Infarcted Fibroadenoma of the Breast: Difficulties in Diagnosis
A B S T R A C T
Introduction: Infarction is a very rare complication of fibroadenoma. Diagnosis of such a situation is not easy.
Case Presentation: 23-year-old woman with a painful tumor of the right breast with mild erythema at the periareolar region. Breast ultrasound shows a heterogeneous lesion of 31×30 mm, in the retroareolar right breast with well-defined borders, and does not present vascular flow inside. Antibiotic treatment was administered without improvement. The breast ultrasound was repeated with no significant changes. Surgical removal of a well-encapsulated cystic lesion was performed. The patient was discharged the same day of surgery, and her postoperative evolution was correct. Histopathologic evaluation revealed an infarcted fibroadenoma.
Conclusion: Breast ultrasound could be very useful in the diagnosis of infarcted fibroadenoma; treatment consists of local excision of the lesion.
Keywords
Fibroadenoma, infarction, diagnosis, breast, ultrasound
Established Facts
i. Infarcted fibroadenoma is a very rare clinical situation
ii. Is more frequent in young ages
Novel Insights
i. Infarcted fibroadenoma should be in the differential diagnosis of painful breast tumor.
ii. Breast ultrasound was very useful in the diagnosis of infarct fibroadenoma, heterogeneous mass with an absence of vascularization.
iii. It is very important not to confuse necrotic changes with malignancy to avoid inappropriate treatments.
Introduction
Fibroadenomas are fibroepithelial lesions that represent the most common benign neoplasms of the breast [1-3]. These tumors usually affect young women (between 20 and 30 years) [2]. The diagnosis of fibroadenomas is easy; they typically present as a palpable, mobile, and painless mass, although they can sometimes be painful just before menstruation when the breast tissue responds to the action of progesterone. Fibroadenomas are usually small in size, but in certain cases, they can reach considerable size; in these cases, we must rule out a phyllodes tumor. Breast fibroadenoma infarction is a very rare complication. We present a case of spontaneous fibroadenoma infarction in a young patient without any risk factors, and we discuss clinical and diagnostic events.
Case Report
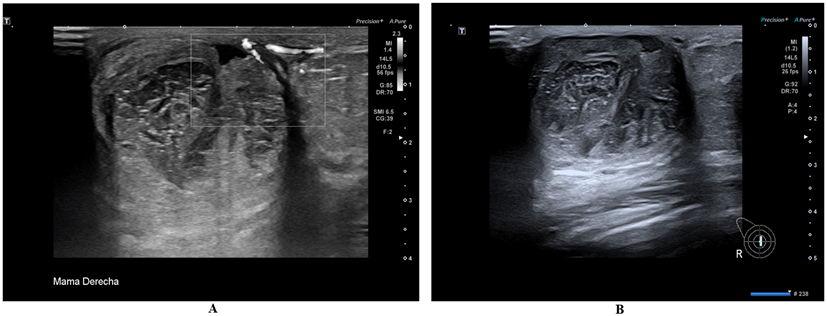
A 23-year-old nulliparous woman presented to our outclinic department because painful tumor of her right breast; she was in the second phase of her menstrual cycle. In her medical history, only acne treated with isotretinoin 40 mg per day stands out. The physical examination of the right breast shows mild erythema in the periareolar region with a tumefaction of the area. Palpation of this area is painful and revealed a mobile tumor of 3cm in diameter. A breast ultrasound is performed to rule out a breast abscess. Breast ultrasound shows the presence of a heterogeneous lesion with a size approximately of 31x30 mm, in the retroareolar right breast with well-defined borders, with posterior enhancement, which does not present vascular flow inside, as shown in (Figure 1A). The diagnostic orientation was a complicated cyst.
Figure 1: A) Description: Presence of heterogeneous retroareolar lesion in the right breast with well-defined borders, shows posterior enhancement, approximate measurements of 31×30 mm, does not present vascular flow inside. 4kPa elastography (low values, not solid). B) No significant changes were seen in the second breast ultrasound, so the final diagnosis was a heterogeneous right retroareolar lesion. Findings raise diagnosis of the complicated cyst, solid lesion with necrosis inside.
Amoxi-clavulanate 500mg was administered every 8 hours for 10 days without improvement, breast ultrasound was repeated two weeks later. No significant changes were seen in the breast ultrasound, so the final diagnosis was a heterogeneous right retroareolar lesion, which due to its evolution, may be a solid lesion with areas of necrosis or hemorrhage, as shown in (Figure 1B). Surgical removal was indicated, a periareolar incision was made and a well-encapsulated cystic lesion was excised, producing a rupture of the capsule in the extraction, observing the exit of necrotic material. The surgical specimen was sent for a pathology study.
The patient was discharged the same day of surgery and her postoperative evolution was correct. Histopathologic evaluation revealed an infarcted fibroadenoma (4.5cm) with the presence of hemorrhage and necrosis shown in (Figure 2).
Figure 2: Histopathologic evaluation revealed an infarcted fibroadenoma with foci of hemorrhage. No evidence of malignancy was found (H&E, 4x).
