Fibrous Dysplasia of the Frontal Sinus Presenting with Periorbital Emphysema
A B S T R A C T
Fibrous dysplasia (FD) is an uncommon non-malignant bony tumor in which normal bone is replaced by disorganized fibro-osseous tissue. It most often involves the femur, ribs, and craniofacial skeleton and is commonly diagnosed in adolescence or early adulthood. Involvement of the paranasal sinuses is rare, and there is a relative paucity of case reports in the literature. Here, we report a case of FD of the frontal sinus in a 22-year-old male initially presenting with acute onset periorbital emphysema after nose-blowing. Radiographic examination revealed an expansile lesion with “ground-glass” appearance. The patient underwent resection and reconstruction by combined endoscopic and external approach with osteoplastic flap by a multidisciplinary team. The diagnosis of FD was confirmed by permanent histopathology. This report reviews the presentation and treatment of FD of the paranasal sinuses and details a combined external and endoscopic approach to resection of the frontal sinus mass.
Keywords
Fibrous dysplasia, bony tumor, paranasal sinuses, frontal sinus
Background
Fibrous dysplasia (FD) is a rare, non-malignant, slowly progressive tumor of bony origin in which normal bone is replaced by fibrous tissue due to failure of normal osteogenesis [1]. The two traditional classifications of fibrous dysplasia are polyostotic, involving multiple dysplastic foci and accounting for 15-30% of cases, and the more common monostotic form with one disease focus [2, 3]. Fibrous dysplasia accounts for a small minority (5-7%) of all benign bone tumors [3]. McCune-Albright syndrome is a rare subtype of the polyostotic form associated with precocious puberty and café-au-lait macules [4].
Craniofacial involvement is reported to be present in 50% of polyostotic cases and 27% of monostotic cases, but is considered by many to be a unique variant of FD that may best be described as monostotic, as it often involves contiguous bones of the craniofacial skeleton [5]. Involvement of the paranasal sinuses has been only rarely reported [6-9]. We report the case of a 22-year-old man presenting with periorbital edema and subcutaneous emphysema found to have frontal sinus fibrous dysplasia.
Case Report
