Journals
Influence of Luting Material types on the Microleakage and Retention of Pressable Ceramic Crowns Cemented to Zirconia Implant Abutments
A B S T R A C T
Objective: To compare microleakage and retention of all-ceramic crowns cemented to zirconia implant abutments using three different luting agents.
Material and Methods: 42 internal hex zirconia abutments were assembled on 42 Implant Directs Legacy then lithium disilicate ceramic crowns with overhanging margins were fabricated and cemented to their corresponding assembly. All specimens were stored in water at 37°C for 24 hours then subjected to 3500 thermocycling. The all-ceramic crowns were pulled off to accomplish the retention test. The microleakage between all crowns and zirconia abutments was measured after immersed in 2% basic red fuchsine dye then were assessed using binocular stereomicroscope at each margin.
Results: Descriptive statistics showed that the highest mean value retentive strength of Rely-x cement (383.44±19.69 N), then Ketac-Cem (130.57±9.37N) and lowest mean value of Temp-Bond luting cement was (74.67±9.57 N). Rely-x demonstrated the least microleakage while Tembond was the worst microleakage value.
Conclusion: Resin modified glass ionomer Rely-x demonstrated the highest mean retentive strength. Resin modified glass ionomer Rely-x had the best sealing properties. The temporary cements Tempbond NE showed more microleakage than those Rely-x and Ketac-Cem.
I N T R O D U C T I O N
ONatural appearance of replaced single missing tooth in the anterior maxilla is one of the most challenging goals in dentistry. To achieve optimal esthetics, it has been suggested to restore single-tooth implants with all-ceramic abutment-crown combination. Bluish appearance of the cervical soft tissues as encountered with metal abutments can be avoided and light transmission is facilitated when using all-ceramic abutments [1].
Dental implants are an effective and popular option for replacing missing teeth, and they also form an important part of mainstream restorative dentistry today. Due to their good long-term outcome, implant-supported single crowns have become a preferred choice of many clinicians for the treatment of single edentulism in esthetic zones [2].
Today the continued high rate of success achieved with osseointegration allows a greater number of patients to enjoy the benefits of fixed supported restorations rather than removable restorations [3]. The use of single-tooth implants is considered a viable treatment option for single-tooth replacement. They are often recommended because preparation of adjacent teeth is avoided, the ideal replacement in spaced dentition, highly predictable, require little maintenance, and they preserve ridge height and width [4].
A currently popular material for fabrication of implant abutments is zirconia which is 3-yttria stabilized zirconia polycrystals (3Y-TZP). It is a white ceramic with physical properties very different from titanium. Zirconia is stronger, harder, and potentially more abrasive than titanium. Commercially pure titanium (Grade four) has a strength value of 550 MPa, while zirconia has shown strengths greater than 1000 MPa [5].
Some zirconia abutments utilize a titanium interface which attaches the implant and abutment through a titanium to titanium connection. Other zirconia abutments are a one-piece design which creates a zirconia to titanium interface. The variation of physical properties of these two materials may set up a mechanism for wear at the implant-abutment interface [6].
All-ceramic crowns are the most esthetically pleasing prosthodontic restorations. They can resemble natural tooth structure in terms of color and translucency because there is no metal to block light transmission [3]. Microleakage is defined as the passage of fluids, bacteria, molecules or ions between a restorative material and a tooth structure. The ingress of fluids and microorganisms may lead to staining at the restoration-tooth interface, pulpal irritation and in the long term, dissolution of the cement and development of secondary caries [7].
Microleakage prevented ideally by a luting agent. This leakage between implant abutments and the restoration results in the growth of bacteria. When examining the bacterial colonization found in conjunction with implant-supported restorations some authors noted that this colonization had a role in the growth of bacteria within the internal aspect of the implant [8].
Crown retention is a very important factor in the success of fixed restorations. The necessity for retention and the resistance of cement-retained restorations are related to the geometry of the abutment preparation, surface area, abutment height, surface roughness, and cementing medium [9].
