Journals
Infectious Endocarditis in Sub-Saharan Africa: Epidemic-Clinical Aspects, Evolutionary and Prognostic: Multicentre Study on 81 Cases Followed Over 1 Year in Lomé (Togo)
A B S T R A C T
Introduction: Infectious endocarditis remains a relatively common, serious pathology and suffering heavy mortality in sub-Saharan Africa.
Purpose: The objective of this study was to describe the epidemic-clinical, evolutionary aspects patients hospitalized for infectious endocarditis and assess their prognosis.
Methods: This is a prospective, 5-year, multicentre study of 81 hospitalized patients and treated for infectious endocarditis. These patients were followed for at least a year.
Results: We observed that in our sub-Saharan context, patients who suffer from infectious endocarditis are often young, with an average age of 30 years. Rheumatic valve disease and congenital heart disease underlying the most frequent. Blood cultures are often negative, making it difficult the choice of appropriate antibiotic therapy. Surgical treatment (heart surgery) is difficult to access (2% in our study). As a result, the mortality is very high (63% at 1 year), with a survival rate of only 37% at 1 year.
Conclusion: Our study shows that despite progress in diagnosis and therapeutic management, infectious endocarditis remains a pathology serious with heavy mortality in sub-Saharan Africa. It is important to highlight the importance of prevention, early diagnosis of infectious endocarditis, and especially the need for early medical-surgical management of these patients to improve their prognosis.
Keywords
Infectious endocarditis, prognosis, sub-Saharan Africa
Introduction
Infectious endocarditis (AE) remains a serious disease, with an overall mortality of 20 to 30% in the West, despite advances in antibiotic therapy and surgery heart rate [1-13]. In sub-Saharan Africa, the low socio-economic level of patients, cultural context, diagnostic delay, antibiotic limits and difficult accessibility of cardiac surgery, make the prognosis of AE quite reserved with significantly higher mortality than in the West [14-20]. Very few African studies were devoted to the medium and long-term prognosis of AE. The objective of our study was therefore to assess the epidemic-clinical aspects and to evaluate the short and medium-term prognosis of hospitalized patients for infectious endocarditis in cardiology in Lomé.
Patients and Methods
It is a prospective, multicentric, longitudinal, descriptive study carried out in four hospitals in Lomé (Sylvanus Olympio University Hospital Centre, Centre Hospitalier Universitaire Campus, Polyclinique Internationale Saint Joseph, Cabinet médical Holy Spirit) from January 2015 to December 2019, a period of 5 years, covering patients hospitalized in Cardiology. We included all patients hospitalized, treated and followed up in cardiology for certain or probable infectious endocarditis, according to criteria Durack, Duke University [21]. The criteria for no inclusion were no confirmation of infectious endocarditis diagnosis, incomplete records and patients lost sight before 1 year of follow-up. During the 5 years of our study period, 92 patients were hospitalized on suspicion of infectious endocarditis, 11 patients did not fill the inclusion criteria. Eighty-one patients were selected for our study.
We collected epidemiological and clinical parameters: age, sex, origin geographic, economic profile, time between onset of febrile state and diagnosis. The data from the comprehensive physical examination emphasizing the cardiovascular system and the looking for the front door. Biologically, we studied: blood cultures, blood count, blood velocity sedimentation, C-reactive protein (normal less than 6 mg/l), fibrinaemia, and creatinine (normal 5 to 11 mg/dl) and creatinine clearance, examination urine cytobacteriology. At the electrocardiogram (ECG) we looked for rhythm disorders, conduction disorders, signs of cavity hypertrophy and repolarization disorders. At the Trans-thoracic Doppler echocardiography, we looked for the existence or not of lesions such as: vegetations, abscesses, perforations, rupture of ropes. We have also appreciated the echostructure of the valves, the dimensions of the cardiac cavities, the myocardial function, the pericardium and the existence of pulmonary arterial hypertension (PAH). From a therapeutic point of view, we insisted on antibiotic therapy by specifying the type antibiotic, dosage, duration and route of administration, and treatment of complications (medical treatment and cardiac surgery). The evolution was assessed on a stable or not apyrexia, the regression or not of the biological inflammatory syndrome, the regression of signs of heart failure, the negative or negative blood cultures, the occurrence of complications and death. After patients' hospital discharge, we tried to determine the overall evolution in ambulatory, assessing them in the third, sixth and twelfth months.