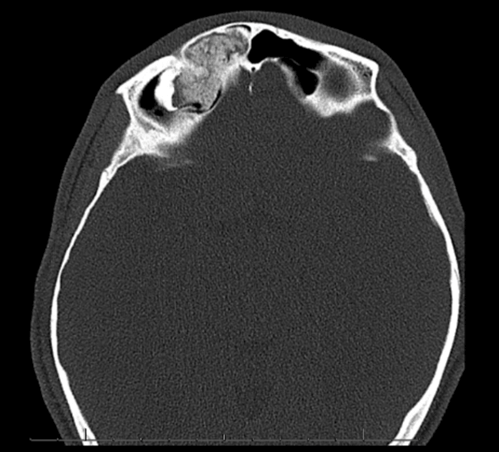
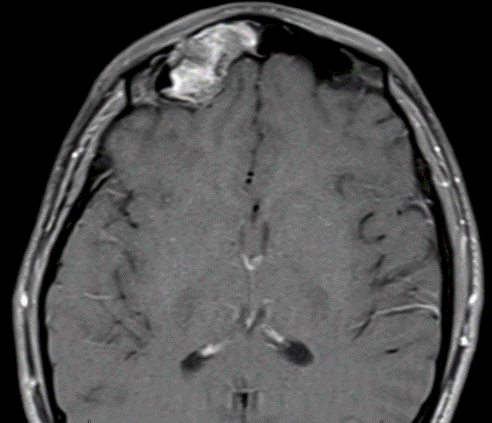
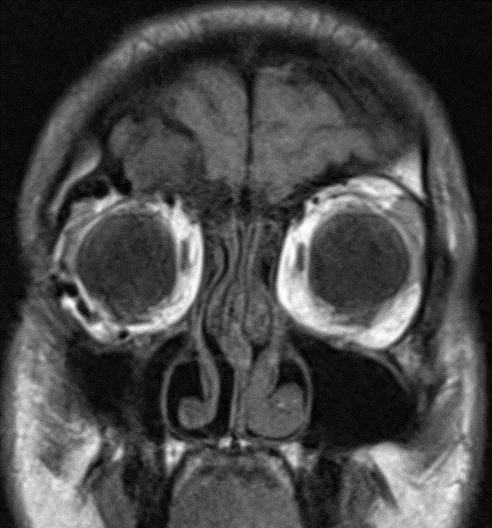
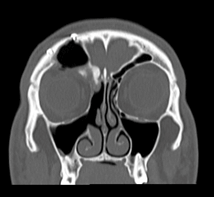
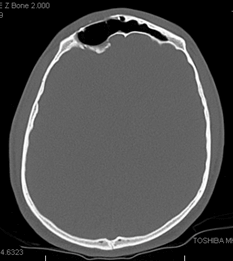
A 22-year-old male Air Force Cadet presented to the emergency department with a report of right periorbital swelling after blowing his nose. He had no previous medical history and denied any preceding headache, visual changes, or facial trauma. On examination in the emergency department, he was noted to have right periorbital swelling and diplopia on superior gaze, but otherwise had a normal exam without focal neurological deficits. A maxillofacial CT was performed and demonstrated soft tissue emphysema of the preseptal and extraconal fat of the right orbit. Within the right frontal sinus was a 3.9 cm “ground-glass” expansile bony mass with erosion of the superior orbital wall (Figures 1 & 2). MRI with contrast for further characterization redemonstrated this right frontal sinus expansile mass of osteogenic origin, and showed heterogeneous enhancement (Figures 3 & 4). The patient was referred to ENT for urgent follow-up and was discharged from the ED in stable condition with nose-blowing precautions. Given the size, location, and extensive expansile nature of the mass, the patient was seen by a rhinologist, facial plastic surgeon, and oculoplastic surgeon.
Figure 1: Preoperative coronal facial CT.
Figure 2: Preoperative axial facial CT.
Figure 3: Preoperative axial post-gadolinium MRI.
Figure 4: Preoperative coronal post-gadolinium MRI.
The differential diagnosis was felt to include an osteoma, ossifying fibroma, fibrous dysplasia, and malignancy. A multidisciplinary surgical plan was made for an open approach, utilizing an osteoplastic flap (OPF) technique and endoscopic resection of the mass with orbital roof and anterior frontal table reconstruction. At the time of surgery, a bicoronal flap was raised in a subgaleal plane down to the superior orbital rim. As no pericranial flap was planned, the pericranium was incised above the site of the expected superior osteotomy. The pericranium was then elevated inferiorly to adequately expose the frontal bone.
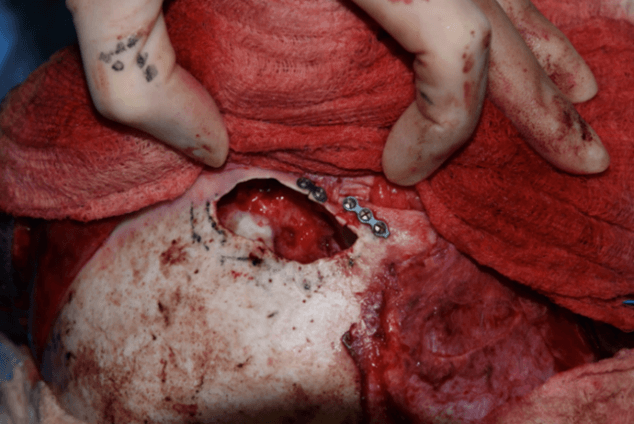
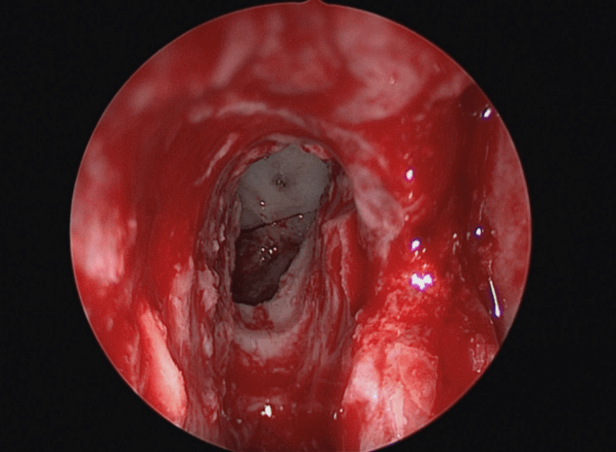
Figure 5: Intraoperative view of frontal sinus.