The clinical success of fixed prostheses is highly dependent on the cementation procedure. An ideal adhesive should provide a durable bond between dissimilar materials, possess favorable compressive and tensile strengths, have sufficient fracture toughness to prevent dislodgment as a result of interfacial or cohesive failures, be able to wet the tooth and the restoration, exhibit adequate film thickness and viscosity to ensure complete seating, be resistant to disintegration in the oral fluids, be tissue compatible and demonstrate adequate working and setting time [7].
Materials and methods
Forty-two internal hex zirconia abutments were placed on 42 Implant Directs Legacy implants with titanium screws and torqued according to the manufacture’s recommendation.
The specimens were divided into two equal groups (N = 21) each, relative to the proposed test either retention or microleakage test, then each group was further subdivided into three equal subgroups (N= 7) according to the type of luting agent used for cementation of the crowns to their corresponding abutments as follows: Group RX: using Rely X Luting material, Group KC: using Ketac-Cem, and Group TB: using Tem-Bond Non Eugenol.
The implants were mounted in plastic rings with their coronal parts upwards using an autopolymerizing acrylic resin. The special jig device was used for specimen centralization in the plastic ring (Fig.1, 2).
A low viscosity hydro compatible condensation silicone was used to fabricate index on acrylic pattern of the first specimen (GC America INC, ALSIP, IL 60803, Japan) with overhanging margin on zirconia implant abutment then impression taking as index which used to prepare standardized wax patterns with the same dimensions for the rest of the specimens.
Forty-two crown wax patterns were fabricated by duplication of the acrylic patterns with silicone. The wax patterns were sprued and invested with a speed investment material (Fig. 3).
After the burn out of the wax analogue a lithium-disilicate glass-ceramic (IPS e.max) ingot was heated (917 °C) and pressed into the investment mold in the furnace following manufacturer’s recommendation.
After divestment with glass polishing beads at 4 bar pressures, fine divestment was carried out with glass polishing beads at 2 bar pressures. The pressed specimens were immersed into 1% hydrofluoric acid solution and cleaned in an ultrasonic cleaner for 15 min. Subsequently, each specimen was cleaned under running water and blow dry. Sprues were cut with a diamond disk. The white reaction layer was removed carefully using aluminum oxide at 2 bar pressures. Glazing was done according to manufacturer’s recommendation at 800°C. All finished crowns were examined using visual and tactile methods to ensure that the fit was acceptable.
All ceramic crowns were cleaned with water, and then dried with gentle air flow. Each type of the tested cement was mixed according to manufacture recommendations, recommendations, and then applied into the fitting surface of each crown, then the crowns were fixed to their corresponding abutments using special loading device under a constant seating pressure of 3.0kg that was maintained for 10 minutes [10]. Each crown was held in place while any excess cement remaining at the margins was removed carefully with a disposable brush (Fig.4).
All specimens were stored in water at 37 ˚C for 24 hours. They were subjected to thermocycling between 5 and 55 ˚C for total of 3000 cycles with a dwell time of 30 seconds and transfer time 5 seconds.
Twenty-one all-ceramic crowns were constructed with overhanging margins circumferentially from which the crowns were pulled up to accomplish the retention test; a longitudinally cylindrical steel tube (10 cm long) was reassembled using two steel screws [11]. The lower end of the tube was designed to accommodate the overhanging margins of the cemented ceramic crowns.
The upper end of the tube was designed to be attached to the moving jig of the universal testing machine (Lloyd Instruments LTD, West Fareham, UK) (Fig.5).
