Idiopathic Omental Infarction Mimic Acute Appendicitis: A Case Report
A B S T R A C T
Idiopathic Omental Infarct (IOI) is a rare cause of an acute abdomen that arises from an interruption of blood supply to the omentum. Since first case was described by Elitelin 1899, more than 300 cases have been published [1]. It can mimic serious surgical pathology. It occurs in <1% of appendicitis cases [2]. It’s challenge to diagnose, as features may mimic acute appendicitis and therefore in young patients, may only be discovered intra-operative. Here, we present a case of omental infarct in 26-year-old gentleman with no significant medical or surgical background who present with acute onset of right iliac fossa (RIF) pain. Examination revealed tenderness over the right iliac fossa and was having localized rebound. His inflammatory markers were high. He was successfully treated with laparoscopy surgery and he was subsequently discharged the following day.
Keywords
Omental infarction, acute appendicitis, laparoscopic surgery, right iliac fossa pain
Introduction
Omental infarction is a rare cause of an acute abdomen that arises from an interruption of blood supply to the omentum and may be caused by torsion of the omentum around its vascular pedicle or venous outflow obstruction or vasculitis or thrombosis of the omental vessel, which can mimic the common presentations of acute appendicitis, acute cholecystitis or diverticulitis [3]. The omentum is double sheet of flattened endothelium with epiploic vessels, lymphatics, nerves, and fatty areolar tissue pass in between, hangs as a double fold between the greater curve of the stomach to the transverse colon with the right side usually longer and larger [4]. Size depends on the amount of fat, usually underdeveloped in infants. It acts as Policeman of the abdomen helps in walling of inflammatory conditions.
While mesentery is a reflection of the posterior peritoneum connects the intestine to the posterior abdominal wall and carries blood vessel and nerves. Root of the mesentery extends from the ligament of Treitz at the level of L2 and is approximately 6 inches. Mesocolon suspensory ligament of the transverse and sigmoid colon. Space of Riolan is avascular space to the left of the middle colic artery. Omental infarct can be classified as primary or secondary and can occur with or without torsion. Primary Omental infarct, with or without torsion occur commonly in obese patient and is associated with congenital anatomic variation [2].
Case Report
26-year-old gentleman with no significant medical or surgical history, presented via emergency department with history of sever RIF pain for 1 day. He reported sever sudden, dull, non-radiating RIF pain, with no relieving or aggravating factors, associated with nausea and subjective fever. No history of vomiting, constipation, diarrhea or anorexia. He has also denied any previous abdominal trauma or recent surgery. No other associated symptoms. No previous similar illness. Systemic review unremarkable. No family history of any hematological disease.
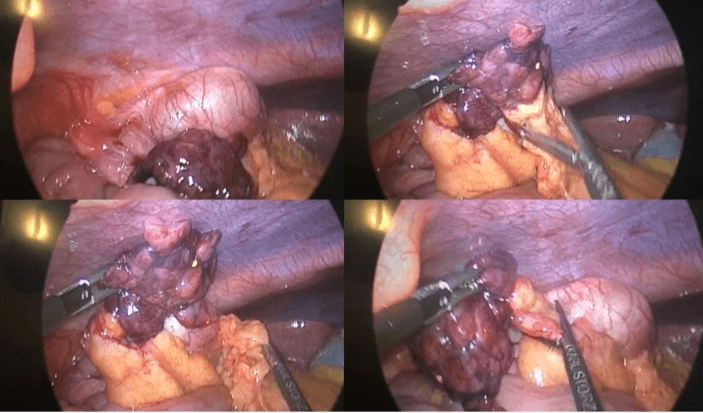
On examination, he was conscious alert, vital signs within normal (HR:84 BPM, BP:117/66 mmHg, O2sat.:99% on Room air, T: 37.4 C), BMI: 37.3 abdominal examination revealed RIF tenderness with positive rebound tenderness. His examination otherwise unremarkable. Urine analysis was normal. Blood tests revealed an elevated white cell count 13.5x10^9/L with left shift. An initial differential diagnosis was made as acute appendicitis. Appropriate intravenous resuscitation and antibiotics were started. Patient was consented for laparoscopic appendectomy and proceed then push same night for surgery. On laparoscopy, exploration was done, 3x4 infarcted omentum was found associated with minimal serous fluid in the pelvis (Figure 1). Appendix, cecum, entire colon and small bowel were grossly unremarkable. An omental necrosectomy and appendectomy was done.
