Journals
Humeral Osteomyelitis with Apophysomyces ossiformis in an Immunocompetent Patient: A Case Report
A B S T R A C T
Introduction
Osteomyelitis of a limb can lead to devastating functional consequences. Fungal osteomyelitis is rare in immunocompetent patients, and compared to bacterial osteomyelitis, fungal infections are more difficult to eradicate.
Case Report
We present a case of a 59-year-old male who suffered traumatic left open radius and ulna fractures at the elbow with significant soft tissue loss. He underwent spanning fixation across the elbow, and soft tissue coverage was provided with a free latissimus flap. At the time of flap coverage, the patient was found to have fungal osteomyelitis with the organism Apophysomyces ossiformis. The patient achieved wound closure and functional use of the left upper extremity.
Conclusion
The reported case demonstrates the pathogenicity of a microorganism not previously described in human disease. In this case, treatment was successful with local debridement, placement of antibiotic beads, and long-term antifungal therapy.
Keywords
Fungal osteomyelitis, Apophysomyces ossiformis, limb salvage, free tissue transfer
Introduction
Osteomyelitis is a challenging problem for clinicians to face. Either through direct inoculation or hematogenous spread, pathogenic invasion of the bone leads to destruction of native architecture and biophysical signaling pathways, leading to impaired mechanical stability and fracture healing capacity [1]. In severe infections, patients may also have systemic, life-threatening symptoms. More commonly, osteomyelitis presents as a localized infection. In the limbs, this has profound implications on functional capacity. While antibiotic therapy alone may be effective in certain cases of acute infection, surgical intervention is commonly required concurrently to remove all sequestra and nonviable tissue, allowing healing of the bone and soft tissue envelope [2]. Implanted hardware most commonly needs to be removed. In more severe cases, reconstruction of the bony and soft tissue defect with or without bone lengthening and/or free tissue transfer may be needed [3]. If a limb is not salvageable or the disease cannot be cleared, amputation is required. Osteomyelitis caused by fungal pathogens is much less common than bacterial osteomyelitis, and cases are more typical in immunosuppressed and/or diabetic patients [4]. Given the typical indolence of these pathogens, surgical intervention is often mandatory in combination with prolonged antifungal therapy [5]. Here we describe a case of fungal osteomyelitis of the humerus in an immunocompetent patient who was treated successfully and has regained use of the affected limb.
Case Presentation
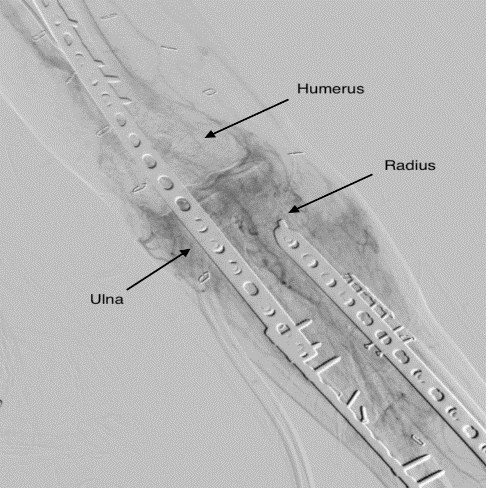
A 58-year-old healthy male was involved in a motor vehicle accident, suffering thoracic spine fractures, rib fractures, a pneumothorax, and left open fractures of the radius and ulna including the olecranon. The patient was stabilized from a trauma perspective and underwent multiple debridements to the left elbow. Ultimately the ulna and radius underwent internal fixation and a spanning plate was placed across the humerus to the ulna (Figure 1). However, the patient had insufficient soft tissue envelope to cover the elbow wound and underlying bone and hardware. The patient underwent prolonged wound care using vacuum assisted suction devices for over a month.
Figure 1: Pre-operative angiogram image of the left elbow demonstrating internal fixation. Note the fixation plates on the radius and ulna as well as the spanning plate across the humerus and ulna.
