Glass Removed During Endoscopic Prepatellar Bursectomy
A B S T R A C T
Foreign body objects could be a cause of prepatellar bursitis. This is the only reported case in the literature describing prepatellar bursitis caused by a glass foreign body and the use of endoscopy to retrieve it. During an endoscopic bursectomy to alleviate symptoms of prepatellar bursitis, glass was discovered. The glass was removed and the prepatellar space irrigated and debrided to removed inflamed tissue. This case highlights the only case report of prepatellar bursitis caused by a retained foreign body and the use of endoscopy to remove it. Endoscopic bursectomy is a viable alternative to open bursectomy to minimize wound complications and allow faster recovery.
Keywords
Prepatellar Bursitis, glass, foreign body, endoscopy, bursectomy
Introduction
The prepatellar bursa is located subcutaneously and positioned anteriorly to the patella [1]. Its function includes reducing frictional forces and enhancing gliding of tissue over the patella. When the prepatellar bursa is irritated it becomes inflamed which can produce a decrease in range of motion and elicit pain. The most common etiologies of prepatellar bursitis include acute trauma, atraumatic and chronic irritation. Acute traumatic origin of prepatellar bursitis can develop from direct force applied to the bursa disrupting its anatomical function. Atraumatic causes of bursitis include inflammatory conditions such as gout and rheumatoid arthritis as well as pyogenic-producing conditions such as syphilis, tuberculosis and septic arthritis caused by Staphylococcus aureus. Chronic irritation-causing inflammation of the bursa can be the result of repetitive microtraumatic episodes, such as kneeling, or unresolved atraumatic causes [2]. This case discusses the occurrence of prepatellar bursitis as a result of a foreign body.
Case Report
A 60-year-old male presented initially to our Orthopaedic clinic with primary complaint of left knee swelling and pain. He accidentally kneeled on a broken glass bottle that fell off the shelf while cleaning and stocking shelves as a grocery clerk three weeks prior to presentation. The following day he noticed diffuse swelling of his left kneecap and subsequently developed diffuse bruising of his entire leg. Bruising resolved after one week but the swelling persisted. He also complained of left knee tenderness with applied pressure. The pain was a constant steady pain that was 6/10, achy, worse with kneeling, and improved with rest and aspirin. He denied any constitutional symptoms. Patient initially sought treatment with his primary care physician and then was referred to our clinic for further evaluation.
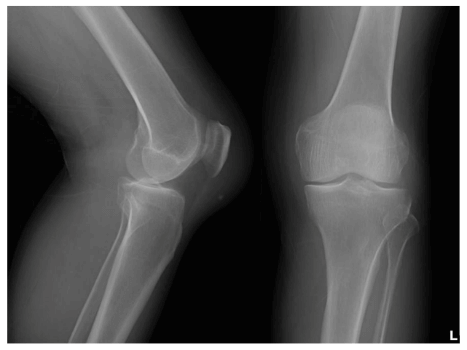
On examination, patient did not have an antalgic gait. He had a 1 cm scar and edema over the anterior aspect of left knee. There was diffuse tenderness of the anterior knee and prepatellar bursa. He had full range of motion and strength. He had negative anterior drawer sign, Lachman’s, posterior drawer sign, valgus and varus stress tests. Radiographs of his left knee showed a large prepatellar soft tissue swelling and a small 4.3 mm radiopaque foreign body in the inferior prepatellar soft tissue region (Figure 1). Assessment at that time was that the patient had prepatellar bursitis due to a foreign body. We decided to perform an aspiration of the left knee prepatellar bursa in clinic due to its large effusion. 30 mL of bloody fluid (hematoma) was aspirated with an 18-gauge needle. Patient was instructed to avoid strenuous activity. He was also instructed to obtain a MRI of the left knee to further evaluate the foreign body. He returned a week later reporting the swelling had returned.