Each cemented specimen was fixed to the table of the testing machine, and debonding force was determined. (Fig.6) Cemented crowns were pulled off along the path of insertion with a crosshead speed of 10 mm/min, and the maximum force to debond each crown was considered as retentive strength. Maximum pull-out force of the jig of the universal testing machine was set to 2000 N.Statistical analysis was performed using Statistical Package for Social Sciences (SPSS).The other twenty-one specimens were coated with nail varnish and immersed in 2.0% basic red fuchsine dye solution for 24 hours at room temperature.All specimens were sectioned inciso-gingival by using carborandum disc and then assessed under magnification using binocular stereomicroscope at each margin. A total of twenty one readings were available for evaluation of microleakage between all-ceramic crown (e-max press) and zirconia implant abutments.
Specimens were assessed at each margin using the following five-point scale:
|
Score |
Description |
|
0 |
No dye penetration |
|
1 |
Dye penetration along the gingival wall |
|
2 |
Dye penetration up to ½ the axial wall |
|
3 |
Dye penetration along more than half to the full length of the axial wall |
|
4 |
Dye penetration extending to the occlusal surface |
Statistical analysis
The collected data were tabulated and statistically analyzed. Special tests were used to identify significant relationship between different variant in this study.
Statistical test used were: Statistical Package for Social Sciences (SPSS). Median (range), mann-whitney, kruskal-wallis Non-parametric test.
Tables
Table 1: Comparison of retention means values and standard deviation among different groups
|
Type of the cement |
No |
Mean |
SD |
ANOVA p value |
|
Rely x luting cement |
7 |
1.1 |
0.43 |
0.25 |
|
Ketaccem cement |
7 |
1.14 |
0.69 |
|
|
Tempbond cement |
7 |
1.71 |
0.76 |
Similar letter showing significant difference
Table 2: Comparison of microleakage mean values and standard deviation among different groups
|
Type of the cement |
No |
Mean |
SD |
ANOVA p value |
|
Rely x luting cement |
7 |
383.44ab |
19.69 |
<0.001 |
|
Ketaccem cement |
7 |
130.57ac |
9.37 |
|
|
Tempbond cement |
7 |
74.67bc |
9.57 |
Figure 1: Diagram and photograph for the specially designed jig used for implant fixtures centralization
Figure 2: Implant & zirconia abutment fixed in centralized position in plastic ring
Figure 3: Preparation of wax patterns for investing
Figure 4: Cemented ceramic crown
Figure 5: Specially designed attachment for retentive strength measurement, A; Upper part, B; Lower part
Figure 6: Close-up view to specially designed attachment in universal testing machine
Figure 7: All-ceramic crown cemented with Rely-x luting cement. This specimen was given a score of 1. (The die penetrated along the gingival wall).
Figure 8: All-ceramic crown cemented with Ketac cem cement. This specimen was given a score of 2. (The die penetrated up to ½ the axial wall).
Figure 9: All-ceramic crown cemented with Tempbond NE cement. This specimen was given a score of 3. (The die penetrated along more than half to the full length of the axial wall).
R e s u l t s
Analytical statistics
In the statistical comparison between the different groups, the significance of difference was tested using ANOVA (analysis of variance) to compare between more than two groups of numerical (parametric) data followed by post-hoc tukey for multiple comparisons. A P value < 0.05 was considered statistically significant. And a P value < 0.0001 was considered highly significant in all analyses.
Retention Results
Descriptive statistics showed that the highest mean value retentive strength of Rely-x cement (383.44±19.69 N), then Ketac-Cem (130.57 ± 9.37N) and lowest mean value of Temp-Bond luting cement was (74.67±9.57 N). (Table 1)
Microleakage results
All specimens of this group (21 zirconia implant abutments with all ceramic crowns) were subdivided into three equal subgroups according to different cements. Data were statistically analyzed by using Statistical Package for Social Sciences (SPSS). Descriptive statistics of microleakage results showed that the mean value of Rely-x cement was the least microleakage (1.1±0.43), then Ketac-Cem cement (1.14±0.69) and highest mean value of Temp-Bond NE cement (1.71±0.76) (Table 2), (Fig. 7, 8, 9, 10).