Figure 1: Laparoscopic picture showing infarcted omentum adherent to cecum and adjacent healthy omentum.
Improved post-operative with no more pain or fever and tolerating regular diet. He was discharged one day later on simple analgesic (paracetamol). Histopathology result was:
i. Appendix: Normal Appendix tissue, negative for malignancy.
ii. Omentum: Mature adipose tissue, negative for malignancy.
Discussion
Omental infarction is a rare cause of acute abdomen, with an incidence equivalent to less than four cases per 1000 cases of appendicitis [2]. Historically, omental infarction was diagnosed only intraoperatively during surgery for presumed appendicitis or other causes of acute abdomen. But with the increase in the use of imaging, especially abdominal computed tomography (CT) scan in the work-up for acute abdomen, more cases of omental infarction are being diagnosed preoperatively [2]. This has also led to the observation that omental infarction is a self-limiting condition which can be managed conservatively. Omental infarct depending on the area of infarction can mimicked acute appendicitis, acute cholecystitis, or even acute diverticulitis [5, 6].
The exact pathogenesis of the omental infarction is still unclear but there have been many theories of how it occurs. In most instances is affecting the right side of the abdomen [4]. It can be divided into 2 classes primary and secondary and are commonly associated with risk factors such as anatomic variation in blood supply to the end of omental, obesity, trauma, coughing, sudden body movement [7]. Secondary causes include hypercoagulability, polycythemia, vasculitis and adhesions. Primary cause is considered when there are no recognizable causes found otherwise known as idiopathic [2]. In the above case, we think that this is likely a primary omental infarction case. Some authors have suggested that it is due to a different embryonic origin of the right sided omentum as the right sided omentum consist of more fragile blood vessel and are more susceptible to occlusion [4]. Some have also observed that omental infarction typically occurs after a heavy meal and is caused by venous engorgement and similarly. Obesity is a known risk factor, the hypothesis being that an excessive weight of the omentum cause venous engorgement and elongation also fatty omentum may occlude its own distal atrial branches [8]. From our reading, we summaries pathophysiology behind omental and mesenteric infarction.
I Omental Infarction
i. Torsion twisting along its long axis causing vascular compromise. requirements for torsion is redundant segment and a fixed point. It can be Primary with predisposing factors such as projections from the edge of the omentum, obesity, and venous redundancy and secondary which associated with another pathology such as omental cysts, tumors, inflammatory conditions or hernias, right side twists more frequent [4]. Clinical manifestations will be sudden, constant pain, increasing in intensity associated with nausea and vomiting, on examination there will be signs of peritonitis and possible palpable mass [8].
ii. Idiopathic Segmental Infarction (acute vascular occlusion) not accompanied by torsion, intraabdominal conditions, trauma, or cardiac disease. Caused by thrombosis of the omental veins secondary to endothelia injury and usually involves the right side [9]. Clinical manifestation will be pain more of gradual in onset. Diagnosis through CT scan which will show a smudged appearance. Treatment will be excision of involved segment.
iii. Cysts which caused by obstruction of lymphatic channels and growth of congenitally misplaced lymphatic tissue. It will be manifested as palpable mass. X-ray can diagnose dermoid cyst. Ultrasound and CT scan could help to diagnose.
iv. Solid tumors, metastatic carcinoma most common. Hemangiopericytoma and leiomyosarcoma most common primary tumors. Diagnosis made by ultrasound or CT scan. Treatment will be excision of the primary tumor if possible and omentum.
