellitus have significant sIAD (p=0.033) and significant dIAD (0.01) compared to respondents without hypertension and diabetes mellitus. The proportion of respondents with significant sIAD increases with increasing severity of hypertension (p=0.028). Significant dIAD was more common among female respondents (p=0.023) (Table 5). The sIAD and dIAD were unrelated to age and anthropometric variables (Tables 4 & 5).
Discussion
The mean systolic BP and diastolic BP readings on the right arm were higher than those of the left arm and the difference was significant in the case of systolic BP. The previous reports on this subject are conflicting [9, 19-22]. Similar to this study, several studies have also reported higher BP readings in the right arm compared to the left [19-21]. On the other hand, Clark and others systematically reviewed studies on IAD and found no overall evidence in favour of a higher BP on the right arm [22]. A previous Nigerian study also showed no significant difference between the BP readings of the right and left arm [9]. Hence, the finding that higher BP readings are more frequent in one arm than the other may be for educational purpose with no clinical significance because there is still a chance of higher BP reading in any of the arms for every BP measurement especially across a population. The possibility of higher BP reading in either arm further justifies the guidelines’ recommendation of dual arm BP measurements at the initial visit, and subsequent measurement of BP in the arm with higher reading [2-4].
This study showed that significant IAD is a common finding in a population of unselected primary care patients. The present study reported an overall prevalence of 24.2% and 18.8% for significant sIAD and dIAD respectively. The clinical implication of this finding is that almost a quarter of unselected primary care patients may have their BP underestimated by 10 mmHg if IAD is not specifically excluded. It is noteworthy though that the reduction in the BP of 10 mmHg can prevent fatal and non-fatal coronary events and stroke [15]. Thus, significant IAD should be sought out for during clinical assessment of BP.
There was no previous study on the prevalence of inter-arm BP difference in unselected general practice population in Nigeria to compare our findings with. The prevalence of significant IAD in the present study was, however, higher than those stated in a Nigerian study conducted among secondary care hypertensive and normotensive adult Nigerians, which reported a prevalence of 14.9% and 9.1% for significant sIAD and dIAD respectively [8]. A literature searches on the prevalence of significant IAD in developed and developing countries showed a range of 5.0-39% for a significant sIAD and 3.8-23.2% for significant dIAD [1, 8, 19, 22, 23]. Although, the prevalence of significant sIAD and dIAD in this study is comparable to previously reported prevalence, the higher prevalence found in this study is interpreted with caution because of the sequential BP measurement protocol used. Clark and others in their systematic review reported that the prevalence of IAD is overestimated threefold by sequential measurement compared to repeated simultaneous BP measurement protocol [24].
In spite of the risk of overestimation that may occur with the use of sequential BP measurement protocol, the sequential measurement with standard mercury sphygmomanometer may still be the most feasible and practical way of dual arm BP measurement during a routine clinic in resource-poor countries when one considers the cost implication of simultaneous BP measurement protocol. In addition, a single sequential pair of measurements has also been shown to rule out significant IAD with a high negative predictive value [20, 24]. Furthermore, the consistent finding of a relationship between significant IAD and cardiovascular events using the sequential approach further showed that sequential protocol of measuring IAD is still relevant [20, 24].
The large proportion of respondents with hypertension and diabetes mellitus may also contribute to the high prevalence of significant sIAD and dIAD. The prevalence of significant sIAD and dIAD was higher among respondents who had hypertension and diabetes mellitus compared to those without these diseases in the study. Aside from the finding of a high prevalence of significant sIAD and dIAD in respondents who have hypertension and diabetes mellitus, the prevalence of significant sIAD also rose with increasing severity of hypertension in this study. The finding of a direct relationship between the presence of cardiovascular disease and significant IAD in this study concurred with findings from other studies [5-7, 11, 19, 20-23]. The associations of IAD with these cardiovascular diseases may be useful in primary care in Nigeria with shrinking and finite resources. The detection of significant IAD through BP measurement may serve as a simple cost-effective tool in primary care to identify patients who may benefit from further screening for cardiovascular diseases.