The data collected was captured and analysed using Epi Info 6.02 software. The continuous variables were expressed by the mean plus or minus the standard deviation. The student and khi two were made for comparisons between groups when these were appropriate and when the sample was too small or the distribution anomalous we used Mann Whitney’s test or Fisher’s exact test considering a significant difference where the p was less than or equal to 0,05.
Results
I Epidemic-Clinical Aspects
During our study period, we diagnosed 81 cases of endocarditis of a total of 6,248 patients hospitalized in Cardiology study. The hospital prevalence of infectious endocarditis was therefore 1.3%. Age average of patients was 30 years with extremes of 7 and 60 years. More than half of patients (54%, n=44) were under 30 years of age. Predominance was not sex ratio (sex ratio of 1.1). Socio-economic level of most patients was average. The average time between onset of febrile condition and diagnosis was 1 month (extremes 5 days to 2 months). The gateway was found in 40.7% of cases (n=33). Table 1 shows the clinical characteristics of inclusion patients. Blood cultures were positive only in 28.4% of cases (n=23).
Table 1: Patient Clinical Data.
|
|
Total |
Percentage % |
|
Fever |
77 |
95,1 |
|
Average Temperature |
38,5°c (38-40°) |
|
|
Altered condition |
72 |
88,9 |
|
History |
|
|
|
Recurring Sore throat/ Pharyngitis |
24 |
29,6 |
|
Polyarthralgia |
21 |
26 |
|
Known heart disease |
23 |
28,4 |
|
Previous antibiotics use |
63 |
77,8 |
|
Dyspnea |
62 |
76,5 |
|
CF average |
116 (86-156) |
|
|
Cardiac breath |
74 |
91,3 |
|
Skin symptoms |
8 |
9,9 |
|
Splenomegaly |
10 |
12,3 |
|
Heart failure |
69 |
85,2 |
|
Portes d’entrée |
33 |
40,7 |
|
Oral or dental |
11 |
13,6 |
|
Pulmonary |
7 |
8,6 |
|
Urinary |
5 |
6,2 |
|
Obstetrical |
5 |
6,2 |
|
Central venous catheter |
2 |
2,5 |
|
Pacemaker probe |
2 |
2,5 |
|
Cardiac surgery |
1 |
1,2 |
|
Average delay febrile-diagnostic condition 30 days (2-45 days) |
||
Table 2: Paraclinical Patient Data.
|
|
Effective |
Percentage% |
|
Blood Cultures |
81 |
|
|
Positives |
23 |
28,4 |
|
Negatives |
58 |
71,6 |
|
Hémogram |
81 |
|
|
Hyperleukocytosis |
72 |
88,9 |
|
Vs accélérée |
73 |
90,1 |
|
Cardiac Echodoppler |
81 |
|
|
Végétations |
81 |
100 |
|
Mitral |
41 |
50,6 |
|
Aort |
20 |
24,7 |
|
Mitral-aortic |
12 |
14,8 |
|
Tricuspid |
5 |
6,1 |
|
Pulmonary |
2 |
2,5 |
|
Abscess |
12 |
14,9 |
|
Rupture de cordages |
17 |
21 |
The ECG found among other anomalies, 10 cases of atrial fibrillation, 6 cases of atrial flutter, 20 cases of polymorphic ventricular extrasystoles, and 8 blocks of right branch complete. Cardiac ultrasound showed one or more vegetations in all patients. These vegetations were found in the left heart in 91% of cases (n=73) and in the right heart in 9% (n=7). They were voluminous in 39 patients (48.1%) and small in 42 patients (51.8%), pedi cultural and highly mobile in 37% of cases (n=30). Moderate pericardial effusion was found in 12 cases (14.8%). Underlying heart disease was found in 35 patients (43.2%). For these underlying heart diseases, rheumatic valve diseases (22.2%, n=18) were the most frequent, including 11 cases of Mitral Insufficiency (13.6%), 4 cases of aortic insufficiency (4.9%), and 3 cases of Mitral Disease (3.7%). Congenital heart disease ranked second (17.3%, n=14), of which Interventricular Communications (7.4%, n=6), Fallot Tetralogy (3.7%, n=3), Persistent Arterial Canal (3.7%, n=3), Pulmonary Stenosis (2.5%, n=2). Finally, 3 patients (3.7%) were carriers of mechanical valve prosthesis. However, In the majority of cases, endocarditis occurred on a seemingly healthy heart (56.8%, n=46). According to the modified DUKE classification endocarditis was certain in 60 patients (74%) and possible in 21 cases (26%) [21]. Table 2 shows paraclinical patent data.
