Hemostasis Surgery of Spontaneous Hemothorax Complicating Neurofibromatosis Type 1
A B S T R A C T
Vascular lesions in Von Recklinghausen’s disease also known as Neurofibromatosis type 1 (NF1), are rare but have a fatal and potentially life threatening complications such as spontaneous hemothorax. An emergent thoracotomy is indicated when there is an active bleeding associated unstable hemodynamic status. Despites surgery is laborious and unpredictable but it have a merit to stop hemorrhage. A conservative management with endovascular embolization or non-operative approach have also been reported in case of hemodynamic stability. We report two case report of spontaneous hemothorax in patient with Recklinghausen disease. A chest tube was immediately inserted for two patients. Due to continuous bleeding and hemodynamic instability (Patient 1), and the increase of pleural effusion volume (Patients 1 & 2), emergent surgery of thorax was done with favourable post-operative follow up.
Keywords
Hemothorax, neurofibromatosis, surgery
Introduction
Neurofibromatosis type 1 (NF1), or Von Recklinghausen’s disease, is autosomal dominant disorder and has an incidence of 1/3000 [1, 2]. This disease is characterized by ‘tache café au lait spots’, it can also manifest as any type of neurofibroma, characteristic bone lesions, optic nerve glioma [2-4]. Vascular involvement is rare but particularly serious due to its complications. Lesions of the vessels can be stenoses, occlusions, arteriovenous malformations, aneurysms and pseudoaneurysms complicated by spontaneous rupture with a major risk of bleeding [1, 3, 4]. We present two cases of spontaneous and sudden hemothorax occurring in a woman and a man carrying (NF1). In fact, we demonstrate the primordial place of emergency hemostasis surgery in the management of this vascular complication fatal disease.
Case 1
A 52-year-old Tunisian patient with known NF 1, admitted on the pneumology department for left basithoracic pain with acute dyspnea. The physical examination noted a blood pressure (10/6 mm Hg), polypnea (24c/min) and a syndrome of left fluid effusion. He had a skin and mucous membrane paleness, several café-au-lait spots and plexiform neurofibromas on the trunk, limbs. The chest X-ray showed moderate left pleural effusion. The blind pleural puncture brought back a blood fluid. The biological assessment reveals deglobulization with a haemoglobin that goes from 11 to 9 g/dl. A control chest X-ray showed an increase in the left pleural effusion hence an emergent CT scan showed a massive hemothorax with mediastinal deviation to the contralateral side and shows an enlargement of the central spinal canal and left foramina extended from T1 to T4 probably related to neurofibromas.
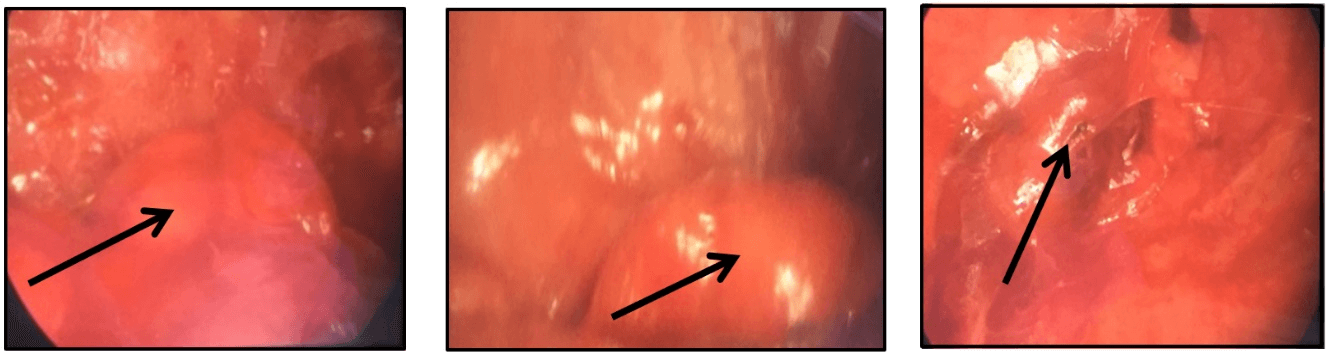
A chest tube was inserted and 2000 ml of blood was removed in 3 hours. Given to an unstable hemodynamic status, it was decided to operate the patient in emergency through a left video-assisted posterolateral minithoracotomy. Intraoperative exploration noted ten neurofibromas scattered over the parietal pleura (Figure 1). A neurofibroma next to the 5th left rib was bleeding in a sheet. The patient had a clot removal with an embodiment of the hemostasis electrocoagulation injury. The immediate postoperative course was favourable. The postoperative course was favourable with a 24-month decline.