Female participants had a higher prevalence of significant sIAD and dIAD than their male counterparts and this was significant in the dIAD. Similar to this study, some previous studies have reported a higher prevalence of significant IAD among female respondents, whereas others have failed to demonstrate this [1, 11, 23, 25-27]. The high prevalence of significant IAD among female participants in this study can be attributed to the higher proportion of female respondents in the study population and consequent higher prevalence of obesity, diabetes mellitus and hypertension among the female participants in this study may also be contributory to this finding.
Our study showed that age was not associated with IAD. The association between IAD and age in previous studies is conflicting. While our finding was in consonance with some previous reports, other studies reported association between age and IAD [1, 11, 23, 26, 27]. The relationship in the later studies were either direct or inverse [11, 23, 27]. The direct or inverse relationship between age and IAD that were reported in these studies and the finding of an approximately equal prevalence of significant IAD across different age groups in the index study underscore the importance of screening everyone for IAD through dual arm BP measurement irrespective of their age.
Implications for Research and Practice
The high prevalence of significant IAD among the unselected primary care patients in this new study supports the current clinical guideline to measure BP in both arms at the initial visit and subsequently use the arm with the higher BP for continued management. The chances of getting a higher BP on either arm, though, greater on the right arm compared to left arm in this study further justifies the guidelines’ recommendation of an initial dual arm BP measurement [2-4].
Unfortunately, this guideline is not routinely followed in many primary care settings in Nigeria. The non-exclusion of IAD in patients may lead to under-diagnosis of hypertension, misdiagnosis of hypotension or under-treatment of hypertensive patients. The disparity can be enormously important to certain individuals that we see at primary care who are applying for life insurance, pre-employment fitness assessment, or military/paramilitary service, particularly when only the arm with the higher pressure is used for BP measurement.
Therefore, the assessment of BP in both arms should become routine in our clinics. The incorporation of bilateral arm BP measurement into our various clinical training programmes at both undergraduate and postgraduate that lacks this practice may also improve the practice of dual arm BP measurement. The single sequential BP measurement protocol which has been shown to reliably rule patients out of the need for subsequent pair of BP measurement may be the most practical method for now [11]. The facilitators and obstacles to dual arm BP measurement should also be explored through qualitative research.
The association of an IAD with hypertension and/or diabetes mellitus makes bilateral arm blood pressure measurement in these groups of patients appropriate to prevent under-treatment. In addition, identification of IAD in patients should trigger the consideration of cardiovascular diseases which may require further screening and investigations especially in primary care settings in Nigeria with limited health resources.
Conclusion
There is a chance of getting higher BP readings on either arm, though, greater on the right arm compared to left arm in this study. The prevalence of significant IAD is high in unselected primary care patients. This is particularly more marked among patients with hypertension and/or diabetes mellitus. BP measurement in both arms should become a routine clinical practice at initial patients’ visit in primary care.
Strength and Limitations
This is the first Nigerian study on IAD among unselected primary care patients. The study used the sequential method of BP measurement which might have resulted in the over-estimation of the prevalence of significant IAD. Further works that assess the prevalence of IAD among the unselected primary care patients using the simultaneous BP measurement protocol is needed. In addition, the study is a cross-sectional, one-center study; therefore, some caution may be needed in the generalization of these results. Some patients with previously undiagnosed diabetes mellitus may have been missed due to the use of self-report in determining the prevalence of diabetes mellitus among the participants.
Acknowledgments
We appreciate our colleagues in the department of family medicine, Federal Medical Centre, Abeokuta, Nigeria for their immense contributions at every stage of this research work.
Ethical Consideration and Consent
Ethical approval for the study was obtained from the Health Research Ethics Committee of the hospital with protocol number FMCA/470/HREC/11/2016 and registration number FWA/Q0018660/02/28/2017.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Sat 01, Aug 2020Accepted: Tue 01, Sep 2020
Published: Mon 14, Sep 2020
Copyright
© 2023 Oluwaseun Solomon Ojo. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.04.13
Author Info
Oluwaseun Solomon Ojo Akinfemi Joel Fatusin Bolatito Betty Fatusin Ademola Oluwaseun Egunjobi Sunday Olukayode Malomo Peter Taiwo Sogunle Adegbola Meeden Ige Babajide Adekoyejo Taiwo Ayo Adesokan Nurudeen Adigun Gbadamosi Odunola Olaitan Ojo
Corresponding Author
Oluwaseun Solomon OjoFamily Medicine Department, Federal Medical Centre, Abeokuta, Nigeria
Figures & Tables
Table 1: Baseline characteristics of the respondents.