Mapping of the anterior frontal table osteotomies was carefully completed using the Medtronic (Minneapolis, MN) Fusion™ ENT Navigation System with concurrent endoscopic transillumination. An Anspach drill (DePuy Synthes, West Chester, PA), with 4 mm cutting burr was used to ‘postage-stamp’ the anterior table along the proposed osteotomy. A sagittal saw was used, beveled at 30 degrees, to create the osteotomies which were then carried into the supraorbital rim along the lateral and medial aspects of the frontal sinus. Osteotomies around the supraorbital foramen and nerve were completed to enable complete exposure of the superior orbit. The anterior table was then separated from the underlying bony mass. The mass was fixed and required slow dissection from superior-anterior and transorbital approaches, using a combination of Kerrison rongeurs, Anspach drill with cutting burrs, and the Sonopet ultrasonic aspirator (Stryker, Kalamazoo, MI) for areas adjacent to the periorbita and posterior table. Further dissection and removal of the mass revealed the site of origin to be a broad area along the medial frontal recess extending inferiorly and posteriorly along the fovea ethmoidalis. Removal of the mass resulted in a significant area of demucosalized bone within the frontal recess (Figure 5).
Due to concerns for right frontal recess stenosis, the frontal intersinus septum was removed. At this time, the endoscopic trans-nasal approach was performed, which included right-sided maxillary antrostomy, anterior ethmoidectomy, and Draf IIb frontal sinusotomy. The additional bony mass within the anterior ethmoid along the fovea ethmoidalis was drilled down. A cuff of bony mass was left intact in the area in an attempt to avoid cerebrospinal fluid fistula. At the completion of the endoscopic resection, the frontal sinusotomy was widely patent (Figure 6). The orbital roof defect was reconstructed with 1 mm thickness porous polyethylene (Medpor, Stryker, Kalamazoo, MI). The supraorbital rim was reconstructed using 0.5 mm miniplates. The osteoplastic flap was replaced and secured with mini plates, and the bicoronal incision was closed in layers.
Figure 6: Endoscopic intraoperative view of the right frontal sinusotomy.
The patient’s post-operative recovery was uneventful. He reported normal visual acuity, denied diplopia, and had no evidence of CSF leak. Permanent pathology was consistent with fibrous dysplasia without evidence of malignancy. At three months post-operatively there was no suggestion of frontal sinus outflow obstruction. He tolerated an in-clinic valsalva maneuver without evidence of orbital emphysema. CT scan two months post-operatively showed soft tissue density within the right frontal recess, but no evidence of residual mass and well-aerated common frontal sinus (Figures 7 & 8).
Figure 7: Post-operative coronal facial CT.
Figure 8: Post-operative axial facial CT.
Discussion
Craniofacial FD is an uncommon histologically benign disease that infrequently affects the craniofacial bones. FD is thought to be caused by a somatic activating point mutation in the GNAS gene (guanine nucleotide-binding protein), which encodes a stimulatory G protein. The downstream effect of this mutation is sustained activation of adenylate cyclase and increased production of cyclic AMP (adenosine monophosphate). These cellular changes cause increased cell proliferation, impairment of proper transition of bone-forming mesenchyme to mature osteogenic cells, and increased osteoclast activity resulting in increased bone resorption [1]. This activating mutation thus results in a disorganized fibrotic bone matrix.
Fibrous dysplasia does not appear to have a genetic predilection, except when associated with McCune-Albright Syndrome. This syndrome represents 3% of FD, is more commonly found in females, and is characterized by associated café-au-lait macules and precocious puberty [10]. FD is classified as monostotic (70-85%) or polyostotic (15-30%), but craniofacial FD (CFD) is often considered a variant of monostotic, as it involves contiguous bones in the craniofacial skeleton [11]. The most commonly reported locations for FD are the proximal femur, rib, and craniofacial bones [12]. Amongst patients with CFD, the mandible and maxilla are most commonly affected, and the majority of these lesions are unilateral [13]. Involvement of the paranasal sinuses is infrequent, but when present, is most often seen in the sphenoid sinus, followed by ethmoid and maxillary sinuses [14].
