Innovative Approach of Endosonographic Radioactive Labeling of an Ectopic Parathyroid Adenoma by Technetium-99m Human Serum Albumin: A Case Report
A B S T R A C T
Primary hyperparathyroidism caused by parathyroid adenoma requires surgical resection. To confine the extent of surgery to the very minimum and to exclude an atypical adenoma location, preoperative imaging aims at identifying the suspicious gland. For this purpose, Technetium-99m (99mTc)-sestamibi scintigraphy and SPECT have become the international imaging standard, in inconclusive cases also with C-11 methionine and F-18 choline PET/CT. We present a case of surgery for an ectopic retroesophageal adenoma resected under gamma probe guidance after preoperative radioactive targeting. A 73-year-old patient, who was diagnosed with primary hyperparathyroidism, presented to our outpatient clinic. The patient was symptom-free, but during a routine check-up, parathormone levels of 127 pg/ml (normal range 15-65) were detected. Parathyroid MIBI scintigraphy, including SPECT/CT, failed to locate an adenoma. Therefore, a PET/MRI scan with 164 MBq F-18 choline was applied and a single parathyroid adenoma was detected in a very untypical retroesophageal and prevertebral position, respectively. Due to its esophageal proximity and to enable a very confined surgery, endosonography was performed and the adenoma was transesophageally injected with 75 MBq 99mTc-human serum albumin (HSA). The next day gamma probe-guided minimally invasive resection was performed without any intra- or postoperative complications. Minimally invasive resection of parathyroid adenomas should be the standard but may be difficult in deep collar and atypical locations. Marking the adenoma with a radioactive nanocolloid tracer for gamma probe-guided surgery can be considered an innovative approach to maintain minimal invasive therapy for ectopic adenomas.
Keywords
Gamma probe-guided surgery, 99mTc-human serum albumin, Primary Hyperparathyroidism, Parathyroidectomy, Endoscopic Ultrasonography, Case report
Introduction
Primary hyperparathyroidism (PHPT) is a common endocrine disease caused by dysregulated parathyroid hormone secretion. In 75-85 % of cases, underlying reason is a single parathyroid adenoma [1]. The remainder may be due to multiglandular hyperplasia or rarely (1 %) to parathyroid carcinoma. Surgical resection is the first-line therapy and is successful in 80-95 % of the cases [1, 2]. Difficulties in removing adenomas may arise with ectopic parathyroid adenomas, which are present in up to 16 % of patients [3]. The main cause of persistent hyperparathyroidism after resection is additional ectopically located parathyroid glands that were not found during the initial operation [2, 4]. For this reason, a multimodality diagnostic approach including 99mTc-sestamibi scintigraphy and single photon emission computed tomography/computed tomography (SPECT/CT) is necessary and has become the standard. In rare cases, when the aforementioned modalities fail in localizing a hyperfunctioning gland, F-18 choline or C-11 methionine positron emission tomography/magnetic resonance imaging (PET/MRI) can be used as a new hybrid and most sensitive imaging technique to detect the adenoma [5]. This technique offers advantages over conventional MRI or CT scans for functional and soft tissue analysis of complex anatomical regions [6].
Accurate localization of these adenomas not only has diagnostic significance, but may also pave the way for a targeted surgical strategy that avoids conventional bilateral neck exploration. Compared with the conventional approach, minimally invasive parathyroidectomy (MIP) is considered to be superior in terms of healing, operative time, postoperative recovery, and complication rates, especially in ectopic sites [7, 8]. MIP can be further facilitated by the use of an intraoperative hand-held gamma probe, however requires prior radioactive marking of the lesion [9, 10]. This case report presents an innovative approach in which endosonography was used to apply the radiotracer directly into the adenoma located in an ectopic retroesophageal position.
Methods
This case report was written in accordance with the SCARE guidelines for case reports [11].