D i s c u s s i o n
The high success rates of dental implant and implant supported prostheses make the dental implant as a reliable alternative to conventional fixed dental prostheses which gives several options for treatment of edentulous areas. Implant-supported prostheses using titanium abutments sometimes give the gingiva an unnatural bluish at the cervical neck even when placed sub gingivally [12]. To overcome this problem, the use of ceramic abutments for implant supported restorations was suggested [13].
Recently, heat-pressed all-ceramic materials that contain lithium disilicate as a major crystalline phase have become available. One such system is IPS e.max Press, heat-pressed between 890 and 1120 ˚C, with which single crowns can be fabricated for both the anterior and posterior region of the mouth [14].
The use of titanium implant
Since the introduction of osseointegration, new alternatives of prosthetic treatment were available to patients based on the placement of endosseous titanium implants in edentulous areas, there placement of missing teeth by means of implants has become a predictable treatment modality for both complete and partial edentulous patients, ten-years surveys of fixed prostheses on natural teeth reveal a survival rate of approximately 75%, in contrast, success rates for endosseous implants have been shown to be greater than 90% [15].
Titanium implants were used because of its high success and survival rate due to their superior biocompatibility, corrosion resistance and specific strength compared with other metallic implant materials [10].
The use of zirconia abutments
Zirconia is a crystalline dioxide of zirconium. Its mechanical properties are very similar to those of metals and its color is similar to tooth color [16]. It is used as alternative to metallic abutments because of their optical properties. This type of restoration provides esthetic advantages especially in the visible anterior region. This is mainly due to the white color of the abutments which may avoid gray shadows or even a metal-colored part that emerges from the gingiva [17].
Zirconia abutments offer sufficient stability to support implant-supported single-tooth reconstructions in incisor and premolar locations, healthy mucosal conditions and stable marginal bone levels documented at zirconia abutments indicated a favorable soft and hard tissue reaction toward this ceramic material [18].
The use of acrylic resin for models
Acrylic based resins consist of polymeric materials based on polymethylmethacrylate. These dental materials are the result of a free radical polymerization reaction. They can be classified as chemical, heat or light activated depending on the factor that initiates the reaction. Chemical or autopolymerized materials involve a chemical activator like N, N-dimethyl p-toluidine. For heat-polymerizing materials, heat can be generated by hot water bath or microwave energy, while the light polymerizing uses visible light as energy source [19].
Fabrication of ceramic crown
In the present study, all crowns were fabricated from IPS e.max press. It consists of a lithium-disilicate pressed glass ceramic. It is considered the material of choice for the restorations in anterior teeth due to the favorable esthetic outcome [20].
Single-unit all-ceramic IPS e.max Press (Ivoclar Vivadent,Schaan, Liechtenstein) crowns were fabricated using the lost wax technique and by pressure injection of ceramic ingots (Ivoclar Vivadent) following the manufacturer’srecommendations [14].
IPS e.max crowns were fabricated by staining technique with no layering or veneering material applied to the crown for eliminating co-factors which may affect the purpose of the study [21].
The use of cements (Rely x, Ketac cem, Tempbond)
This study examined cement failure load and marginal leakage of all ceramic crowns cemented to implant-retained abutments. In each case, the cement failure was adhesive in nature and occurred at the abutment interface. Thus, marginal leakage was measured by examining the amount of stain penetration along the cement at the abutment interface.
Although variations exist in the quantity of retention provided by the same types of cements used with different implant systems and under different in vitro conditions. A multitude of factors in the oral environment including temperature changes such as thermocycling, occlusal forces affect the properties and retention of dental cements [22]. The retention of all-ceramic crowns cemented to prepared zirconia implant abutment was affected by the type of luting cement.
Various cements differ in their ability to provide resistance to microleakage. Some causes of leakage related to crowns include shrinkage of the cement on setting, lack of adhesion of the cement, cement solubility and mechanical failure of the cement. Examination of the leakage characteristics of a restorative material in vitro requires thermal-cycling to mimic temperature extremes found in the oral cavity. In the case of a cemented-crown restoration, the expansion and contraction of the restorative materials in response to thermal-cycling subjects the cement to mechanical stress. This effect of thermal cycling on marginal leakage has been found to be contingent upon the thermal conductivity and coefficients of thermal expansion of the materials used [23].
