Incidentally Detected Asymptomatic Thrombus in the Inferior Vena Cava Thought to be Caused by Central Venous Catheterization for an Oral Surgical Procedure
A B S T R A C T
Central venous catheterization (CVC) is a common procedure in the perioperative period, and thrombosis is one of the well-known complications of CVC. If the thrombus comes free from the vascular wall, it may cause serious problems such as pulmonary embolism. However, in some cases of inferior vena cava thrombosis, the patient has no symptoms, and thrombus is detected accidentally. A case in which asymptomatic thrombus in the inferior vena cava was incidentally detected following removal of the CV catheter after an oral surgical procedure is described.
Keywords
Central venous catheter, inferior vena cava, thrombosis, oral surgery, femoral vein
Introduction
Central venous catheterization (CVC) is used for various purposes in the perioperative period, such as measurements of central venous pressure (CVP), administration of cardiovascular agents, intravenous hyperalimentation, etc. In some cases of orofacial surgery, a CV catheter is inserted from the femoral vein so as to not interfere with the operative procedure.
Case Report
A 59-year-old (weight 62 kg, height 174 cm) man with carcinoma of the oral floor (T4aN1M0) was scheduled for tracheostomy, right neck dissection, resection of the tumor, and oral reconstructive surgery with a right anterolateral thigh flap. Past medical history included well-controlled hypertension, diabetes, and COPD. He had no history of thrombosis. Although a recessed lesion in the stomach was detected on preoperative gastrointestinal screening, the workup and treatment for the lesion were planned after oral surgery.
On the operation day, after induction of anaesthesia, a double-lumen, 12-gauge CV catheter (SMACTM plus, Covidien Japan, Tokyo, Japan) was inserted via the left femoral vein, and the tip was fixed 47 cm from the insertion point. The catheter lumens were used for transfusion and continuous measurement of CVP. The operation was completed without incident. Total bleeding was 800 mL, and total infusion volume, which included transfusion of 4 units of packed red blood cells, was 6150 mL, whereas total urine volume was 4400 mL. There was no abnormality of the indwelling catheter on the postoperative chest x-ray. The patient’s postoperative course was favorable, and the CV catheter was removed on postoperative day (POD) 5, and the patient was discharged on POD 56.
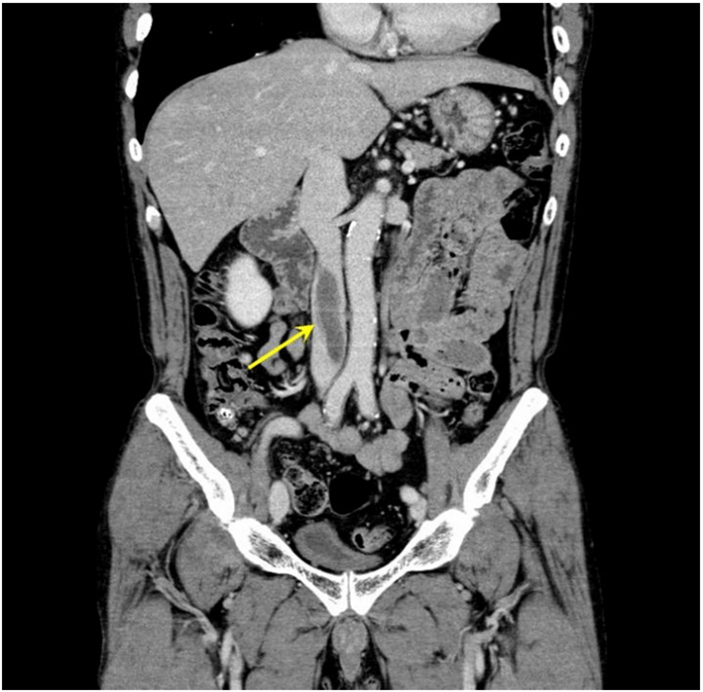
Endoscopic submucosal dissection (ESD) was scheduled two months after discharge. However, a 7 cm-long thrombus in the inferior vena cava was detected on contrast-enhanced CT (Figure 1). The ESD was then postponed, and anticoagulant therapy was started. Fortunately, a marked reduction of the thrombus was observed, and a complete disappearance of the thrombus was confirmed 53 days after the beginning of the therapy. Anticoagulant therapy was then stopped, and the ESD was performed. No severe complications such as pulmonary embolism occurred from the time of finding the thrombus to its disappearance. No relapse of the thrombus was observed for seven months after its disappearance.