II Therapeutic and Evolutionary Aspects
Antibiotic therapy was routinely administered in all patients by parenteral route, just after blood cultures. Bi-antibiotic therapy was administered in 75 cases (92.6%). The combination of an aminoglycoside (gentamycin) and a beta-lactam (Amoxicillin + clavulanic acid or ceftriaxone) was the most used. Ceftriaxone was the most commonly used antibiotic with 90.1% (n=73). It was administered intravenously, at a dose of 2 grams per day for adults. In patients with aminoglycoside contraindication, monotherapy with ceftriaxone was administered. Gentamycin was administered intravenously in 69 patients (85.2%) at a dose of 160 mg/d for adults and 5 mg/kg/day for children. Amoxicillin + clavulanic acid was prescribed in 9.9% of cases, intravenously. The daily intake was 6g in adults and 200 mg/kg in children. The average duration of the antibiotic treatment as a whole was 37.3 days with extremes of 1 day and 67 days. Treatment of the entrance doors was routine. Surgical indication was required in 58 patients (71%). But since cardiac surgery is difficult to access in Togo, only 13.8% of cases (n=8) after a medical evacuation abroad (Morocco and Europe). This involved resection of vegetations with valve plasticity in 2 patients (25%), valve replacement in 2 patients (25%), resection of vegetations followed by correction of congenital heart disease in 4 children (50%). The operational follow-up were simple with good clinical and hemodynamic evolution. The average length of hospitalization was 34.2 days (extremes of 2 and 62 days). During hospitalization the evolution was enamelled with several complications.
Cardiac complications were frequent, mainly heart failure in 84.5% of cases (n=68), pericardial effusion in 15% of cases (n=12), and complete atrial fibrillation tachyarrhythmia in 10 patients (12.3%). Vascular complications of septic arterial embolism of the lower limbs were observed in 5 patients (6.2%), with 2 cases of progression to gangrene requiring amputation of the limb. Neurological complications were observed in 9 patients (11.1%), including 7 cases (8.6%) ischaemic stroke and two stroke cases haemorrhagic (2.4%). Kidney complications were observed in 6 patients (7.4%). There were 4 cases (4.9 %) renal failure related to the renal toxicity of Gentamycin, and 2 cases (2.5%) of acute glomerulonephritis. Progression was favourable in 53 patients (65.5%) during hospitalization with regression clinical and biological signs under antibiotic treatment. No blood culture control had not returned positive.
III Prognosis
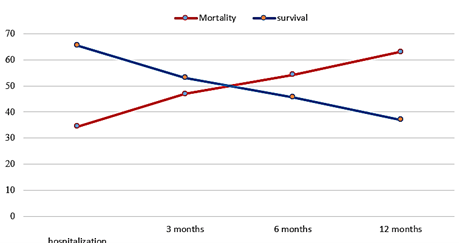
Intra-hospital mortality was 34.5%. Overall mortality at the end of a follow-up year was 63% (Table 3). The Figure 1 shows the evolution of mortality and survival over 12 months. In univariate analysis, poor prognosis factors were: heart failure, uncontrolled, persistent infectious syndrome, anemia, alteration of general condition, voluminous vegetations ( 10 mm) and valvulopathies rheumatic. (Table 4).