Figure 1: Per-operative exploration showing pleural neurofibroma.
Case 2
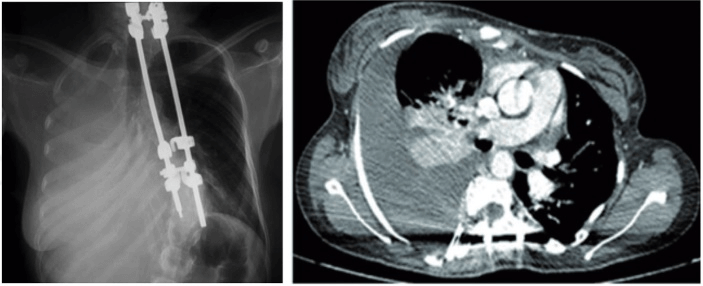
A 32-year-old women, operated on ten years previously for scoliosis with implantation of prosthetic material, carrier of Recklinghausen’s disease presenting a benign thoracic trauma occurring 5 days previously presented for right chest pain. Physical examination noted right pleural effusion syndrome with ‘café-au-lait’ spots on the trunk. The chest X-ray shows a moderate abundance of pleural effusion. The puncture of which brings back bloody fluid. The follow-up X-ray after puncture shows an increase in the effusion (Figure 2). These findings were confirmed by a CT scan a which shows a right pleural effusion of great abundance but it is failed to show an evident source of bleeding (Figure 2).
Figure 2: Chest X-ray and Chest CT showing an massive right pleural effusion.
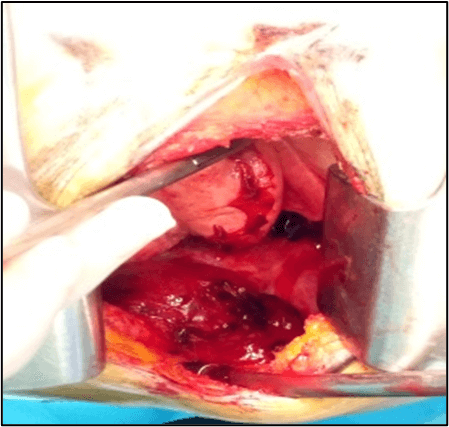
Figure 3: Per-operative exploration showing pleural neurofibroma.
Laboratory investigations showed a deglobulization with haemoglobin which drops to 6.7 g/dl, with a relative hemodynamic stability. The patient was transferred to the thoracic surgery department where a emergent chest tube was inserted and which brought back 1500 ml of blood over 24 hours. We evaluated that the patient was in a stable condition and the follow-up chest X-ray shows partial regression. The following day, surgical exploration were performed by a right video-assisted postero-lateral minithoracotomy. We have removed 1000 ml of black blood fluid with electrocoagulation of the lesion which was at the origin of the bleeding. This lesion was located opposite the 5th intercostal space on the parietal pleura, it was a vascular lesion at the expense of the intercostal artery (Figure 3) which could be a vascular dysplasia or pseudoaneurysm.
Intraoperative exploration noted an unusual extreme vascular fragility with hyperhemorrhagic intercostal vessels. We performed hemostasis with an electric scalpel and we make a ligation with Vicryl on the intercostal vessels with the installation of an absorbable hemostatic. The postoperative outcome was favourable with ablation of the chest drains on the 5th postoperative day. The patient was seen after 16 months of the operation with a correct follow-up X-ray.
