Factors in Post-Operative Implant Cervical Burnout: A Retrospective Review
A B S T R A C T
Introduction: The purpose of this study was to evaluate the factors which had the greatest impact on implant cervical bone health. A retrospective review was completed, and various factors were examined. The investigators hypothesized that there is no difference in implant success based on location, brand, or length of the implant.
Methods: A retrospective electronic chart review of patients from the Dental College of Georgia (DCG) was done, looking at a study population composed of all patients who had an implant placed between January 1, 2009, and January 1, 2010. This included any type of dental implant placed at this academic institution, within any of the multiple departments who place implants. Patients were excluded as study subjects if they had the implant placed by another practitioner outside of the DCG. Information including location, brand, timing, age, sex, and complications was examined.
Results: The sample was composed of data extracted from the dental records of 67 eligible study participants. Of these, 63 (94%) had data on bone loss and all results in this paper are based on these 63 patients. The majority of the participants were female (42/63, 67%), and age ranged from 41 to 88 (mean 68.6, SD 12.3, median 70). Significantly more bone loss was found in maxillary implants than in mandibular. This was true for mesial (p = 0.013, Table 1), distal (p = 0.012, Table 2), and average bone loss (p = 0.006, Table 3).
Conclusion: The results of this study suggest a relation between implant length and positioning and bone loss. Future studies will focus on the development of more clinical markers and assessment tools for failure.
Keywords
Implant, marginal bone loss, crestal bone loss, implant failure, thread exposure
Introduction
Implants have become a crucial tool in the restoration of the dentition and complications still abound, which prevent long-term success. The purpose of this study was to evaluate the factors which caused the greatest impact on implant cervical bone health. A retrospective chart review of patients from January 2009-2010 was conducted from patients of the Dental College of Georgia. Variables examined were the implant location, brand, and restoration, as well as patient factors. Statistical analysis was completed using unequal variance t-test and one-way ANOVA with Tukey-Kramer pairwise comparisons to compare groups (gender, brand of implant, etc.) in terms of mean bone loss. Pearson correlation was used to examine the association of continuous correlates with bone loss. All statistical analyses were performed using SPSS Version 21 (IBM Corporation, Armonk, NY, 2012). All significance tests were two-tailed, with a significance level of 0.05. Average bone loss differed significantly between males and females, with males showing a significantly greater bone loss for both mesial and distal surfaces, and greater bone loss was found around maxillary implants when compared to mandibular.
Long-term implant success, from both an aesthetic and a functional perspective, is a multifactorial process [1, 2]. Connective tissues, hard and soft, play a major role in the health of an implant platform and its associated restoration [3]. While bone loss around the crestal portion of an implant within the first year of use is expected, we wanted to determine factors that predict bone loss and overall implant success [4]. Some of the factors which can contribute to bone loss include inappropriate stresses and force distribution, trauma during surgery, micromechanical movement, infection, and multiple other patient factors [5, 6]. Bone loss has not been linked to a single implant type, placement procedure, or specialty, but remains a significant challenge in the long-term success of implants [3]. The purpose of this study was to evaluate the factors which caused the greatest impact on implant cervical bone health. The investigators hypothesize that there is no difference in implant success based on location, brand, or length of implant. The aim of this study is to help identify if specific factors could be isolated and addressed to minimize bone loss.
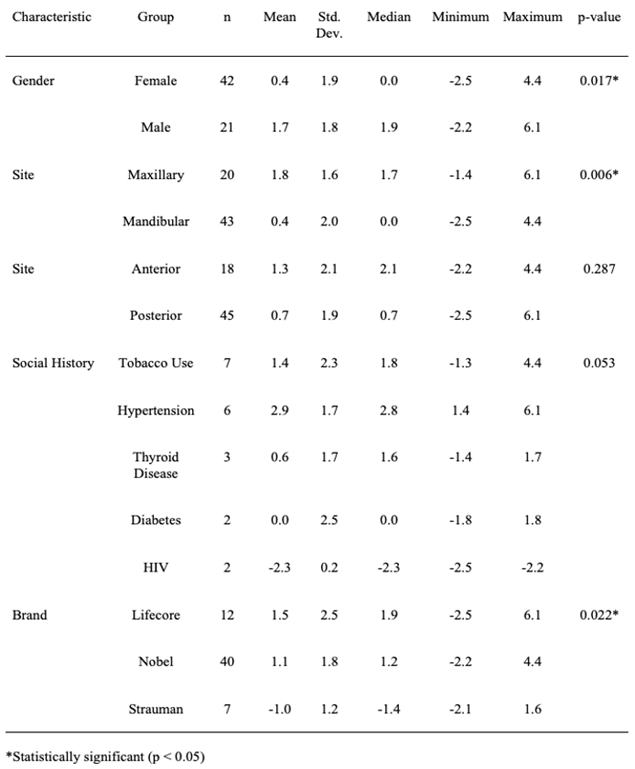
Table 1: Group comparisons for mesial bone loss.