|
Variables |
All patients N=186 |
Male N=74 |
Female N=112 |
p-value |
|
Age (years) |
48.16±14.59 |
47.28±14.36 |
48.74±14.77 |
0.506 |
|
Height (meter) |
1.64±0.09 |
1.71±0.08 |
1.60±0.06 |
0.349 |
|
Weight (kilogram) |
71.03±14.55 |
72.21±12.68 |
70.25±15.27 |
p<0.001 |
|
Body mass index(kg/m2) |
26.38±5.37 |
24.78±4.42 |
27.43±5.70 |
p<0.001 |
|
Waist circumference (cm) |
90.00±13.10 |
87.57±11.27 |
91.61±14.00 |
0.031 |
|
Right arm systolic blood pressure (SBP) (mmHg) |
130.35±23.99 |
126.53±20.16 |
132.88±25.99 |
0.077 |
|
Right arm diastolic blood pressure (DBP) (mmHg) |
81.10±14.09 |
80.76±13.61 |
81.32±14.45 |
0.790 |
|
Left arm systolic blood pressure (mmHg) |
128.79±24.37 |
124.18±20.04 |
131.84±26.50 |
0.035 |
|
Left arm diastolic blood pressure (mmHg) |
80.52±13.57 |
80.68±12.94 |
80.42±14.03 |
0.900 |
|
SBP inter-arm difference(mmHg) |
5.54±5.19 |
5.07±4.88 |
5.85±5.39 |
0.317 |
|
DBP inter-arm difference(mmHg) |
4.35±4.53 |
3.38±3.53 |
5.00±4.99 |
0.010 |
|
Diabetes mellitus |
18 (9.70%) |
4 (5.41%) |
14 (12.50%) |
0.109 |
|
Hypertension |
80 (43.01%) |
25 (33.8%) |
55 (49.1%) |
0.039 |
Table 2: Comparison of blood pressure measurement in both arms.
|
Blood pressure |
Right arm |
Left arm |
T |
P |
|
Systolic BP (mmHg) |
130.35±23.99 |
128.79±24.37 |
2.957 |
0.004 |
|
Diastolic BP (mmHg) |
81.10±14.09 |
80.52±13.57 |
1.282 |
0.201 |
Table 3: Prevalence of inter-arm blood pressure difference (IAD) among different groups.
|
Population |
Significant sIAD |
Significant dIAD |
||
|
No |
Yes |
No |
Yes |
|
|
No hypertension or diabetes (N=100) |
82 (82.0%) |
18 (18.0%) |
88 (88.0%) |
12 (12.0%) |
|
Hypertension only(N=67) |
46 (68.7%) |
21 (31.3%) |
53 (79.1%) |
14 (20.9%) |
|
Diabetes mellitus only (N=5) |
4 (80.0%) |
1 (20.0%) |
3 (60.0%) |
2 (40.0%) |
|
Hypertension coexisting with diabetes mellitus (N=14) |
9 (64.3%) |
5 (35.7%) |
7 (50.0%) |
7 (50.0%) |
|
All respondents (N=186) |
141 (75.8%) |
45 (24.2%) |
151 (81.2%) |
35 (18.8%) |
Table 4: Association between participants’ characteristics and significant IAD (continuous data).