In this study, specimens were kept in the wet medium to imitate the events occurring in the mouth environment and then they were subjected to thermal cycle with a pre-determined program.
In this study the retentive strength of Ketac-Cem was nearly half the value of the Rely x (resin modified glass ionomer cement) this result is in agreement with Ernst et al. (2005).[14] Also who concluded that the results of this study showed that retentive strength of Temp-Bond NE was nearly less than three times value of the Rely-x this result is in agreement with Camaggio et al. (2012) [24].
This study was carried out with dyes which considered stricter than those carried out in the oral cavity. This is probably due to many reasons, such as:
- The dye is more easily diffused than bacteria and their byproducts,
- The build-up of proteins and debris that then calcify in the marginal gap may improve the seal.
- The dentinal fluid in vital teeth, which has a positive pressure, and the settling of fibrinogen inside the sectioned tubules may contrast molecular penetration [25].
Resin-modified glass ionomer cement (Rely-x) exhibited less microleakage scores than Ketac-Cem this result is in agreement with Zmener et al. (2013) who found that there were no statistically significant differences among resin-modified glass ionomer and glass ionomer cement [26].
Results of this study showed that Rely-x cement provided less microleakage than Ketac-Cem. But the result is in disagreement with Bhatnagar et al. (2007) who reported that within limitations of this in vitro study, Keatac-Cem showed less microleakage than Rely-x cement [27].
In the present study Tembond NE cement showed more microleakage according scores of five-point scale in which dye was penetrated along more than half to the full length of the axial wall (score 3) this result is in agreement with Duymus et al. (2005) who reported that both Temp-bond with and without eugenoul showed high microleakage [25].
Microleakage and marginal gaps are the important causes of fixed restoration failures. The amount of cement exposed to oral fluids, which depends on the marginal gap, may be related to cement dissolution. Cement dissolution can promote microleakage, but other causes such as mechanical properties of luting cement and adhesion between cement and tooth structure are involved [25].
Conclusions
Within the limitation of this in-vitro study the following conclusion were drawn:
- Specimens of glass ionomer cement demonstrated significantly higher mean retentive strength values than Temporary cement.
- Resin modified glass ionomer demonstrated the highest mean retentive strength and was significantly different from glass ionomer and temporary luting cement.
- All of the tested materials demonstrated different degrees of microleakage.
- Resin modified glass ionomer had the best sealing properties.
- The tested temporary cement showed more microleakage than other cements
Article Info
Article Type
Research ArticlePublication history
Received: Wed 14, Mar 2018Accepted: Sat 24, Mar 2018
Published: Fri 27, Apr 2018
Copyright
© 2023 Shaimaa Ahmed Abo-Elfarag. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOCR.2018.10.005
Author Info