Table 3: Evolution of mortality and survival over 12 months.
|
|
Number of deaths |
Mortality |
Survival |
|
In Hospitalization |
28 |
34,5 |
65,5 |
|
After Hospitalization |
|
|
|
|
3 months |
38 |
46,9 |
53,1 |
|
6 months |
44 |
54,3 |
45,7 |
|
12 months |
51 |
63 |
37 |
Table 4: Prognosis factors evaluated in univariate analysis evaluated factors.
|
|
p-value |
|
Heart failure* |
0,002 |
|
General condition alteration* |
0,041 |
|
Anemia* |
0,003 |
|
Large vegetations ≥ 10 mm* |
0,023 |
|
Rheumatic valve disease* |
0, 043 |
|
Uncontrolled persistent infectious syndrome* |
0,042 |
|
Age |
0,847 |
|
Heart rhythm disorder |
0,623 |
|
Kidney failure |
0,341 |
|
Stroke/cerebrovascular accident |
0,426 |
Figure 1: Evolution of mortality and survival over 12 months.
Discussion
Our study included 81 patients hospitalized and treated for endocarditis in the cardiology departments of four medical facilities in Lomé 5-year period. In this work the hospital prevalence of infectious endocarditis was 1.3%. Patients with AE are young in Africa, while they are older in western series (mean age 30 vs 60-70) [1-20]. Clinical signs were dominated by the combination of fever + heart murmur. Blood cultures are often negative (71.6%). This high rate of negative blood cultures was also found in the most African series [14-20]. This can be explained in Africa by antibiotic therapy untimely, poor technical conditions for producing blood cultures (collection, storage and delivery of blood samples), lack of suitable culture media to isolate demanding or slow-growing germs. Indeed, in our study, 77.8% of patients had already taken antibiotics before arriving in cardiology, either on self-medication, or on unwanted medical prescription. However, in the Western series, previous antibiotic therapy is observed only around 20% of cases [2, 7, 8, 11, 12].
Microbiologically the germ most encountered in our study was Staphylococcus aureus, found in 52% of positive blood cultures. This predominance can be explained by the frequency of skin, urinary and gynaecological entrance doors. On the other hand, in developed countries, blood cultures are made under optimal conditions and consequently, are positive in 90-95% of cases and the germs most found are staphylococcus and streptococci. Staphylococci being predominant in iatrogenic entry doors [1-4, 7, 11-13, 22]. In our study, the predominant underlying heart diseases were: rheumatic valvulopathies and congenital heart disease, unlike in the country where endocarditis occurs most often on valve prosthesis, catheter and endocardiac probes, in drug users (right heart AE) and immunocompromised patients [1-4, 11-13].
However, we are seeing more and more in Africa, the decline of valvulopathies improved living conditions, improved access to antibiotic treatment in post-streptococcal angina. Nevertheless, this decline does not mean disappearance because these rheumatic heart diseases still continue to be the bed endocarditis. The predominance of mitral damage may be related to the greater frequency of these valvular lesions during rheumatic fever (AAR) [14-20]. In developed countries, aortic involvement is most common during endocarditis infection on acquired valve diseases, due in particular to the increase in incidence of degenerative aortic valve disease in the elderly congenital heart disease comes second to underlying heart disease in our study [1-13]. However, the scarcity of AEs on congenital heart disease was highlighted in several African series [14-20]. Probably because these studies were done in adult cardiology where congenital heart disease is less frequent. Stents on valve prostheses represent in our series only 3.7% AEs. However, it is a common form in Europe (12-35% of endocarditis infectious) [1-13]. This is one of the most frequent and serious complications of valve replacement surgery. In Africa their frequency is variable from 2-14.9% [14-17, 20]. This rate will likely increase in the future, with the development of open-heart surgery in several African countries.
The search for the entry gate must be systematic during infectious endocarditis. It was found in only 33 cases (40.7%) in our series. The oral entrance door was the most represented. The latter is common in most studies and shows once again the importance of oral hygiene [1-20]. In addition, in sub-Saharan Africa we are seeing more and more cases of care-related infectious endocarditis: central venous catheters, pacemaker probes, especially as interventional cardiology is emerging in some of our countries [14-16].