II Mesenteric Infarction
i. Acute occlusion of the SMA, either embolic which manifested as sudden occlusion of the main branch of the SMA produces ischaemia of the entire small bowel distal to the ligament of Treitz and proximal half of the colon, or thrombotic which occurs in an artery partially occluded by atherosclerosis, slowly developing stenosis may allow time for collaterals to develop. Sudden complete occlusion first causing an ischaemic infarct in which the bowel is pale, later stages will show haemorrhagic infarction. It is surgical emergency with extreme abdominal pain not proportional to the pain the patient perceives, unresponsive to narcotics and absent bowel sounds with mottled, cyanotic bowel on exploration. Diagnosis made by arteriogram, patient will have leukocytosis, Hct hemoconcentration, metabolic acidosis. Treatment including NGT, antibiotics, anticoagulation, embolectomy and resection of affected part.
ii. Non-occlusive mesenteric infarction, caused by hypo-perfusion secondary to low cardiac output (CHF, MI), septic shock, arrhythmia. Diagnosis made by arteriography. Treatment consist of correction of hypo-perfusion status, vasodilators and antibiotics.
iii. Chronic occlusion of visceral arteries which will cause intestinal angina, ischaemia without infarction, food pain sequence. Pathology behind it is partial occlusion secondary to atherosclerosis. Clinical manifestation will be post-prandial crampy abdominal with weight loss. Diagnosis made by arteriogram. Treatment consist of arterial reconstruction, thromboendarterectomy, synthetic vein graft or resection of affected segment.
iv. Occlusion of mesenteric veins usually caused by thrombosis secondary to hyperemia, edema, or sub-serosal haemorrhage. Clinically manifested as vague discomfort and severe abdominal pain. Treatment consist of resection of affected segment, antibiotics and anticoagulant.
Till date there is still no studies comparing significant difference between conservative management and surgical management and with limited evidence. Management of omental infarct can varies according to surgeons experience. If a patient symptom has not improved after 24 hours of conservative management, laparoscopic management can be considered as it presents with a method for exploration and treatment. At the same time, laparoscopic management overall reduce hospital stay and it is thought to prevent complication of conservative management such as abscess formation.
Conclusion
IOI is a rare benign condition, which can mimic clinically common serious intra-abdominal pathology and might only be diagnosed intra-operative. High suspicion in addition to proper radiological imaging could help to pick it up. Both surgical and conservative management are optimal with no evidence of superiority of one over the other. Our case diagnosed and managed surgically with no early nor late complications.
Article Info
Article Type
Case ReportPublication history
Received: Mon 09, Nov 2020Accepted: Thu 19, Nov 2020
Published: Tue 08, Dec 2020
Copyright
© 2023 Hamad Almakinzy. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.12.07
Author Info
Corresponding Author
Hamad AlmakinzyDepartment of General Surgery, Prince Sultan Military Medical City, Riyadh, Kingdom of Saudi Arabia
Figures & Tables
References
- Eitel GG (1899) Rare omental torsion. NY Med Rec 55: 715.
- Itenberg E, Mariadason J, Khersonsky J, Wallack M (2010) Modern management of omental torsion and omental infarction: a surgeon’s perspective. J Surg Educ 67: 44-47. [Crossref]
- Yoo E, Kim FH, Kim MJ, Yu JS, Chung JJ et al. (2007) Greater and lesser omenta: normal anatomy and pathologic processes. Radiographics 27: 707-720. [Crossref]
- Battaglia L, Belli F, Vannelli A, Bonfanti G, Gallino G et al. (2008) Simultaneous idiopathic segmental infarction of the great omentum and acute appendicitis: a rare association. World J Emerg Surg 3: 30. [Crossref]
- Goti F, Hollmann R, Stieger R, Lange J (2000) Idiopathic segmental infarction of the greater omentum successfully treated by laparoscopy: report of case. Surg Today 30: 451-453. [Crossref]
- Loh MH, Chui HC, Yap TL, Sundfor A, Tan CE (2005) Omental infarction--a mimicker of acute appendicitis in children. J Pediatr Surg 40: 1224-1226. [Crossref]
- Barai KP, Knight BC (2011) Diagnosis and management of idiopathic omental infarction: A case report. Int J Surg Case Rep 2: 138-140. [Crossref]
- Epstein LI, Lempke RE (1968) Primary idiopathic segmental infarction of the greater omentum: case report and collective review of the literature. Ann Surg 167: 437-443. [Crossref]
- Scobie BA (1998) Gastrointestinal emergencies with marathon-type running: omental infarction with pancreatitis and liver failure with portal vein thrombosis. N Z Med J 111: 211-212. [Crossref]
- Park TU, Oh JH, Chang IT, Lee SJ, Kim SE et al. (2012) Omental infarction: case series and review of the literature. J Emerg Med 42: 149-154. [Crossref]