Mohammed Hamed Ghazy Shaban Mohammed Takerza Shaimaa Ahmed Abo-Elfarag
Corresponding Author
Shaimaa Ahmed Abo-ElfaragB.D.S. Ms. PhD. Assistant Professor of Fixed Prosthodontics, Faculty of Dentistry, Mansoura University, Egypt
Figures & Tables
Table 1: Comparison of retention means values and standard deviation among different groups
|
Type of the cement |
No |
Mean |
SD |
ANOVA p value |
|
Rely x luting cement |
7 |
1.1 |
0.43 |
0.25 |
|
Ketaccem cement |
7 |
1.14 |
0.69 |
|
|
Tempbond cement |
7 |
1.71 |
0.76 |
Similar letter showing significant difference
Table 2: Comparison of microleakage mean values and standard deviation among different groups
|
Type of the cement |
No |
Mean |
SD |
ANOVA p value |
|
Rely x luting cement |
7 |
383.44ab |
19.69 |
<0.001 |
|
Ketaccem cement |
7 |
130.57ac |
9.37 |
|
|
Tempbond cement |
7 |
74.67bc |
9.57 |
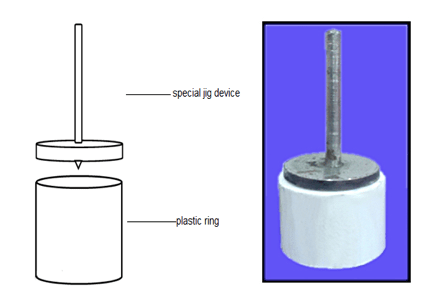

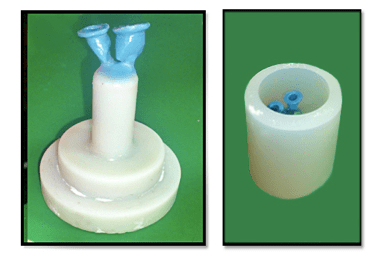

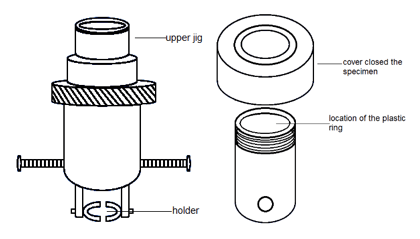




Figure legends
Fig. 1: Diagram and photograph for the specially designed jig used for implant fixtures centralization
Fig. 2: Implant & zirconia abutment fixed in centralized position in plastic ring
Fig. 3: Preparation of wax patterns for investing
Fig. 4: Cemented ceramic crown
Fig. 5: Specially designed attachment for retentive strength measurement, A; Upper part, B; Lower part
Fig. 6: Close-up view to specially designed attachment in universal testing machine
Fig. 7: All-ceramic crown cemented with Rely-x luting cement. This specimen was given a score of 1. (The die penetrated along the gingival wall).
Fig. 8: All-ceramic crown cemented with Ketac cem cement. This specimen was given a score of 2. (The die penetrated up to ½ the axial wall).
Fig. 9: All-ceramic crown cemented with Tempbond NE cement. This specimen was given a score of 3. (The die penetrated along more than half to the full length of the axial wall).
References
1. Butz F, Heydecke G, Okutan M, Strub JR (2005) Survival rate, fracture and failure mode of ceramic implant abutments after chewing simulation. J Oral Rehabil 32: 838-843. [Crossref]
2. Akin H, Guney U (2012) Effect of various surface treatments on the retention properties of titanium to implant restorative cement. J Lasers Med Sci 27: 1183-1187. [Crossref]
3. Rosenstial SF, Land MF, Fujimoto J (2006) Implant supported fixed prosthesis: contemporary fixed prosthetics (4th Edition). St Louis, Mosby, 323-610.
4. Vermylen K, Collart B, Linden UIF, De Bruyn H (2003) Patient satisfaction and quality of single-tooth restorations. J Clin Oral Implant Res 14: 119-124. [Crossref]
5. Aboushelib MN, Kleverlaan CJ, Feilzer AJ (2008) Evaluation of high fracture toughness composite ceramic for dental applications. J prosthodont 17:538-544. [Crossref]
6. Klotz MW Wear parameters of zirconia and titanium at implant-abutment interface. Master Thesis. University of Connecticut, New Jerses, USA 20l1-3.
7. Albert FE (2001) Marginal adaptation and micoleakage of procera all-ceramic copings. Master Thesis, University of Toronto, Otawa, Canada 1-60.
8. Ali AM (2010) Immediate and delayed micro-tensile bond strength of different luting resin cements to different regional dentin. University of mansoura, Egypt, Master thesis 28.