|
Variables |
Significant sIAD |
|
Significant dIAD |
|
||
|
No (N=141) |
Yes (N=45) |
p-value |
No (N=151) |
Yes (N=35) |
p-value |
|
|
Mean age (years) |
48.01±14.19 |
48.62±15.94 |
0.808 |
47.63±14.18 |
50.46±16.24 |
0.303 |
|
Mean height (m) |
1.64±0.09 |
1.64±0.08 |
0.580 |
1.65±0.09 |
1.62±0.07 |
0.065 |
|
Mean weight (kg) |
71.56±14.64 |
69.38±14.28 |
0.382 |
71.78±14.22 |
67.80±15.67 |
0.145 |
|
Mean BMI (kg/m2) |
26.52±5.44 |
25.95±5.20 |
0.534 |
26.47±5.26 |
25.98±5.91 |
0.622 |
|
Mean waist circumference (cm) |
90.39±12.83 |
88.80±13.98 |
0.479 |
90.00±13.01 |
90.01±13.66 |
0.996 |
|
Mean left arm SBP (mmHg) |
126.96±22.97 |
134.51±27.82 |
0.070 |
127.94±24.13 |
132.46±25.41 |
0.344 |
|
Mean right arm SBP (mmHg) |
127.84±22.79 |
138.22±26.13 |
0.011 |
129.15±23.63 |
135.54±25.18 |
0.156 |
|
Mean left arm DBP (mmHg) |
80.06±13.35 |
81.98±14.31 |
0.410 |
80.74±13.56 |
79.57±13.78 |
0.647 |
|
Mean right arm DBP (mmHg) |
80.06±13.66 |
84.36±15.04 |
0.075 |
80.98±13.84 |
81.60±15.33 |
0.815 |
Table 5: Association between participants’ characteristics and significant IAD (categorical data).
|
Variable |
|
Significant sIAD |
|
Significant dIAD |
|
||
|
Categories |
No (N=141) |
Yes (N=45) |
p-value |
No (N=151) |
Yes (N=35) |
p-value |
|
|
Age grouped |
Young Middle age Adult |
40 (75.5) 72 (75.8) 29 (76.3) |
13 (24.5) 23 (24.2) 9 (23.7) |
0.996 |
42 (79.2) 82 (86.3) 27 (71.1) |
11 (20.8) 13 (13.7) 11 (28.9) |
0.115 |
|
Gender |
Male Female |
61 (82.4%) 80 (71.4%) |
13 (17.6%) 32 (28.6%) |
0.086 |
66 (89.2%) 85 (75.9%) |
8 (10.8%) 27 (24.1%) |
0.023 |
|
Presence of hypertension or diabetes |
Yes No |
59 (68.6%) 82 (82.0) |
27 (31.4%) 18 (18.0%) |
0.033 |
63 (73.3%) 88 (88.0%) |
23 (26.7%) 12 (12.0%) |
0.01 |
|
JNC 7 stage of high blood pressure |
Normal Prehypertension Stage 1 Stage 2 |
52 (83.9%) 41 (82.0%) 31 (68.9%) 17 (58.6%) |
10 (16.1%) 9 (18.0%) 14 (31.1%) 12 (41.4%) |
0.028 |
53 (85.5%) 42 (84.0%) 35 (77.8%) 21 (72.4%) |
9 (14.5%) 8 (16.0%) 10 (22.2%) 8 (27.6%) |
0.422 |
References
- C E Clark, J L Campbell, R J Powell (2007) The inter-arm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: cohort study. J Hum Hypertens 21: 633-638. [Crossref]
- J C Petrie, E T O'Brien, W A Littler, M de Swiet (1986) Recommendations on blood pressure measurement. Br Med J (Clin Res Ed) 293: 611-615. [Crossref]
- Giuseppe Mancia, Robert Fagard, Krzysztof Narkiewicz, Josep Redón, Alberto Zanchetti et al (2013) 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 31: 1281-1357. [Crossref]
- National Clinical Guideline Centre (UK) (2006) Hypertension: The Clinical Management of Primary Hypertension in Adults [Internet]. [Crossref]
- James White, Laust H Mortensen, Mika Kivimäki, Catharine R Gale, G David Batty (2014) Inter-arm differences in systolic blood pressure and mortality among US army veterans: aetiological associations and risk prediction in the Vietnam experience study. Eur J Prev Cardiol 21: 1394-1400. [Crossref]
- Christopher E Clark, Rod S Taylor, Angela C Shore, John L Campbell (2012) The difference in blood pressure readings between arms and survival: primary care cohort study. BMJ 344: e1327. [Crossref]
- Jinkwon Kim, Tae Jin Song, Dongbeom Song, Hye Sun Lee, Chung Mo Nam et al. (2013) Interarm blood pressure difference and mortality in patients with acute ischemic stroke. Neurology 80: 1457-1464. [Crossref]
- Ayodele OE, Akintunde AA, Akinboro AO, Gbadegesin BA, Olayinka O (2015) Inter-arm blood pressure difference in hypertensive and normotensive adult Nigerian.