Figure 1: Radiographs revealed a 4.3 mm radiopaque foreign body in the inferior prepatellar soft tissue, along with a large prepatellar soft tissue swelling
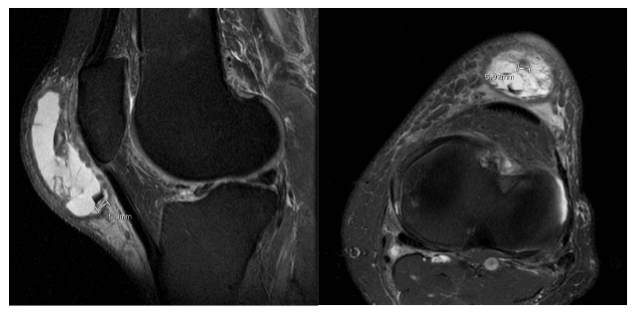
Figure 2: MRI (Proton Density Fat Saturated) Sagittal and Axial views showed septated prepatellar bursa with fluid and foreign body which measured approximately 6 mm
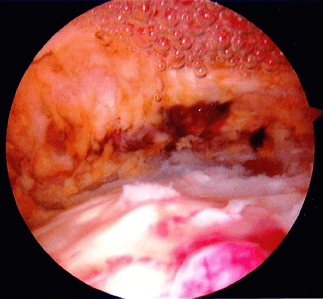
Figure 3: Endoscopic view of thickened, inflamed bursa
We aspirated the prepatellar bursa a second time and obtained 50 mL of serosanguineous fluid. With his MRI still pending, he returned two weeks later reporting the swelling had returned a couple days after the last aspiration. The patient reported minimal improvement and recurrent swelling despite wearing knee pads, applying compressive wrap, and taking nonsteroidal anti-inflammatory drugs (NSAIDs). His MRI was obtained showing a large prepatellar bursa with fluid and a questionable foreign body within the bursa (Figure 2). Because of the retained foreign body and recurrent prepatellar bursitis causing difficulty kneeling and affecting his work, we recommended surgical excision of the bursa with removal of the foreign body.
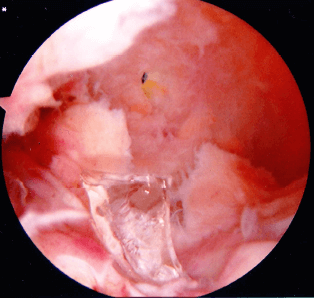
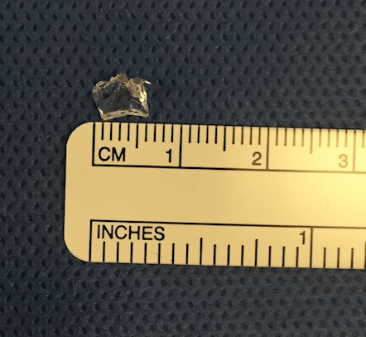
Three weeks later, patient underwent endoscopic prepatellar bursectomy under general anesthesia. Preoperative antibiotics were given. We exsanguinated and inflated the tourniquet to 250 mmHg. Inferolateral, inferomedial and superolateral portals were established to gain access to the prepatellar bursa. We introduced the arthroscope and saw thickened, inflamed bursa (Figure 3). We then proceeded to use the shaver to remove the bursa. As we were sweeping the most inferior aspect of the prepatellar bursa, we came across a piece of glass incidentally which we removed (Figure 4). The glass measured 0.6 cm in length (Figure 5). We let the tourniquet down and hemostasis was obtained. We placed a 10-French Hemovac drain through the arthroscope into the superolateral portal to decrease the risk of postoperative hematoma. Clean dressings were applied. Patient was instructed to weight bear as tolerated and begin range of motion immediately. He was scheduled to come to clinic to remove the drain on postoperative day two. He was placed on aspirin for deep venous thrombosis prophylaxis.
Patient returned on postoperative day two reporting minimal pain. He was ambulatory without any assistive device and required no pain medications. He was monitoring his drain output and recorded 5 mL over the past 24 hours. We decided to pull the drain. On exam, the incision was clean, dry and intact. His left knee had swelling and expected tenderness diffusely. His range of motion and strength were full. We advised him to change dressings daily and apply ACE wrap. He was instructed to return to work with light duties with restriction from kneeling. Two weeks later, patient returned for follow up. He reported mild swelling in the prepatellar bursa without pain and discomfort. He described pain occurring only at night in his thigh and leg. Otherwise, he was able to work and perform his normal activities of daily living. On exam, he had mild prepatellar effusion. There was no tenderness. Range of motion and strength were full. We examined his left thigh and leg but did not find any induration, swelling, erythema, tenderness, nor palpable cord. We believed this could have been related to the tourniquet use during surgery and decided to observe his symptoms. He was instructed to continue compressive wrapping to decrease the swelling. He returned six weeks postoperatively for routine follow up. He reported complete resolution of pain. He still had a prepatellar effusion, which improved significantly compared to his last visit. He was instructed to continue compressive wrapping as needed. Patient was told to follow up in six weeks, but he never returned.