Discussion
In 1949 Delaure and Redon were the first to diagnose spontaneous infarction in fibroadenoma among young women [4]. The frequency of infarction within fibroadenoma reported in different series varies from 0.3 to 3.6% [5-8]. The pathogenesis of infarcted fibroadenomas is not clear but are clinical situation associated. Risk factors associated with an infarcted fibroadenoma were described in the literature in pregnancy, lactation, thrombo-occlusives diseases, trauma and fine-needle aspiration cytology (FNAC). In our patient, none of these factors were present; although she has a history of taking retinoids, which are associated with a low risk of thrombosis, Newman et al. found thrombo-occlusive vascular changes as a possible cause of infarction within fibroadenomas [9].
Fibroadenomas are very common in young women (in their 20s and 30s) like in our patients [2]. The age of women presenting infarcted fibroadenoma described in the literature varies from 13 to 29-year-old, our patient had 23 years-old. The symptoms of infarcted fibroadenoma are rapid growth of the breast tumor with pain and tenderness, all of which were present in our case [2]. Differential diagnosis must be considered with mastitis and duct ectasia; our patient was treated with an antibiotic to discard mastitis with breast abscess. Other less frequent diagnoses with which to make the differential diagnosis are phyllodes tumor or carcinoma. In our case, breast ultrasound was very useful to give a correct diagnosis, with an absence of vascularization in the heterogeneous mass.
The most common recommended investigation for breast masses is FNAC [10]. In the FNAC, microscopic features of infarcted fibroadenoma are several individually scattered round or oval cells, without atypical features, and ghostly epithelial cells in a necrotic background [1]. In our case, the absence of suspicion of malignancy and the non-resolution of the condition after antibiotic treatment led us to perform tumor removal. It is very important not to confuse these necrotic changes with malignancy to avoid inappropriate treatments.
The definitive diagnosis of infarct fibroadenoma is the histopathological examination in which abundant areas of ischaemic necrosis, and hemorrhage with partial or null retention of the original architecture of the fibroadenoma without inflammatory or atypical cells can be observed [1]. In our case, the histological examination showed fibroadenoma with necrotic and hemorrhagic changes.
Conclusion
Breast ultrasound could be very useful in the diagnosis of infarcted fibroadenoma, whose treatment is conservative with local excision of the lesion.
Ethical Approval
The study protocol was reviewed and approved by Research Ethics Committee Fundació Sant Joan de Deu, approval number ART-04-22.
Consent
Written informed consent has been obtained from the patient for publication of the details of their medical case and any accompanying images.
Conflicts of Interest
None.
Funding
None.
Author Contributions
Eduardo Gonzalez Bosquet: designing and writing the manuscript; Paulino Sousa: provision of ultrasound images and writing legends of figures 1A and 1B, reviewing and approving the text; Carlota Rovira: provision of histologic images and writing legend of figure 2 reviewing and approving the text.
Data Availability
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Article Info
Article Type
Case ReportPublication history
Received: Wed 08, Jun 2022Accepted: Wed 22, Jun 2022
Published: Thu 30, Jun 2022
Copyright
© 2023 Eduardo González Bosquet. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2022.06.04
Author Info
Eduardo González Bosquet Paulino Sousa Carlota Rovira
Corresponding Author
Eduardo González BosquetDepartment Obstetrics and Gynecology, Sant Joan de Déu Hospital, University of Barcelona, Barcelona, Spain
Figures & Tables

References
1. Salih AM, Kakamad
FH (2016) Spontaneous infarction of fibroadenoma of breast-A case report with
literature review. Int J Surg Case Rep 24: 1-3. [Crossref]
2. Singh SK, Gupta P,
Arora R, Singla S, Mishra B et al. (2017) Giant fibroadenoma with massive
infarction masquerading as malignancy: a case report. Int Cancer Conf J
6: 167-170. [Crossref]
3. Fukui S, Yamaguchi
K, Nakazono T, Egashira R, Nakamura J et al. (2018) Breast MRI findings of
fibroadenoma with hemorrhagic infarction. Breast J 24: 1078-1079. [Crossref]
4. Delarue J, Redon H
(1949) Myocardial fibro-adenoma breast; clinical problem and pathogenesis. Sem
Hop 25: 2991-2996. [Crossref]
5. Jayasinghe Y,
Simmons PS (2009) Fibroadenomas in adolescence. Curr Opin Obstet Gynecol
21: 402-406. [Crossref]
6.
Onuigbo
W (2003) Breast fibroadenoma in teenage females. Turk J Pediatr 45: 326-328. [Crossref]
7. Al Atrooshi SA (2012) Fibroepithelial tumor of female breast: a review of 250
cases of fibroadenomas and phylloides tumors. Iraqi Postgrad Med J 11:
140-145.
8. Skenderi F,
Krakonja F, Vranic S (2013) Infarcted fibroadenoma of the breast: report of two
new cases with review of the literature. Diagn Pathol 8: 38. [Crossref]
9. Newmann J, Kahn LB (1973) Infarction of fibro-adenoma of the breast. Br J Surg 60: 738-740. [Crossref]
10. Wadhwa N, Joshi R, Mangal N, Khan NP, Joshi M (2014) Cytopathologic diagnosis of spontaneous infarction of fibroadenoma of the breast. Turk Patoloji Derg 30: 237-240. [Crossref]