Discussion
According to the conference of the National Institutes of Health in Bethesda in the United States, the diagnosis of Von Recklinghausen disease is made by combining 2 criteria among the following: a first degree relative with NF1, the presence of 6 café-au-lait spots, 2 neurofibromas or 1 plexiform neurofibroma, axillary or inguinal lentigines, two Lisch nodules, characteristic bone lesions, glioma of the optic pathways [2, 5]. The incidence of vascular disease in case of NF1 is rare (3.6%), but by serious complications [3, 4]. The rapidly acute character, the increase of the effusion after pleural puncture bringing back an haematic fluid as well as the deglobulization were major arguments in favour of the diagnosis of hemothorax. In addition, in 2nd patient we mentioned the possibility of triggering bleeding by pinning of a neurofibroma by the prosthetic material, especially since it describes a minimal thoracic trauma 5 days before symptoms. Faced with hemodynamic instability, deglobulization and thoracic drainage that continues to bring a blood it was decided to opt for a surgery for the two cases. The difficulty of the management was the need of an emergent surgical exploration without knowing the exact origin of the bleeding in the context of a major arterial fragility [5, 6].
The hemothorax, occasional revelation or complication of (NF1), is a medical and surgical emergency potentially fatal situation [1, 4]. According to the literature, postoperative mortality reached (40%) [1]. This lethal manifestation of (NF1) is mainly due to either spontaneous vascular erosion or bleeding from a degenerated hyper-vascularized neurofibroma [1]. In some cases, an iatrogenic cause or a trauma may be suggested and can causes a rupture of a neurofibroma or vascular injury previously uncomplicated. The predominant locations of vascular lesions in NF1 are the subclavian artery and intercostal arteries and internal mammary arteries [1, 3, 4]. Spontaneous hemothoraxes in (NF 1) are due to two main factors, namely the fragility of the arterial wall on the one hand and spontaneous primary hemostasis disorders on the other hand [3, 4].
A chest X-ray can detect pleural effusion. An emergent CT scan with contrast has a prominent place in the diagnostic and management if hemothorax associated with NF1 [3]. It allows to confirm the diagnosis, assess the abundance of the effusion and its impact, identify the source of bleeding [5]. In addition, CT scan allows searching a hypervascular thoracic tumor mass that might be complicated by hemothorax. After evaluation of hemodynamic and biologic status of patient, all imaging finding are used to plan the steps of the therapeutic approach (Chest tube and/or endovascular treatment and/or surgery) [3]. The management for a hemothorax associated with NF1 depends mainly on the stability of hemodynamic status. In cases of hemorrhagic shock and/or major hemodynamic instability, extreme emergency hemostasis surgery is required [4]. If on hemodynamic stability, it is enough of a conservative treatment first intention. Thus, a chest drainage urgently evacuates the effusion, to avoid a compression of mediastinal structure by increasing of the hemothorax and especially to monitor the rate of bleeding flow. The radiography control after drainage and flow schedule thoracic drainage allow to indicate or not secondarily surgery.
Endovascular embolization, which is not always available, recently considered by many teams as the treatment of choice in cases of major bleeding but provided an identification accurate by imaging the bleeding vessel and hemodynamic stability [3]. Surgery may be proposed later to evacuate the hematoma or failure of interventional treatment [1]. Surgical hemostasis is having the merit to clarify the exact etiology of bleeding and to stop it in the same time. For our first patient, the most plausible cause of the hemothorax was a spontaneous bleeding from the pleural neurofibromas and regarding to our second patient, it was a rupture of small vessels dysplastic fragile at that was possibly triggered by the trauma. The conduct for the two patients was an emergency chest drainage. Then after consultation with the anaesthesia team, we decided an emergency thoracotomy given the vital prognosis involved within 4 hours following the installation of the drain for our first patient who was hemodynamically unstable with an hourly flow rate of haematic liquid greater than 200 cc / hour. For our second patient, the evolution was marked by a relative stability on the hemodynamic status with a decreasing hourly flow of haematic fluid removed, that said we opted for a surgical exploration the following day. The surgery was performed in delayed emergency after a blood transfusion.