FD most commonly affects patients in the first to third decades of life, with most patients diagnosed in adolescence or early adulthood [15]. The most common clinical signs of CFD are swelling or deformity at the primary site. Functional impairment depends on the region of involvement [12]. Frontal, ethmoid, maxillary, or sphenoid involvement may cause symptoms of nasal obstruction, facial pain, ostial outflow obstruction and subsequent sinusitis-like symptoms. Involvement of the orbit or cranial base can produce compression of the optic nerve and resultant visual complaints [1]. Proptosis, epiphora, headache, and facial paresthesia can also be seen. CT imaging is the preferred modality for the diagnosis of FD. The lesion generally appears to be expansile and is either homogeneously sclerotic in appearance or displays a ground-glass pattern of radiolucent and radiodense areas [16]. There is often thinning of the cortical bone [17]. MRI may reveal a heterogeneous mass that enhances with gadolinium-based contrast [1].
Our patient’s imaging demonstrated the typical ground-glass appearance on CT, but was also consistent with the appearance of an ossifying fibroma and osteoma. Differentiating these masses based on imaging is challenging, though ossifying fibroma often appears as a well-defined multi-loculated mass with a dense rim and is the least common of these three fibro-osseous lesions [1]. Osteoma, the most common benign tumor of the paranasal sinuses, often appears as a homogeneous mass that is well-circumscribed by defined margins [18]. Our patient’s mass appeared consistent with an osteoma on imaging and in the operating room, but on permanent histology, it was found to be fibrous dysplasia.
Because FD is not a malignant or highly locally aggressive disease, the objectives of surgical resection in this case included improving facial deformity and sinus outflow obstruction with the removal of the majority of the mass, rather than radical and complete resection. In the case of quiescent FD without continued growth and in the absence of facial deformity, observation is considered an acceptable approach. However, in our case, the patient’s occupation as a pilot increased his need for a functional frontal sinus. Furthermore, his continued intermittent periorbital swelling and diplopia in the months following the initial presentation made continued observation inappropriate.
Surgical resection of frontal sinus masses can be completed through both endoscopic and/or external approaches with an OPF. The endoscopic approach alone is limited by the lateral extent of the mass within the frontal sinus. In this case, the mass extended laterally beyond the mid-pupillary line and therefore necessitated a combined open and endoscopic approach. The bicoronal approach and OPF achieved wide exposure of the frontal sinus and superior orbit. Transorbital exposure limited the risk of intraorbital complications and facilitated reconstruction of the superior-lateral orbital roof. Following subtotal removal of the mass through the open approach, an endoscopic technique allowed for improved removal of residual tumor inferiorly and posteriorly along the fovea ethmoidalis.
There are several aspects of our patient’s case that are unique. His lack of any headache, facial pain, or sinusitis-like symptoms prior to the day of his presentation is surprising given the complete occlusion of his frontal sinus and outflow tract by the bony mass. In addition, his presenting symptom of acute onset periorbital edema and emphysema after sneezing has not been previously reported in the presentation of FD. Orbital emphysema is a rare occurrence in the absence of facial trauma, though it has been previously noted to occur secondary to nose blowing [19]. Our patient’s orbital swelling resolved spontaneously and was not noted to recur post-operatively. An additional consideration is the patient’s occupation as a military pilot. Every precaution was taken intraoperatively to avoid CSF leak, including purposefully leaving a small cuff of FD along the attachment site of the fovea ethmoidalis. The possibility of frontal recess stenosis from the removal of the mucosa during mass excision and/or growth of residual FD over time influenced the decision to remove the frontal intersinus septum.
In conclusion, we describe a case of fibrous dysplasia of the frontal sinus presenting initially with periorbital emphysema after sneezing. Fibrous dysplasia is a rare disease and is infrequently found in the paranasal sinuses. This case report adds to the limited body of literature that describes fibrous dysplasia of the paranasal sinuses. We advocate for pre-operative MRI and CT imaging, use of image guidance intra-operatively, and combined open and endoscopic technique by a multidisciplinary team involving otolaryngology (rhinology and facial plastics) and oculoplastics when appropriate. Our patient underwent combined endoscopic and open surgical resection with orbit, superior orbital rim, and frontal table reconstruction and had an uncomplicated post-operative course with return to flying.
