Journals
Heterologous Breast Reconstruction in A Patient with Autoimmune Panniculitis
A B S T R A C T
Breast reconstruction in patients affected by collagenopathy and/or panniculopathy is often challenging. In most cases, heterologous reconstruction is avoided due to the low extensibility of skin and subcutaneous tissues. As a consequence, flaps were regarded as work-horses to reconstruct such patients. However, autologous breast reconstruction implies donor-site morbidity, longer surgery and increased risk of post-operative complications. Moreover, the patient may be reluctant to undergo such a complex procedure. We report the case of a 61 year-old woman, affected by autoimmune diffuse panniculitis who successfully underwent two-stage heterologous breast reconstruction following unilateral mastectomy. At 12 months follow-up no complication occurred. In our experience, by slightly modifying the expansion protocol, two-stage heterologous breast reconstruction proved to be a reliable option in patients with panniculopathy.
K E Y W O R D S
Breast, Heterologous, Mastectomy, panniculopathy, reconstruction
Case Report
Panniculitis is an inflammatory process involving the subcutaneous fat. Clinically, it presents with nodular, erythematous skin areas, oedema and, occasionally, and formation of secreting tracts [1]. These areas are mainly localised to thighs, buttocks and trunk. The association between panniculitis and other pathologies such as dermatomyositis and connective tissue disorders was previously reported [2]. In women undergoing mastectomy, the range of therapeutic possibilities for breast reconstruction is severely limited by autoimmune connective tissue disorder and/or panniculopathy, thus requiring accurate pre-operative planning. In most of these cases, the concerns about poor wound healing, low extensibility of skin and subcutaneous tissues lead the surgeon to perform an autologous reconstruction, mainly pedicled flaps [3]. Aiming to share our experience in this field, we report the case of a woman, affected by autoimmune panniculitis, who underwent heterologous breast reconstruction following unilateral mastectomy.
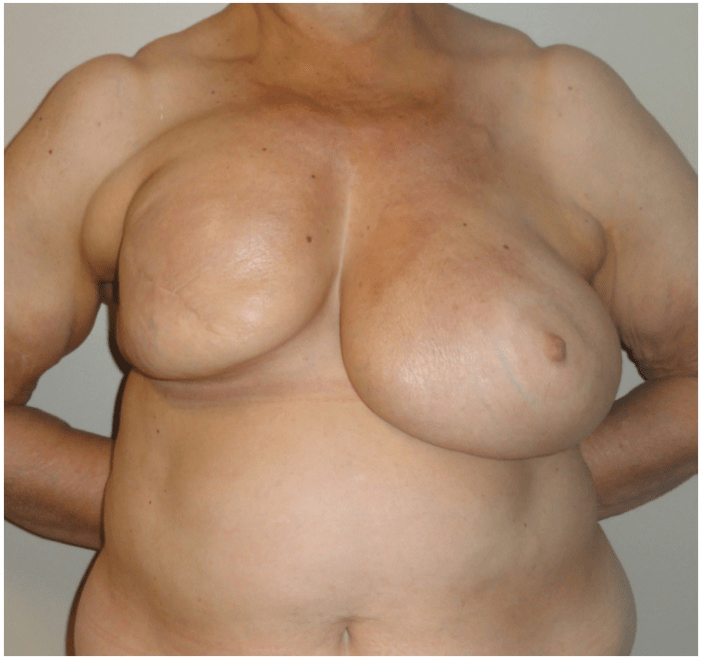
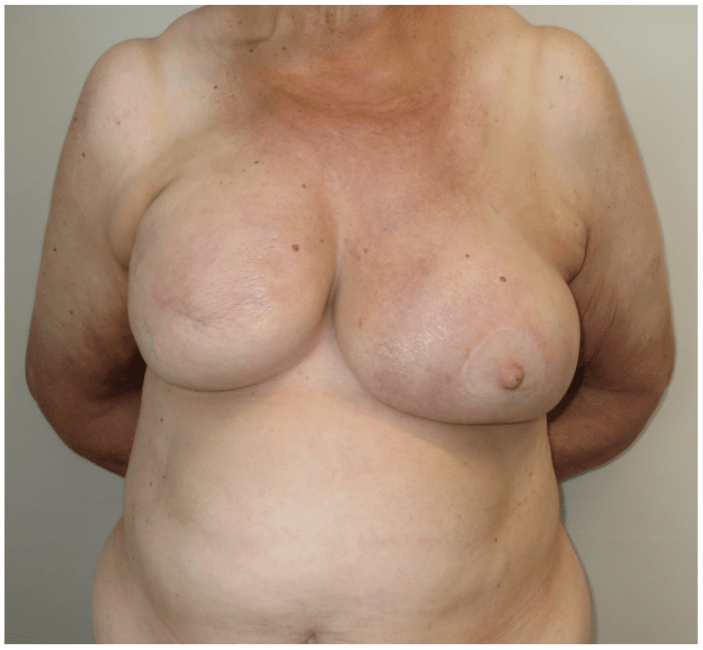
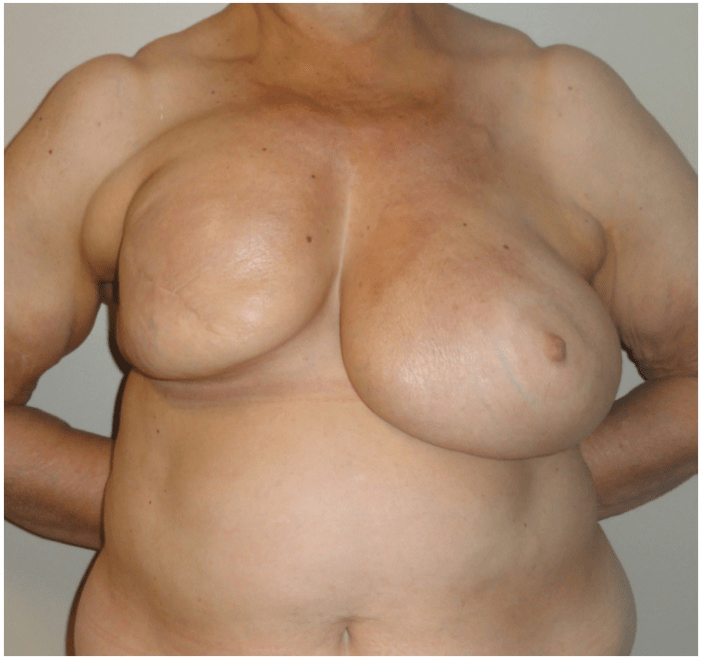