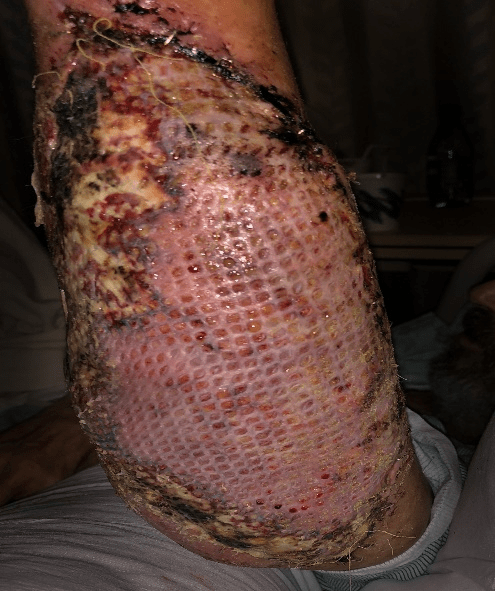
The wound failed to close over this period, and the patient was transferred to a specialized reconstructive microsurgery facility for soft tissue coverage. The patient’s wound at this point was 400 cm2 with exposure of the elbow hardware and bone. Free tissue transfer was planned for coverage. At the time of reconstruction, it was noted that gross fungal elements were growing on the distal humerus and lateral epicondyle (Figure 2).
Figure 2: Intraoperative view of left elbow wound. Panel A: View demonstrating wound size and exposed structures. Note the exposed spanning plate from the humerus superiorly to the ulna inferiorly. Panel B: Zoomed view demonstrating gross hyphal elements growing on the humerus/lateral epicondyle.
The fungal elements and underlying necrotic bone were debrided back to healthy tissue, and specimens were sent for laboratory analysis. Prior consultation with the referring orthopedist noted that removal of the hardware would likely preclude limb salvage, and thus soft tissue reconstruction proceeded without removal of the in-situ plates. Given the fungal element findings, polymethylmethacrylate beads impregnated with amphotericin B were placed at the distal humerus site. A free latissimus flap was then placed over the wound, utilizing the thoracodorsal pedicle with end-to-side anastomosis to the brachial artery and end-to-end anastomosis to the basilic vein. A split thickness skin graft was placed over the latissimus muscle.
The fungal elements and underlying necrotic bone were debrided back to healthy tissue, and specimens were sent for laboratory analysis. Prior consultation with the referring orthopedist noted that removal of the hardware would likely preclude limb salvage, and thus soft tissue reconstruction proceeded without removal of the in-situ plates. Given the fungal element findings, polymethylmethacrylate beads impregnated with amphotericin B were placed at the distal humerus site. A free latissimus flap was then placed over the wound, utilizing the thoracodorsal pedicle with end-to-side anastomosis to the brachial artery and end-to-end anastomosis to the basilic vein. A split thickness skin graft was placed over the latissimus muscle.
Figure 3: View of free latissimus flap 5 days after surgery and takedown of splint. Note necrosis of the skin graft at the perimeter of the flap, while the center bulk of the flap is viable with skin graft take.
Discussion
Over 100,000 fungal species have been defined, and approximately 150 species are known to be pathogenic to mammals. Common species include Candida, Aspergillus, Coccidioides, Histoplasma, Blastomyces, and Cryptococcus [4]. Apophysomyces species (which are causative agents of zygomycosis) are opportunistic and typically affect immunocompromised patients [7]. A. trapeziformis has been found as a causative agent in septic arthritis, A. elegans has been seen as a causative agent of rhino-oculo-cerebral mucormycosis, and A. variabilis has been implicated in necrotizing fasciitis [8-10]. A. ossiformis was only described as a distinct species in 2010 and is characterized by its bone-shaped sporangiospores. Amphotericin B and posaconazole have been described as effective anti-fungal agents in vitro, but no clinical guidelines for treatment are available [11]. At the time of this case report, there have been no other documented human infections by this organism.