Ceftriaxone was the most commonly used antibiotic (90.1%). Empirical or probabilistic antibiotic therapy (before blood cultures) of first intention in our series was made especially by the association Ceftriaxone + Gentamycin. This is justified by the fact that this combination is simple (only one injection IV per day) and less expensive compared to the combination with Penicillin (high dose and in 2 or 3 doses per day). On this issue empirical antibiotic therapy, international recommendations have evolved significantly and are currently diverging between Europeans and Americans Europeans recommend (since 2015) the association Penicillin A (Ampicillin, 12 g/day) + Penicillin M (Cloxacillin or Oxacillin, 12 g/day) + Gentamycin (3 mg/kg/day), while this treatment was based on the combination Amoxicillin-clavulanate or Ampicillin-sulbactam (12 g/day) + Gentamycin (3 mg/kg/day) in the 2009 European Guidelines 2005 [8, 9, 12, 23]. On the other hand, recent US recommendations from 2015 argue for more individualized treatment based on patient characteristics and endocarditis scalability [11, 23].
Surgical treatment is the therapeutic method of choice for complications (hemodynamic, infectious, thromboembolic and mixed complications) not controlled by medical treatment [8-12]. In Europe, recent statistics have shown that 40-55% of patients with infectious endocarditis are operated on during the 8 acute period of the disease before the end of antibiotic therapy, with a better prognosis compared to medical treatment alone [8-12, 24]. In our study, only 8 patients (9.9% of all AEs) received surgical treatment abroad (in Europe), because cardiac surgery is not yet available in Togo, as is the case in most countries in sub-Saharan Africa. In addition, most patients were of a low socio-economic level, and have no health insurance to cover the costs heart surgery. With the help of the International Non-governmental Organization Men, 4 children with AEs on congenital heart disease were evacuated to Switzerland (CHUV Lausanne and University Hospitals of Geneva) for cardiac surgery.
He most common complication was heart failure (85.5%). Its presence was statistically related to the occurrence of death (p=0.0068), as demonstrated by several studies [8-12, 15, 24]. Kidney complications are a complication that can affect the life expectancy. The evolution can be made towards renal insufficiency whose mechanism is variable either by glomerulonephritis secondary to the presence of circulating immune complex, either by infarction and/or renal abscess or by gentamycin-related nephrotoxicity. Neurological complications (8.6% DALY) have was widely described in the literature [2, 11-13, 15]. In our work there was no statistically significant relationship between stroke occurrence and mortality (p=0.974).
Our study is one of the few in sub-Saharan Africa that has focused on becoming ill for up to a year. The prognosis was reserved, with a death rate of 34.5% in hospitalization, and 63% after one year of follow-up. The prognosis of IS better in developed countries with 16% and 30% hospital mortality on a one-year follow-up, due to the best conditions of care [2, 9-13]. In of developing countries, this high mortality can be explained by the diagnostic delay, the often-advanced evolutionary stage of underlying heart disease, the frequency of complications of AEs, low access to surgical treatment, level low-cost populations making it difficult to manage patients.
Conclusion
Infectious endocarditis is a relatively common pathology in sub-Saharan Africa, serious, with a reserved prognosis, very high mortality both in the short and medium term. Patients are usually young. Blood cultures are often negative, making echocardiography the key to diagnosis. Staphylococci are increasingly the germs involved. The underlying heart diseases are mainly rheumatic valve diseases and congenital heart diseases. Our study shows that the management of infectious endocarditis poses, nowadays several problems related to diagnostic delay, high frequency of negative blood cultures, low level the socio-economic costs of patients, the high cost of treatment and the very limited cardiac surgery. As a result, mortality is very high, with a survival rate only 37% at one year. Hence the value of AR prevention, early diagnosis and especially early medico-surgical management of these patients to improve their prognosis.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 27, Aug 2020Accepted: Sat 12, Sep 2020
Published: Mon 19, Oct 2020
Copyright
© 2023 Baragou Soodougoua. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2020.05.08
Author Info
Baragou Soodougoua S Pessinaba MF Simwetare EN Oloude-Kakpovi P Dossim
Corresponding Author
Baragou SoodougouaCardiology Department, Sylvanus Olympio, University Hospital Centre, Lomé, Togo
Figures & Tables
Table 1: Patient Clinical Data.