- Igbokwe VU, Adebayo Gege GI, Seriki AS (2017) Prevalence of Inter-Arm Blood Pressure Difference in Normal and Hypertensive Patients. J Cardiol & Cardiovasc Ther 7: 555716.
- Christopher E Clark, Colin J Greaves, Philip H Evans, Andy Dickens, John L Campbell (2009) Inter-arm blood pressure difference in type 2 diabetes: a barrier to effective management? Br J Gen Pract 59: 428-432. [Crossref]
- Christopher E Clark, Anna M Steele, Rod S Taylor, Angela C Shore, Obioha C Ukoumunne et al. (2014) Interarm blood pressure difference in people with diabetes: measurement and vascular and mortality implications: a cohort study. Diabetes Care 37: 1613-1620. [Crossref]
- Maduagwu SM, Umeonwuka CI, Mohammad HH, Oyeyemi AY, Nelson EC, et al. (2018) Reference Arm Blood Pressure Measurement in Stroke Survivors. Middle East J Rehabil Health Stud 5: e62368.
- Parker E, Glasziou P (2009) Use of evidence in hypertension guidelines: should we measure in both arms? Br J Gen Pract 59: e87-e92. [Crossref]
- Araoye MO (2003) Subject selection: sample size determination In: MO Araoye, editor. Research methodology with statistics for health and social sciences, 1st ed. Ilorin: Nathadex 117-118.
- Aram V Chobanian, George L Bakris, Henry R Black, William C Cushman, Lee A Green et al. (2003) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289: 2560-2572. [Crossref]
- World Health Organization (2004) The international classification of adult underweight, overweight and obesity according to BMI. Geneve: WHO.
- World Health Organization (2008) Waist circumference and waist-hip ratio: report of a WHO expert consultation. Geneva: World Health Organization (WHO).
- Kurian S, Joseph RP, Manjula VD (2017) Raised inter-arm difference in blood pressure: Association with family history of hypertension, anthropometric parameters, and mean arterial blood pressure. Natl J Physiol Pharm Pharmacol 7: 55-59.
- Rajiv Agarwal, Zerihun Bunaye, Dagim M Bekele (2008) Prognostic significance of between-arm blood pressure differences. Hypertension 51: 657-662. [Crossref]
- Christopher E Clark, Rod S Taylor, Isabella Butcher, Marlene Cw Stewart, Jackie Price et al. (2016) Inter-arm blood pressure difference and mortality: a cohort study in an asymptomatic primary care population at elevated cardiovascular risk. Br J Gen Pract 66: e297-e308. [Crossref]
- Verma N, Somesh R, Kumar P, Kumai R, Bhardwaj K (2016) Inter arm systolic blood pressure difference is associated with a high prevalence of cardiovascular diseases. Int J Res Med Sci 4: 1177-1180.
- C E Clark, J L Campbell, P H Evans, A Millward (2006) Prevalence and clinical implications of the inter-arm blood pressure difference: a systematic review. J Hum Hypertens 20: 923-931. [Crossref]
- Su A Kim, Jang Young Kim, Jeong Bae Park (2016) Significant interarm blood pressure difference predicts cardiovascular risk in hypertensive patients CoCoNet study. Medicine. 95: e3888. [Crossref]
- Clark CE, Taylor RS, Shore AC, Campbell JL (2016) Prevalence of systolic inter-arm differences in blood pressure varies for different primary care populations: systematic review and metaanalysis. Br J Gen Pract 66: e838-e847. [Crossref]
- Sharma B, Ramawat P (2016) Prevalence of inter-arm blood pressure difference among clinical out-patients. Int J Health Sci (Qassim) 10: 229-237. [Crossref]
- Deirdre Lane, Michele Beevers, Nicola Barnes, James Bourne, Andrew John et al. (2002) Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens 20: 1089-1095. [Crossref]
- Ling Sun, Ting Zou, Bao Zhu Wang, Fen Liu, Qing Hua Yuan et al. (2018) Epidemiological investigation into the prevalence of abnormal inter-arm blood pressure differences among different ethnicities in Xinjiang, China. PLoS One 13: e0188546. [Crossref]