Data Availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 15, Feb 2021Accepted: Mon 01, Mar 2021
Published: Wed 17, Mar 2021
Copyright
© 2023 Emily S. Misch. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.03.10
Author Info
Christina Stevens Emily S. Misch Anne Getz Eric Hink Adam Terella
Corresponding Author
Emily S. MischDepartment of Otolaryngology, University of Colorado School of Medicine, Aurora, Colorado, USA
Figures & Tables

References
1. Nicolai P (2015) Cummings Otolaryngology. Benign Tumors of the Sinonasal Tract. Saunders.
2. Rahman AM, Madge SN, Billing K, Anderson PJ, Leibovitch I et al. (2009) Craniofacial fibrous dysplasia: clinical characteristics and long-term outcomes. Eye (Lond) 23: 2175-2181. [Crossref]
3. Hakim DN, Pelly T, Kulendran M, Caris JA (2015) Benign tumours of the bone: A review. J Bone Oncol 4: 37-41. [Crossref]
4. Robinson C, Collins MT, Boyce AM (2016) Fibrous Dysplasia/McCune-Albright Syndrome: Clinical and Translational Perspectives. Curr Osteoporos Rep 14: 178-186. [Crossref]
5. Couturier A, Aumaitre O, Gilain L, Jean B, Mom T et al. (2017) Craniofacial fibrous dysplasia: A 10-case series. Eur Ann Otorhinolaryngol Head Neck Dis 134: 229-235. [Crossref]
6. Aygun D, Sahin H (2004) Fibrous dysplasia of the frontal sinus: an uncommon cause of frontal lobe abscess. J Clin Neurosci 11: 904-906. [Crossref]
7. Simovic S, Klapan I, Bumber Z, Bura M (1996) Fibrous dysplasia in paranasal cavities. ORL J Otorhinolaryngol Relat Spec 58: 55-58. [Crossref]
8. Kanda M, Yuhki I, Murakami Y, Hasegawa Y, Kanki T (2002) Monostotic fronto-orbital fibrous dysplasia with convulsion--case report. Neurol Med Chir (Tokyo) 42: 36-39. [Crossref]
9. Feldman MD, Rao VM, Lowry LD, Kelly M (1986) Fibrous dysplasia of the paranasal sinuses. Otolaryngol Head Neck Surg 95: 222-225. [Crossref]
10. McCarthy EF (2013) Fibro-osseous lesions of the maxillofacial bones. Head Neck Pathol 7: 5-10. [Crossref]
11. AaC CA, Ray Y (2018) Tumors of the Facial Skeleton: Fibrous Dysplasia. Elsevier I (ed) Plastic Surgery: Craniofac Head Neck Surg Pediatr Plastic Surg 3: 380-400.
12. Ricalde P, Horswell BB (2001) Craniofacial fibrous dysplasia of the fronto-orbital region: a case series and literature review. J Oral Maxillofac Surg 59: 157-167. [Crossref]
13. Yenigun A, Akyuz S (2015) Isolated fibrous dysplasia of the ethmoid sinus. SAGE Open Med Case Rep 3: 2050313X14568132. [Crossref]
14. Lee JS, FitzGibbon EJ, Chen YR, Kim HJ, Lustig LR et al. (2012) Clinical guidelines for the management of craniofacial fibrous dysplasia. Orphanet J Rare Dis 7: S2. [Crossref]
15. Ameli NO, Rahmat H, Abbassioun K (1981) Monostotic fibrous dysplasia of the cranial bones: report of fourteen cases. Neurosurg Rev 4: 71-77. [Crossref]
16. Chong VF, Khoo JB, Fan YF (2002) Fibrous dysplasia involving the base of the skull. AJR Am J Roentgenol 178: 717-720. [Crossref]
17. AlMomen AA, Molani FM, AlFaleh MA, AlMohisin AK (2020) Endoscopic endonasal removal of a large fibrous dysplasia of the paranasal sinuses and skull base. J Surg Case Rep 2020: rjz404. [Crossref]
18. Exley RP, Markey A, Rutherford S, Bhalla RK (2015) Rare giant frontal sinus osteoma mimicking fibrous dysplasia. J Laryngol Otol 129: 283-287. [Crossref]
19. Mohan B, Singh KP (2001) Bilateral subcutaneous emphysema of the orbits following nose blowing. J Laryngol Otol 115: 319-320. [Crossref]