|
|
Total |
Percentage % |
|
Fever |
77 |
95,1 |
|
Average Temperature |
38,5°c (38-40°) |
|
|
Altered condition |
72 |
88,9 |
|
History |
|
|
|
Recurring Sore throat/ Pharyngitis |
24 |
29,6 |
|
Polyarthralgia |
21 |
26 |
|
Known heart disease |
23 |
28,4 |
|
Previous antibiotics use |
63 |
77,8 |
|
Dyspnea |
62 |
76,5 |
|
CF average |
116 (86-156) |
|
|
Cardiac breath |
74 |
91,3 |
|
Skin symptoms |
8 |
9,9 |
|
Splenomegaly |
10 |
12,3 |
|
Heart failure |
69 |
85,2 |
|
Portes d’entrée |
33 |
40,7 |
|
Oral or dental |
11 |
13,6 |
|
Pulmonary |
7 |
8,6 |
|
Urinary |
5 |
6,2 |
|
Obstetrical |
5 |
6,2 |
|
Central venous catheter |
2 |
2,5 |
|
Pacemaker probe |
2 |
2,5 |
|
Cardiac surgery |
1 |
1,2 |
|
Average delay febrile-diagnostic condition 30 days (2-45 days) |
||
Table 2: Paraclinical Patient Data.
|
|
Effective |
Percentage% |
|
Blood Cultures |
81 |
|
|
Positives |
23 |
28,4 |
|
Negatives |
58 |
71,6 |
|
Hémogram |
81 |
|
|
Hyperleukocytosis |
72 |
88,9 |
|
Vs accélérée |
73 |
90,1 |
|
Cardiac Echodoppler |
81 |
|
|
Végétations |
81 |
100 |
|
Mitral |
41 |
50,6 |
|
Aort |
20 |
24,7 |
|
Mitral-aortic |
12 |
14,8 |
|
Tricuspid |
5 |
6,1 |
|
Pulmonary |
2 |
2,5 |
|
Abscess |
12 |
14,9 |
|
Rupture de cordages |
17 |
21 |
Table 3: Evolution of mortality and survival over 12 months.
|
|
Number of deaths |
Mortality |
Survival |
|
In Hospitalization |
28 |
34,5 |
65,5 |
|
After Hospitalization |
|
|
|
|
3 months |
38 |
46,9 |
53,1 |
|
6 months |
44 |
54,3 |
45,7 |
|
12 months |
51 |
63 |
37 |
Table 4: Prognosis factors evaluated in univariate analysis evaluated factors.
|
|
p-value |
|
Heart failure* |
0,002 |
|
General condition alteration* |
0,041 |
|
Anemia* |
0,003 |
|
Large vegetations ≥ 10 mm* |
0,023 |
|
Rheumatic valve disease* |
0, 043 |
|
Uncontrolled persistent infectious syndrome* |
0,042 |
|
Age |
0,847 |
|
Heart rhythm disorder |
0,623 |
|
Kidney failure |
0,341 |
|
Stroke/cerebrovascular accident |
0,426 |
References
- Hoen B (2001) Nouvelles caractéristiques de l’endocardite infectieuse en France: résultats de l’enquête multirégionale 1999. Médecine et Maladies Infectieuses 31: 411-445.
- Capilla E, Poyet R, Tortat A V, Marchi J, Brocq F X et al. (2016) Endocardite infectieuse: caractéristiques cliniques et pronostic entre 2004 et 2014 dans un hôpital non universitaire. Ann Cardiol Angéiol.