Case Report
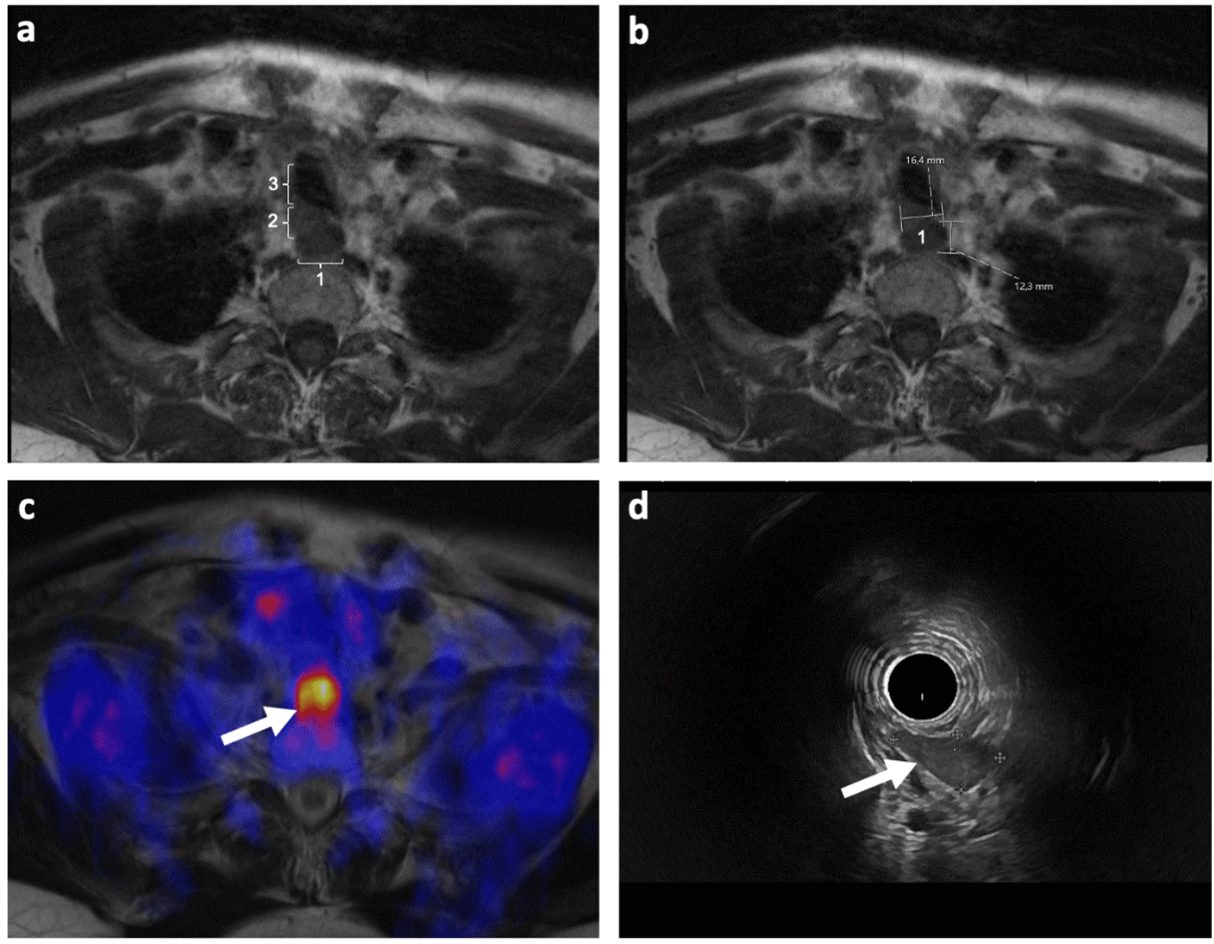
A 73-year-old patient presented to our tertiary center with primary hyperparathyroidism. Elevated parathormone levels of 127 pg/ml (normal range 15-65) were a coincidental finding by means of a laboratory control before cataract surgery. Calcium was 2.68 mmol/L (normal range 2.2-2.65). Otherwise, the patient was symptom-free. Regarding his past medical history, no other medical conditions were present. The patient did not take any medication and had no allergies. In parathyroid scintigraphy with 99mTc-sestamibi, a possible parathyroid adenoma dorsolateral to the left lower pole of the thyroid gland was suspected. However, no morphological correlate could be detected on SPECT/CT (low dose CT) image fusion. Ultrasonography was not helpful either. Therefore, a MRI scan (Figures 1a & 1b) with an additional 164 MBq F-18 choline application was performed. The tracer accumulated retroesophageally at the level of vertebral bodies 1 to 2 (Figure 1c). The suspicious region could be confirmed by endoscopic ultrasound (EUS) (Figure 1d).