Based on this case, it appears that this organism can be controlled by following current standards of care for osteomyelitis. Indeed, in this case radical removal of all potentially infected tissue and hardware was not performed. This implies that while A. ossiformis is virulent enough to infect immunocompetent patients, it is not so aggressive to require radical debridement; this is in contrast to other Apophysomyces species [12]. While amphotericin B was utilized locally, systemic therapy with this agent was avoided, sparing the patient from potential morbidity from this macrolide [13]. However, it must be highlighted in this case that follow up was only 7 months, and the resurgence of underlying infection remains a possibility.
Conclusions
This case report demonstrates A. ossiformis as a human pathogen causing osteomyelitis. Traditional surgical technique and antibiotic therapy appear effective in treating an infection with this organism in an immunocompetent patient; however, current evidence-based guidelines are needed.
Article Info
Article Type
Case ReportPublication history
Received: Wed 27, Feb 2019Accepted: Sat 16, Mar 2019
Published: Sat 30, Mar 2019
Copyright
© 2023 Travis J. Miller. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.02.07
Author Info
Andrew J. Watt Clifford C. Sheckter Travis J. Miller
Corresponding Author
Travis J. MillerDepartment of Surgery, Division of Plastic and Reconstructive Surgery, Stanford University School of Medicine, Stanford, CA 94304, USA
Figures & Tables

References
- Tiemann AH, Hofmann GO (2009) Principles of the therapy of bone infections in adult extremities. Strategies Trauma Limb Reconstr 4: 57-64.
- Maffulli N, Papalia R, Zampogna B, Torre G, Albo E, et al. (2016) The management of osteomyelitis in the adult. Surgeon 14: 345-360. [Crossref]
- Lowenberg DW, Buntic RF, Buncke GM, Parrett BM (2013) Long-Term Results and Costs of Muscle Flap Coverage with Ilizarov Bone Transport in Lower Limb Salvage. J Orthop Trauma 27: 576-581. [Crossref]
- Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda CRA, et al. (2014) Fungal Osteomyelitis and Septic Arthritis. J Am Acad Orthop Surg 22: 390-401. [Crossref]
- Kohli R, Hadley S (2005) Fungal arthritis and osteomyelitis. Infect Dis Clin North Am 19: 831-851. [Crossref]
- Arkun R (2004) Parasitic and fungal disease of bones and joints. Semin Musculoskelet Radiol 8: 231-242. [Crossref]
- Ribes JA, Vanover-Sams CL, Baker DJ (2000) Zygomycetes in Human Disease. Clin Microbiol Rev 13: 236-301. [Crossref]
- Bertumen JB, Schell WA, Joyce M, Alley C, Woods CW (2016) Diagnostic difficulty identifying Apophysomyces trapeziformis septic arthritis in a patient with multiple myeloma. JMM Case Rep 3: e005075. [Crossref]
- Biswas D, Kotwal A, Kakati B, Ahmad S (2015) Amphotericin B Resistant Apophysomyces elegans Causing Rhino-oculo-Cerebral Mucormycosis in an Immunocompetent Host. J Clin Diagn Res 9: DD01-DD02. [Crossref]
- Rodríguez JY, Morales-López SE, Rodríguez GJ, Álvarez-Moreno CA, Ocampo W, et al. (2017) Necrotizing fasciitis caused by Apophysomyces variabilis in an immunocompetent patient. Med Mycol Case Rep 20: 4-6. [Crossref]
- Alvarez E, Stchigel AM, Cano J, Sutton DA, Fothergill AW, et al. (2010) Molecular phylogenetic diversity of the emerging mucoralean fungus Apophysomyces: proposal of three new species. Rev Iberoam Micol 27: 80-89. [Crossref]
- Meis JF, Kullberg BJ, Pruszczynski M, Veth RP (1994) Severe osteomyelitis due to the zygomycete Apophysomyces elegans. J Clin Microbiol 32: 3078-3081. [Crossref]
- Hamill RJ (2013) Amphotericin B Formulations: A Comparative Review of Efficacy and Toxicity. Drugs 73: 919-934. [Crossref]