Figure 4: Glass discovered during endoscopic shaving of prepatellar bursa
Figure 5: Glass measured 0.6 cm in length
Discussion
There have been cases of glass foreign bodies discovered in the knee joint [3-6]. However, there is no case written in the literature that reports of a glass foreign body causing prepatellar bursitis. This patient’s history and physical exam clued into the etiology of his prepatellar bursitis. In addition, its radiopacity on radiographs further narrowed which type of foreign body. We decided to initially treat his prepatellar bursitis conservatively with aspirations, modified activities, compressive wrapping, and NSAIDs. Most aseptic prepatellar bursitis respond to conservative treatment. However, if the prepatellar bursitis is recalcitrant to conservative therapy, bursectomy would be the next plan of management [1]. His effusions recurred so we elected to perform an endoscopic bursectomy instead of an open bursectomy to decrease wound complications and allow faster recovery as described by Ogilvie-Harris et al. and Huang et al. [7, 8]. Patient was able to recover uneventfully with no pain nor tenderness at the six-week follow up. He was able to return to pre-injury level of work and activities. He had full knee range of motion and strength. However, he had a mild prepatellar effusion. We presumed that the swelling eventually resolved with compressive wrapping since the six-week postoperative visit was the last follow up and the patient never returned. This is the only documented case in the literature reporting prepatellar bursitis caused by a glass foreign body. In addition, this is the only case in the literature reporting the successful use of endoscopic bursectomy to remove a glass foreign body.
Acknowledgement
We thank Dr. Kermit Crowder, M.D. from Howard University Hospital Radiology Department for reviewing the MRI images and narrowing good sequences to illustrate the prepatellar bursitis and glass foreign body.
Disclosure
No funds were received in support of this work. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript. The authors declare that they have no conflict of interest.
Statement of Informed Consent
The patient was informed that data concerning the case would be submitted for publication and the patient agreed.
Article Info
Article Type
Case ReportPublication history
Received: Sun 29, Sep 2019Accepted: Mon 14, Oct 2019
Published: Mon 15, Jun 2020
Copyright
© 2023 Thomas X. Nguyen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.05.10
Author Info
Shelton A. McKenzie Thomas X. Nguyen William J. Hill
Corresponding Author
Thomas X. NguyenDepartment of Orthopaedic Surgery, Orthopaedic Resident, Howard University Hospital, Washington, D.C.
Figures & Tables
References
- Aaron DL, Patel A, Kayiaros S, Calfee R (2011) Four common types of bursitis: diagnosis and management. J Am Acad Orthop Surg 19: 359-367. [Crossref]
- Roland GC, Beagley MJ, Cawley PW (1992) Conservative Treatment of Inflamed Knee Bursae. Phys Sportsmed 20: 66-77. [Crossref]
- Devgan A, Mudgal KC (2007) An unusual case of foreign body knee that spontaneously migrated inside and out of the joint: arthroscopic removal. Knee Surg Sports Traumatol Arthrosc 15: 758-760. [Crossref]
- Hafez MA, Al-Dars AM (2012) Glass foreign bodies inside the knee joint following intra-articular injection. Am J Case Rep 13: 238-240. [Crossref]
- Murugharaj SS, Kerketta AH (2016) An unusual case of partial Anterior Cruciate ligament (ACL) tear secondary to a glass foreign body in an adolescent knee joint. J Orthop Case Rep 6: 13-15.
- Sharma S, Rampurada A, Rees AJ (2007) A glass foreign body in the knee joint mistaken for ACL avulsion: an unusual case. Knee Surg Sports Traumatol Arthrosc 15: 766-768. [Crossref]
- Ogilvie-Harris DJ, Gilbart M (2000) Endoscopic bursal resection: the olecranon bursa and prepatellar bursa. Arthroscopy 16: 249-253. [Crossref]
- Huang YC, Yeh WL (2011) Endoscopic treatment of prepatellar bursitis. Int Orthop 35: 355-358. [Crossref]