Figure 1: Preoperative diagnostics. a and b) MRI: T1 sequence showing the ectopic adenoma (2.1 x 1.6 x 1.2 cm) (1), the esophagus (2) and the cervical trachea (3) c) F-18 choline PET/MR transversal slice showing only uptake of the adenoma (white arrow). d) In endosonography, the adenoma is well localized (white arrow).
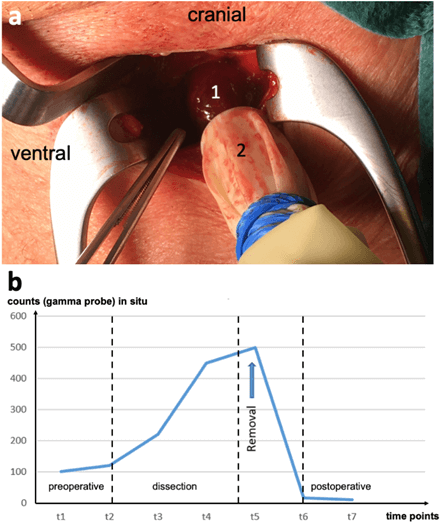
Due to its unfavourable location and the proximity to harmful structures, gamma probe-guided surgery was intended. Therefore, radioactive marking of the adenoma was performed one day before surgery via EUS. A 19 Gauge needle was positioned under endosonographic visual control and 0.5 ml / 75 MBq of 99mTc-HSA were injected. The next day (7 months after initial presentation), the patient underwent gamma probe-guided MIP of the ectopic prevertebral adenoma (Figure 2a). Intraoperatively, the exact location of the activity could be defined by the gamma probe. Gentle dissection of the adenoma over a tiny incision was feasible and succeeded in resection of the adenoma. Re-examination of the neck revealed no further radioactivity, whereas the resected mass showed high activity (Figure 2b). In addition, intraoperative measurement of parathyroid hormones was performed, which showed a fast decrease to a normal level. On postoperative day 1, parathyroid hormone and calcium levels were normal; the patient showed no complications and could be discharged on the same day.
Figure 2: Intraoperative site. a) Intraoperative position of the retroesophageally located parathyroid gland (1): detection confirmation by the gamma probe (2). b) Gamma probe count rates in situ during and after surgery. The control time point (t7) indicates complete removal of the targeted adenoma.
Discussion
The underlying mechanism of PHPT is an excessive secretion of parathyroid hormone caused by enlarged parathyroid glands. PHPT is a common endocrine disorder [12]. In Europe, the estimated prevalence of PHPT is 3-4.3 per 1,000 overall and reaches the prevalence of 21 per 1,000 in women aged 55-75 years [13, 14]. The classic symptom triad of PHPT includes nephrolithiasis, painful bones, and frequent peptic ulcers. In addition, patients may report muscle weakness, fatigue, and depression. However, most patients, including our case, are asymptomatic at the time of diagnosis (~85 % in developed countries). Without surgical intervention, PHPT will progress in one-third of affected individuals over a 15-year period [15]. Guidelines for asymptomatic patients were developed in 1990 to define under what conditions patients may benefit from parathyroidectomy [16]. These guidelines were updated in 2014 and the threshold serum calcium level at which surgical intervention is recommended is > 1 mg/dL (> 0.25 mmol/L) above the upper limit of the normal range [17]. After successful parathyroid surgery, reduced bone density improves, the incidence of recurrent kidney stones decreases, and similarly, there may be improvements in neurocognitive symptoms such as depression or fatigue [17].