- David R Murdoch, G Ralph Corey, Bruno Hoen, José M Miró, Vance G Fowler Jr et al. (2009) Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med 169: 463-473. [Crossref]
- Bruno Hoen, François Alla, Christine Selton Suty, Isabelle Béguinot, Anne Bouvet (2002) Changing profile of infective endocarditis: results of a 1-year survey in France. JAMA 288: 75-81. [Crossref]
- G D Birmingham, P S Rahko, F Ballantyne 3rd (1992) Improved detection of infective endocarditis with transesophageal echocardiography. Am Heart J 123: 774-781. [Crossref]
- R Erbel, S Rohmann, M Drexler, S Mohr Kahaly, C D Gerharz et al. (1988) Improved diagnostic value of echocardiography in patients with infective endocarditis by transoesophageal approach. A prospective study. A prospective study. Eur Heart J 9: 43-53. [Crossref]
- Dieter Horstkotte, Ferenc Follath, Erno Gutschik, Maria Lengyel, Ali Oto et al. (2004) Guidelines on Prevention, Diagnosis and Treatment of Infective Endocarditis Executive Summary. The Task Force on Infective of the European Society of Cardiology. Eur Heart J 25: 267-276. [Crossref]
- Larry M Baddour, Walter R Wilson, Arnold S Bayer, Vance G Fowler Jr, Ann F Bolger et al. (2005) Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation 111: e394-4e34. [Crossref]
- Gilbert Habib, Bruno Hoen, Pilar Tornos, Franck Thuny, Bernard Prendergast et al. (2009) Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur Heart J 30: 2369-2413. [Crossref]
- Tin Han Htwe, Nancy Misri Khardori (2012) Cardiac Emergencies. Infective Endocarditis, Pericarditis, and Myocarditis. Med Clin North Am 96: 1149-1169. [Crossref]
- Larry M Baddour, Walter R Wilson, Arnold S Bayer, Vance G Fowler Jr, Imad M Tleyjeh et al. (2015) Infective endocarditis in adults: diagnosis, antimicrobial therapy and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation 132: 1435-1486. [Crossref]
- Gilbert Habib, Patrizio Lancellotti, Manuel J Antunes, Maria Grazia Bongiorni, Jean Paul Casalta et al. (2015) 2015 ESC Guidelines for the management of infective endocarditis: the Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC), Endorsed by: European 10 Association of Cardio-thoracic Surgery (EACTS), The European Association of nuclear medicine (EANM). Eur Heart J 36: 3075-3128. [Crossref]
- Ana Revilla, Javier López, Isidre Vilacosta, Eduardo Villacorta, María J Rollán I et al. (2007) Clinical and prognostic profile of patients with infective endocarditis who need urgent surgery. Eur Heart J 28: 65-71. [Crossref]
- Benson Njuguna, Adrian Gardner, Rakhi Karwa, François Delahaye (2017) Infective Endocarditis in Low-and Middle-Income Countries. Cardiol Clin 35: 153-163. [Crossref]
- Hassine M, Mlayeh D, Ben Massoud M, Mahjoub M, Tahar M et al. (2016) Endocardite infectieuse compliquée d’insuffisance cardiaque. Ann Cardiol Angeiol (Paris).
- Mouhamadou Bamba Ndiaye, Maboury Diao, Adama Kane, Malick Bodian, Alassane Mbaye et al. (2010) Infective endocarditis in cardiac setting in Dakar: descriptive study about 39 cases. Pan Afr Med J 7: 12. [Crossref]
- Bouramoue C, Nkoua JL, Kimbally Kaky G et al. (1992) Endocardite infectieuse: Experience d’un service brazzavillois: à propos de 47 cas. Cardiol Trop 18: 134.
- Ba S A, Diouf SM, Bao O et al. (1992) Ecueils diagnostiques et thérapeutiques de l’endocardite infectieuse: à propos de 33 observations. Cardio Trop 18: 135.
- Ndiaye M.B, Diao M, Pessinaba S (2012) Endocardite infectieuse aorto-pulmonaire d’évolution fatale: à propos d’un cas. Ann Cardiol Angeiol 61: 118-120.
- Kangah M (1992) Endocardites infectieuses opérées en urgence à Abidjan. Facteurs de risque. Résultats chirurgicaux: indications opératoires actuelles. Cardiologie tropicale 18: 136.
- J S Li, D J Sexton, N Mick, R Nettles, V G Fowler Jr et al. (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30: 633-638. [Crossref]
- Christine Selton Suty, Marie Célard, Vincent Le Moing, Thanh Doco Lecompte, Catherine Chirouze et al. (2012) Preeminence of Staphylococcus aureus in infective endocarditis: a 1-year population-based survey. Clin Infect Dis 54: 1230-1239. [Crossref]
- Tattevin P (2017) Antibiothérapie des endocardites infectieuses: lecture critique des recommandations 2015. Antibacterial treatment of infective endocarditis: Critical review of 2015 guidelines. J des Anti-Infectieux.
- Delahaye F (2016) Quelles endocardites infectieuses chez l’adulte faire opérer en urgence? Presse Med.