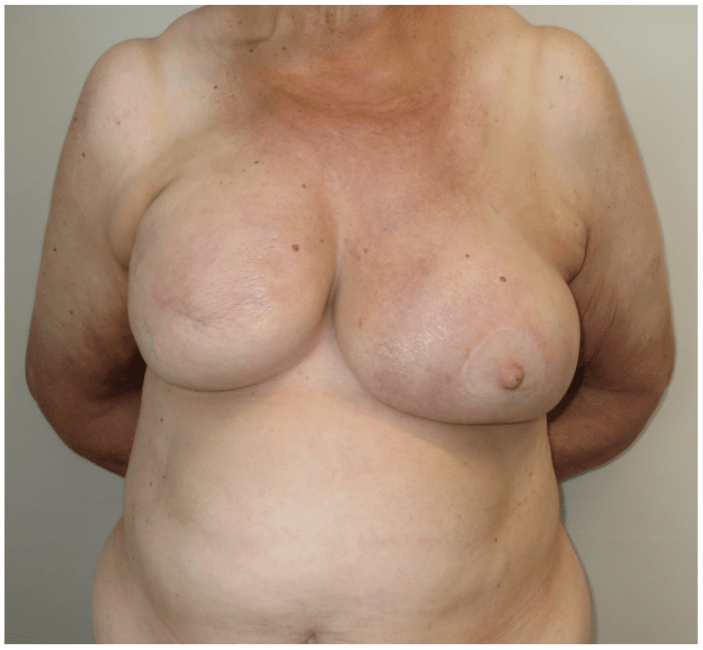
A 61-year-old woman affected by diffuse autoimmune panniculitis mainly involving the superior mammary quadrants, was referred to our Breast Unit following the diagnosis of breast cancer with axillary lymph node involvement (Figure. 1, left). Once informed about the different reconstructive techniques, the patient refused autologous reconstruction, concerned by donor-site morbidity, longer surgery and the increased risk of post-operative complications. As a consequence, two-stage heterologous reconstruction was planned. Preoperatively, she underwent a cycle of anti-rheumatoid medications. Right-sided mastectomy and axillary lymphadenectomy to Fisher level 3 were performed and, in the same operative stage, a 700 cm3 tissue expander was placed in a sub-musculofascial pocket beneath pectoralis major, pectoralis minor and serratus anterior muscles. Prior to insertion, the expander was intra-operatively expanded by 20% of its volume with 140 cm3 of saline solution. Starting on the 15th post-operative day, the patient underwent expansion cycles. Four limited expansions were performed due to the concurrent inflammation of the subcutaneous fat: the average volume for each cycle was 95 cm3 (13.6% of the total volume) and there was a prolonged average interval of 12 days between each expansion. The overall final volume expansion was 520 cm3 (74.3% of the total volume). Expansion cycles were then stopped for six months, during which the patient underwent chemotherapy. Subsequently, 6 months after the last expansion, two further 90 cm3 expansions (12.9% of the total volume) were performed with a 14-day interval between each one, thus achieving complete filling of the expander (Figure. 1, middle). Twenty months after the last expansion, the patient underwent the second stage of breast reconstruction with the placement of a 685 g textured silicone gel prosthesis. Contralateral symmetrisation was achieved by mean of superior pedicle breast reduction with inverted-T scar. At 12-month follow-up, no complication was experience, with no evidence of implant infection, haemorrhage, seroma formation, dehiscence of the surgical wound, breast tissue ischaemic necrosis (Figure. 1, right). The patient was satisfied with the aesthetic outcome.