A total of 15.9 % of parathyroid glands are located in ectopic sites. Of these, 51.7 % are located in the retroesophageal/paraesophageal space or in the thyroid gland [18]. Localization and treatment of ectopic parathyroid adenomas can be challenging. Various imaging techniques such as ultrasound, CT or MRI scans, 99mTc-sestamibi scintigraphy or SPECT/CT are available nowadays to confirm the diagnosis and exact localization [19]. In our patient, both 99mTc-sestamibi scintigraphy and SPECT/CT examination failed to precisely localize the adenoma due to the atypical position and the low dose CT (no contrast enhancement). However, F-18 choline PET/MRI successfully localized the parathyroid adenoma. Functional PET imaging by radiotracers such as F-18 choline or C-11 methionine allows the detection of parathyroid adenomas with high sensitivity [20]. Furthermore, in addition to the known diagnostic modalities, EUS is proposed as another diagnostic tool for the detection of parathyroid adenomas and was also successful in our patient, however with prior knowledge of the MRI finding. EUS can then be used to mark the lesion preoperatively [21]. Another case report describes preoperative injection of the adenoma with ink for better intraoperative visualization [22]. The black tattooed nodule greatly facilitated the resection but requires wider exploration of the defined region. In our case, an alternative approach was chosen. Since preoperative EUS was able to localize the adenoma, it was decided to inject 99mTc-HSA directly into the nodule to allow for gamma-probe guided surgery.
The procedure was easy to perform and could be limited to a minimum surgical trauma. Identification of the lesion was feasible without extensive surgical exploration of the retroesophageal region, and removal of the labelled mass could be confirmed ex situ. Although the lesion was located almost 6 cm away from the incision line, only a small access was necessary. Due to this guided approach, the postoperative course was favourable and the patient did not present any complications. To our best knowledge, the present case is the first report of EUS-guided injection of a radioactive tracer (99mTc-HSA) into a retroesophageal parathyroid adenoma. The limitation of this case report is based on the restricted generalizability for easily accessible adenomas. However, using preoperative EUS-guided labeling in retroesophageally located tumors may be helpful to the surgeon by making surgical excision more precise and less invasive, which is of particular importance in high-risk regions that are difficult to reach. It might further serve as a good example of how multidisciplinary collaboration (nuclear medicine, gastroenterology and surgery) can contribute to the best possible patient care.
Conflicts of Interest
None.
Funding
This work was funded by Stiftung Chirurgie Technical University of Munich.
Author Contributions
All authors contributed to the study conception and design. The endoscopic labeling was performed by Mohamed Abdelhafez and Klemens Scheidhauer. Surgical removal of the adenoma was performed by Dirk Wilhelm and Ruediger Goess. The first draft of the manuscript was written by Christian Stöss, Ruediger Goess, Jonas Fuchtmann, Helmut Friess, Dirk Wilhelm, Klemens Scheidhauer and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Ethical Approval
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Article Info
Article Type
Case ReportPublication history
Received: Mon 20, Jun 2022Accepted: Wed 13, Jul 2022
Published: Tue 26, Jul 2022
Copyright
© 2023 Christian Stöss. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2022.01.03
Author Info
Christian Stöss Ruediger Goess Jonas Fuchtmann Mohamed Abdelhafez Helmut Friess Klemens Scheidhauer Dirk Wilhelm
Corresponding Author
Christian StössDepartment of Surgery, Technical University of Munich, School of Medicine, Munich, Germany
Figures & Tables
References
1.
Marcocci
C, Cetani F (2011) Clinical practice. Primary hyperparathyroidism. N Engl J
Med 365: 2389-2397. [Crossref]
2.
Weber
AL, Randolph G, Aksoy FG (2000) The thyroid and parathyroid glands. CT and MR
imaging and correlation with pathology and clinical findings. Radiol Clin
North Am 38: 1105-1029. [Crossref]
3.
Phitayakorn
R, McHenry CR (2006) Incidence and location of ectopic abnormal parathyroid
glands. Am J Surg 191: 418-423. [Crossref]
4.
Levin
KE, Clark OH (1989) The reasons for failure in parathyroid operations. Arch
Surg 124: 911-914. [Crossref]
5.
Judenhofer
MS, Wehrl HF, Newport DF, Catana C, Siegel SB et al. (2008) Simultaneous
PET-MRI: a new approach for functional and morphological imaging. Nat Med
14: 459-465. [Crossref]
6.
Bailey
DL, Barthel H, Beyer T, Boellaard R, Gückel B et al. (2013) Summary report of
the First International Workshop on PET/MR imaging, March 19-23, 2012,
Tubingen, Germany. Mol Imaging Biol 15: 361-371. [Crossref]
7.