Figure 1: The inferior vena cava thrombus 51 days after removal of the CV catheter (arrow).
Discussion
It is well known that CVC via the femoral vein has a greater risk of provoking thrombosis than CVC via the internal jugular vein or subclavian vein [1]. It is also well known that insertion of the CV catheter via the left femoral vein is sometimes difficult, because the left iliac vein is often compressed by the left iliac artery, and there is stenosis or thrombus inside the vein at the compressed point [2]. However, whether the insertion of the CV catheter via the left femoral vein provokes thrombosis more than insertion via the right one is unknown. Therefore, the extent of the relationship between the formation of the thrombus and the insertion of the catheter via the left femoral vein in the present case is unclear.
Satokawa et al. classified 13 cases of inferior vena cava thrombosis into four types: BI type (connected with bilateral iliac vein thrombosis); UI type (connected with unilateral iliac vein thrombosis); skip type (not connected with lower limb vein thrombosis); and isolated type (only inferior vena cava thrombosis) [3]. In the skip type and isolated type cases, CVCs via the femoral vein were performed; therefore, they suggested that CVC would directly cause thrombosis in both types of cases. Hence, in the present case (isolated type in Satokawa’s classification) also, CVC would have provoked the inferior vena cava thrombosis. Furthermore, there were other factors causing thrombosis in this case, such as malignant disease, post-surgery and recumbency lasting several days.
It is difficult to rule out the possibility that thrombosis was present preoperatively because contrast-enhanced CT was not performed before insertion of the CV catheter in this case. However, the effectiveness of anticoagulant therapy for the thrombus suggested that it was not old but fresh thrombosis [4]. The symptoms of congestion or edema are not commonly found in cases of inferior vena cava thrombosis if there is not complete obstruction [5]. Thus, asymptomatic inferior vena cava thrombosis is often incidentally found on diagnostic imaging for other purposes. If the thrombus comes free from the vascular wall, the patient may have a fatal outcome [6]. Therefore, it may be necessary to examine for the presence or absence of thrombus in the inferior vena cava with blood tests or diagnostic imaging before removal of the CV catheter, especially in cases in which the patient has several pathological and surgical factors increasing the likelihood of thrombosis.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 06, Nov 2020Accepted: Fri 20, Nov 2020
Published: Thu 17, Dec 2020
Copyright
© 2023 Shigeru Takuma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JCMCR.2020.04.01
Author Info
Shigeru Takuma Yukifumi Kimura Nobuhito Kamekura Toshiaki Fujisawa
Corresponding Author
Shigeru TakumaAssistant Professor, Department of Dental Anesthesiology, Graduate School of Dental Medicine, Hokkaido University, Sapporo, Japan
Figures & Tables
References
- McGee DC, Gould MK (2003) Preventing complications of central venous catheterization. N Engl J Med 348: 1123-1133. [Crossref]
- Oguzkurt L, Ozkan U, Ulusan S, Koc Z, Tercan F (2008) Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep vein thrombosis. J Vasc Interv Radiol 19: 366-371. [Crossref]
- Satokawa H, Hoshino S, Iwaya F, Igari T, Midorikawa H et al. (1996) Treatment for inferior vena caval thrombosis. Jpn J Phlebology 7: 293-300.
- JCS Joint Working Group (2011) Guidelines for the diagnosis, treatment and prevention of pulmonary thromboembolism and deep vein thrombosis (JCS2009). Circ J 75: 1258-1281. [Crossref]
- McAree BJ, O’Donnell ME, Fitzmaurice GJ, Reid JA, Spence RAJ et al. (2013) Inferior vena cava thrombosis; A review of current practice. Vasc Med 18: 32-43. [Crossref]
- Ota M, Nakamura M, Yamada N, Yazu T, Ishikura K et al. (2002) Prognostic significance of early diagnosis in acute pulmonary thromboembolism with circulatory failure. Heart Vessels 17: 7-11. [Crossref]