Conclusion
All Recklinghausen’s disease patient who is presenting with a pleural effusion haematic and rapid hemodynamic deterioration should be suspected hemothorax associated with this disease. An early diagnosis of this serious chest complication is essential to prevent its lethal consequences. The decision of the therapeutic strategy involves the participation of several stakeholders (anaesthesiologists, endoscopists, radiologists and thoracic surgeons). Recently, endoscopic treatment has been recommended by several teams in certain situations, but surgery remains the best which at the same time allows to know exactly the lesion at the origin of the hemothorax and to stop radically the bleeding.
Author Contributions
All authors have participated in i) conception and design, or analysis and interpretation of the data; ii) drafting the article or revising it critically for important intellectual content and iii) approval of the final version.
Conflicts of Interest
I. The authors have no affiliation with any organization with a direct or indirect financial interest in the subject matter discussed in the manuscript.
II. The following authors have affiliations with organizations with direct or indirect financial interest in the subject matter discussed in the manuscript:
i. Abdennadher Mahdi: Service de Chirurgie Thoracique et Cardiovasculaire
ii. Ben Saad Soumaya: Service de Pneumologie (C), Hôpital Abderahmen-Mami
iii. Zribi Hazem: Service de Chirurgie Thoracique et Cardiovasculaire
iv. Zairi Sarra: Service de Chirurgie Thoracique et Cardiovasculaire
v. Bouassida Imen: Service de Chirurgie Thoracique et Cardiovasculaire
vi. Marghli Adel: Service de Chirurgie Thoracique et Cardiovasculaire
Article Info
Article Type
Case ReportPublication history
Received: Tue 22, Dec 2020Accepted: Mon 01, Feb 2021
Published: Fri 19, Feb 2021
Copyright
© 2023 Abdennadher Mahdi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2021.01.01
Author Info
Abdennadher Mahdi Ben Saad Soumaya Zribi Hazem Zairi Sarra Bouassida Imen Marghli Adel
Corresponding Author
Abdennadher MahdiEl-Manar University, Tunisia
Figures & Tables
References
- Pulivarthi S, Simmons B, Shearen J, Gurram MK (2014) Spontaneous hemothorax associated with neurofibromatosis type I: A review of the literature. J Neurosci Rural Pract 5: 269-271. [Crossref]
- Miura T, Kawano Y, Chujo M, Miyawaki M, Mori H et al. (2005) Spontaneous Hemothorax Recklinghausen's Disease in Patients with von Recklinghausen's Disease. Jpn J Thorac Cardiovasc Surg 53: 649-652. [Crossref]
- Hongsakul K, Rookkapan S, Tanutit P, Pakdeejit S, Songjamrat A et al. (2013) Spontaneous massive hemothorax in a patient with neurofibromatosis type 1 with successful transarterial embolization. Korean J Radiol 14: 86-90. [Crossref]
- Miyazaki T, Tsuchiya T, Tagawa T, Yamasaki N, Nagayasu T (2011) Spontaneous Hemothorax Associated with von Recklinghausen’s Disease: Report of a Case 2011. Ed Commit Ann Thorac Cardiovasc Surg.
- Aizawa K, Iwashita C, Saito T, Misawa Y (2010) Spontaneous rupture of an intercostal artery in a patient with neurofibromatosis type 1. Interact Cardiovasc Thorac Surg 10: 128-130. [Crossref]
- Saad SB, Abdenadher M, Attia M, Daghfous H, Tritar F (2018) White hemithorax in a young women carrying coffee and milk spots. Rev Pneumol Clin 74: 100-103. [Crossref]