Demirkurek
CH, Adalet I, Terzioglu T, Ozarmagan S, Bozbora A et al. (2003) Efficiency of
gamma probe and dual-phase Tc-99m sestamibi scintigraphy in surgery for
patients with primary hyperparathyroidism. Clin Nucl Med 28: 186-191. [Crossref]
8.
Udelsman
R, Lin Z, Donovan P (2011) The superiority of minimally invasive
parathyroidectomy based on 1650 consecutive patients with primary
hyperparathyroidism. Ann Surg 253: 585-591. [Crossref]
9.
Rubello
D, Casara D, Giannini S, Piotto A, De Carlo E et al. (2003) Importance of
radio-guided minimally invasive parathyroidectomy using hand-held gamma probe
and low (99m)Tc-MIBI dose. Technical considerations and long-term clinical
results. Q J Nucl Med 47: 129-138. [Crossref]
10.
Fraker
DL, Doppman JL, Shawker TH, Marx SJ, Spiegel AM et al. (1990) Undescended
parathyroid adenoma: an important etiology for failed operations for primary
hyperparathyroidism. World J Surg 14: 342-348. [Crossref]
11.
Agha
RA, Fowler AJ, Saeta A, Barai I, Rajmohan S et al. (2016) The SCARE Statement:
Consensus-based surgical case report guidelines. Int J Surg 34: 180-186.
[Crossref]
12.
Bilezikian
JP, Silverberg SJ (2000) Clinical spectrum of primary hyperparathyroidism. Rev
Endocr Metab Disord 1: 237-245. [Crossref]
13.
Adami
S, Marcocci C, Gatti D (2002) Epidemiology of primary hyperparathyroidism in
Europe. J Bone Miner Res 17: 18-23. [Crossref]
14.
Melton
LJ (2002) The epidemiology of primary hyperparathyroidism in North America. J
Bone Miner Res 17: N12-N17. [Crossref]
15.
Rubin
MR, Bilezikian JP, McMahon DJ, Jacobs T, Shane E et al. (2008) The natural
history of primary hyperparathyroidism with or without parathyroid surgery
after 15 years. J Clin Endocrinol Metab 93: 3462-3470. [Crossref]
16.
(1991)
Proceedings of the NIH Consensus Development Conference on diagnosis and
management of asymptomatic primary hyperparathyroidism. Bethesda, Maryland,
October 29-31, 1990. J Bone Miner Res 6: S1-S166. [Crossref]
17.
Bilezikian
JP, Brandi ML, Eastell R, Silverberg SJ, Udelsman R et al. (2014) Guidelines
for the management of asymptomatic primary hyperparathyroidism: summary
statement from the Fourth International Workshop. J Clin Endocrinol Metab
99: 3561-3569. [Crossref]
18.
Taterra
D, Wong LM, Vikse J, Sanna B, Pękala P et al. (2019) The prevalence and anatomy
of parathyroid glands: a meta-analysis with implications for parathyroid
surgery. Langenbecks Arch Surg 404: 63-70. [Crossref]
19.
Purz
S, Kluge R, Barthel H, Steinert F, Stumpp P et al. (2013) Visualization of
ectopic parathyroid adenomas. N Engl J Med 369: 2067-2079. [Crossref]
20.
Huber
GF, Hüllner M, Schmid C, Brunner A, Sah B et al. (2018) Benefit of 18
F-fluorocholine PET imaging in parathyroid surgery. Eur Radiol 28:
2700-2707. [Crossref]
21. Graff-Baker A, Roman SA, Boffa D, Aslanian H, Sosa JA (2009) Diagnosis of ectopic middle mediastinal parathyroid adenoma using endoscopic ultrasonography-guided fine-needle aspiration with real-time rapid parathyroid hormone assay. J Am Coll Surg 209: e1-e4. [Crossref]
22. Carrara S, Cozzaglio L, Jovani M, Pepe G, Bonifacio C et al. (2014) Endoscopic ultrasound-guided tattooing of a retroesophageal parathyroid adenoma. Endoscopy 46: E496-E497. [Crossref]