9. Albrektsson T (1993) On long-term maintenance of the osseointegrated response. Aust Prosthodont J 7: 15-24. [Crossref]
10. Niinomi M (1998) Mechanical properties of biomedical titanium alloys. Mater Sci Eng A 243: 231-236.
11. Abuo-madina M, Ozcan M, Dent M, Badawi MF (2010) Effect of surface conditioning and taper angle on the retention of IPS e.max press crowns. J prosthodont 19: 200-204. [Crossref]
12. Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. J Biomater 20: 1-25. [Crossref]
13. Bettencourt AF, Neves CB, de Almeida MS, Pinheiro LM, Oliveira SA, et al. (2010) Biodegradation of acrylic based resins. J Dent Mater 26: 173-177. [Crossref]
14. Ernst CP, Cohnen U, Stender E, Willershausen B (2005) In vitro retentive strength of zirconium oxide ceramic crowns using different luting agents. J Prosthet Dent 93: 551-558. [Crossref]
15. Tabata LF, Assuneao WG, Barao ARV, de Sousa EA, Gomes EA, et al. (2010) Implant platform switching:biomechanical approach using two-Dirnensional finite element analysis. J Craniofac Surg 21: 182-187. [Crossref]
16. Yucel M, Yondem I, Aykent F, Eraslan O (2012) Influence of the supporting die structures on the fracture strength of all-ceramic materials. Clin Oral Investig 16: 1105-1110. [Crossref]
17. Consani S, Santos JG, Sobrinho LC, Sinhoreti MAC, Sousa-Neto MD (2003) Effect of cement types on the tensile strength of metallic crowns submitted to thermo-cycling. Brazilian Dent J 14: 193-198. [Crossref]
18. Glauser R, Sailer I, Wohlwend A, Studer S, Schibli M, et al. (2004) Experimental Zirconia abutments for implant-supportedsingle-tooth restorations in aesthetically demandingregions: 4-years results of a prospective clinical study. J Int Prosthodont 17: 285-290. [Crossref]
19. Ergin S, Gemalmaz D (2002) Retentive properties of five different luting cements on base and noble metal copings. J prosthet Dent 88:491-497. [Crossref]
20. Piwowarczyk A, Lauer HC, Sorensen JA (2004) In vitro shear bond strength of cementing agents to fixed prosthodontic restorative materials. J prosthet Dent 92: 265-273. [Crossref]
21. Carnaggio TV, Conrad R, Engelmeier RL, Gerngross P, Paravina R, et al. (2012) Retention of CAD/CAM All-Ceramic Crowns on Prefabricated Implant Abutments: An In Vitro Comparative Study of Luting Agents and Abutment Surface Area. J Prosthodont 21: 523-528. [Crossref]
22. Dudley JE, Richards LC, Abbott JR (2008) Retention of cast crown copings cemented to implant abutments. J Australian Dent 53: 332-339. [Crossref]
23. Medic V, Djuricic KO, Dodic S, Petrovic R (2010) In vitro evaluation of microleakage of various types of dental cements. Srp Arh Celok Lek 138: 143-149. [Crossref]
24. Carnaggio TV, Conrad R, Engelmeier RL, Gerngross P, Paravina R, et al. (2012) Retention of CAD/CAM All-Ceramic Crowns on Prefabricated Implant Abutments: An In Vitro Comparative Study of Luting Agents and Abutment Surface Area. J Prosthodont 21: 523-528. [Crossref]
25. Duymus ZY, Yanikoglu ND, Bayindir F (2005) The investigation of the marginal microleakage of four temporary cements in metal casting. Ataturk University, school of dentistry, prosthodontic department, Erzurum, turkey 15: 22-18.
27. Zmener O, Pameijer CH, Rincon SM, Serrano SA, Chaves C (2013) Sealing properties of three luting agents used for complete cast crowns: a bacterial leakage study. Oper Dent 38: 11-20. [Crossref]
28. Bhatnagar V, Sardar C, Ram S, Mehta (2007) An evaluation of microleakage of metallic copings cemented with three luting agents: A stereomicroscopic in vitro study. J Indian Prosth Society 10: 25-34.