Breast reconstruction can be challenging in patients suffering from collagenopathy or associated panniculopathy, as therapeutic options can be significantly restricted. To date, large-scale epidemiologic studies have not found any credible association between silicone breast implants and either well-defined connective tissue diseases or undefined or atypical connective tissue diseases [4]. To our knowledge, there are few reports in literature that can be used to guide decision-making in such cases. Specifically, the presence of a connective tissue disease, as well as the associated panniculopathy, are often considered an indication for autologous breast reconstruction. Autologous breast reconstruction can be a reliable option in these patients because it allows to avoid the complications deriving from the placement of a foreign body in over-reactive damaged tissues, such as extrusion, further tissue derangement and wound healing complications. These considerations are paramount in patients who also need radiotherapy. Nevertheless, autologous breast reconstruction is more difficult to perform, implies donor-site morbidity and requires longer operative time and longer hospitalization. In cases of panniculitis, patient’s own tissues may not be qualitatively adequate for breast reconstruction; moreover, when systemic connective tissue diseases are present, clotting dysfunction and severe hypercoagulable state may contra-indicate autologous techniques [5]. The psychological burden of the patient is a further factor, often underestimated, that drives the choice of the reconstructive technique. Indeed, patients diagnosed with breast cancer often suffer from psycho-emotive lability and may be reluctant to undergo an autologous breast reconstruction, being concerned by its possible complications. Consequently, such as in our case, they may refuse this kind of procedures and prefer the draw-backs of implant placement, such as the need for 2 surgeries. In this context, heterologous reconstruction provides reduced operative time and well-tolerated, easy-to-perform surgeries. Generally, heterologous breast reconstruction requires an initial intra-operative expansion of 20% of the expander volume, followed by expansions of an average of 100 cm3 with a 7-10 days interval among them. In our case, we decided to lengthen the interval between expansions and to limit the saline volume injected each time, in order to obtain adequate coverage with gradual tissue distension. This process achieved homogeneous expansion and reduced tissue tension, thus allowing to perform, 20 months after the last expansion, the second stage with a silicon-based prosthesis and concurrent symmetrisation of the contralateral breast. It must also be emphasised that the use of silicone gel breast implants has been demonstrated not to induce or favour the onset of connective tissue disorders, most of all rheumatoid arthritis and SLE [4]. Through this case, we would like to report and underline the possibility of heterologous breast reconstruction in patients affected by autoimmune panniculopathy. By ensuring good surgical technique and appropriate time between expansions, the risk of complications can be dramatically reduced.
The available approaches for post-mastectomy breast reconstruction are limited when patients suffer from connective tissue disorders or panniculopathy. Autologous breast reconstruction can be limited by patients’ comorbidities and concerns. In our experience, delaying the interval between expansions proved to be safe when performing breast heterologous reconstruction in patients suffering from autoimmune panniculitis.
Authors Contribution
All authors contributed to conception and design, manuscript preparation, read and approved the final manuscript.
Funding
No funding was received for this work. The authors do not have any financial interest or commercial association with subject matter and/or products mentioned in the manuscript.
Competing interests
None
Conflict of interests
None
Article Info
Article Type
Case ReportArticle History
Received 7 September 2018Accepted 3 October 2018
Published 25 October 2018
Copyright
© 2018 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.03.008
Author Info
Corresponding author
Francesco Segreto“Campus Bio-Medico di Roma” University, Via A. del Portillo 200, 00128, Rome, Italy
Figures & Tables

References
1. Zannis J, Wood BC, Griffin LP, Knipper E, Marks MW, et al. (2012) Outcome study of the surgical management of panniculitis. Ann Plast Surg 68: 194-197. [Crossref]
2. Girouard SD, Velez NF, Penson RT, Massarotti EM, Vleugels RA (2012) Panniculitis associated with dermatomyositis and recurrent ovarian cancer. Arch Dermatol 148: 740-744. [Crossref]
3. Chin KY, Chalmers CR, Bryson AV, Weiler-Mithoff EM (2013) Breast reconstruction in the high-risk patient with systemic connective tissue disease: a case series. J Plast Reconstr Aesthet Surg 66: 61-66. [Crossref]
4. Hölmich LR, Lipworth L, McLaughlin JK, Friis S (2007) Breast implant rupture and connective tissue disease: a review of the literature. Plast Reconstr Surg 120: 62S-69S. [Crossref]
5. Mioton LM, Smetona JT, Hanwright PJ, Seth AK, Wang E, et al. (2013) Comparing thirty-day outcomes in prosthetic and autologous breast reconstruction: A multivariate analysis of 13,082 patients? J Plast Reconstr Aesthet Surg 66: 917-925. [Crossref]