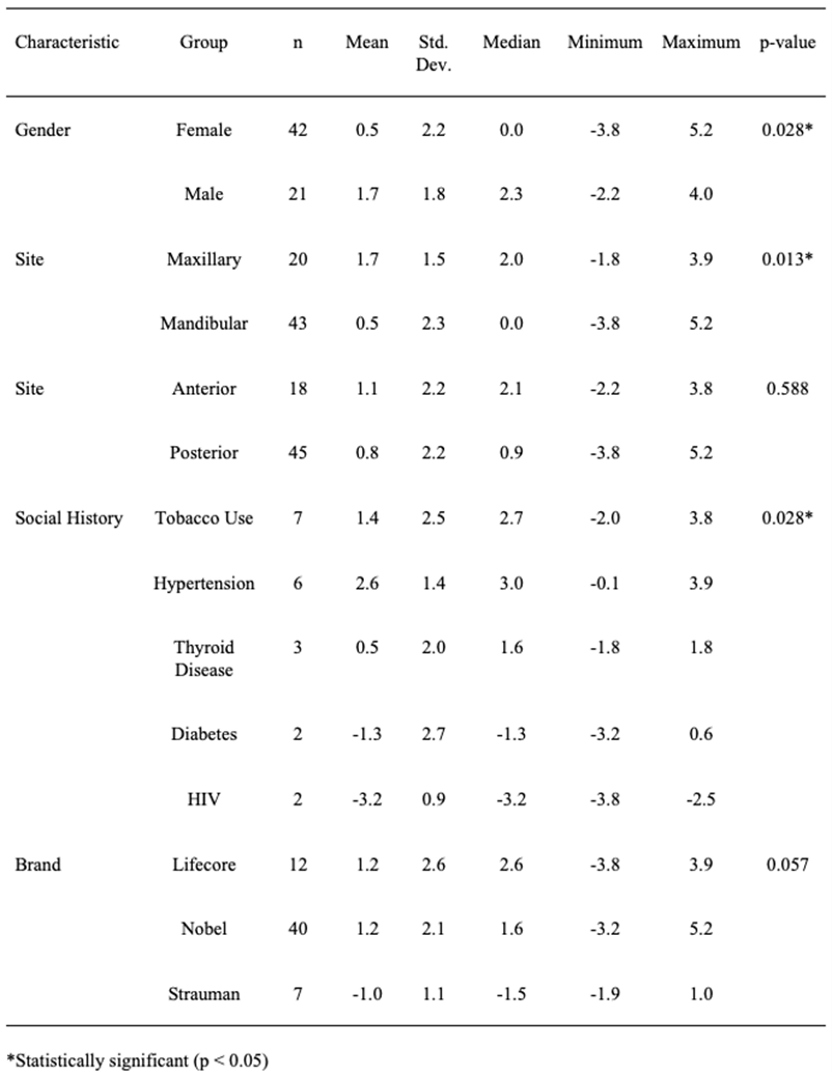
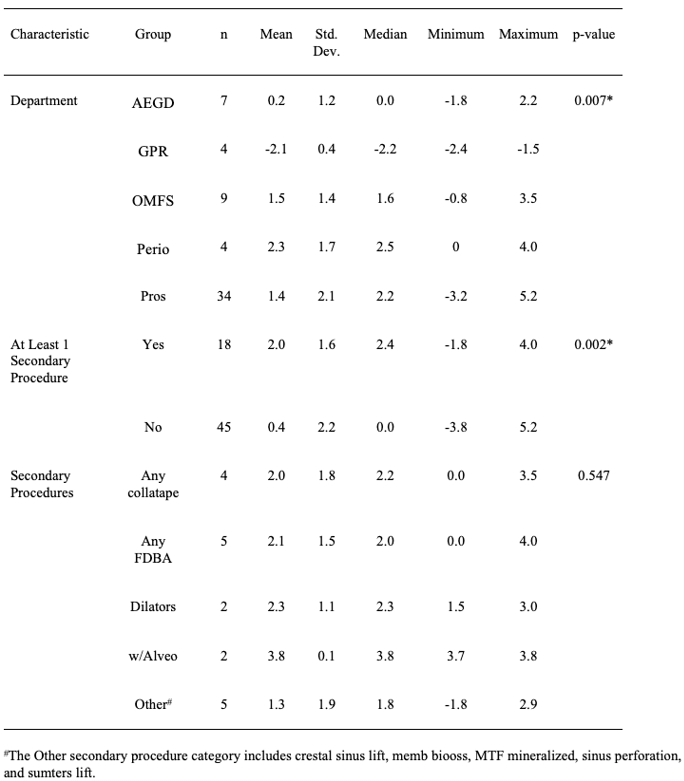
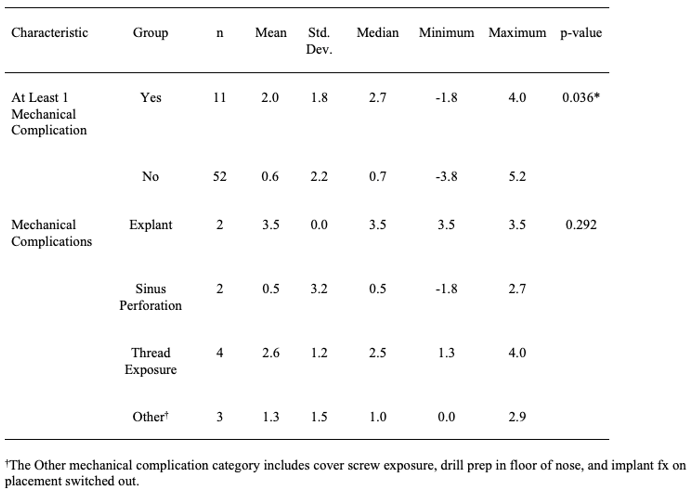
Table 2: Group comparisons for distal bone loss.
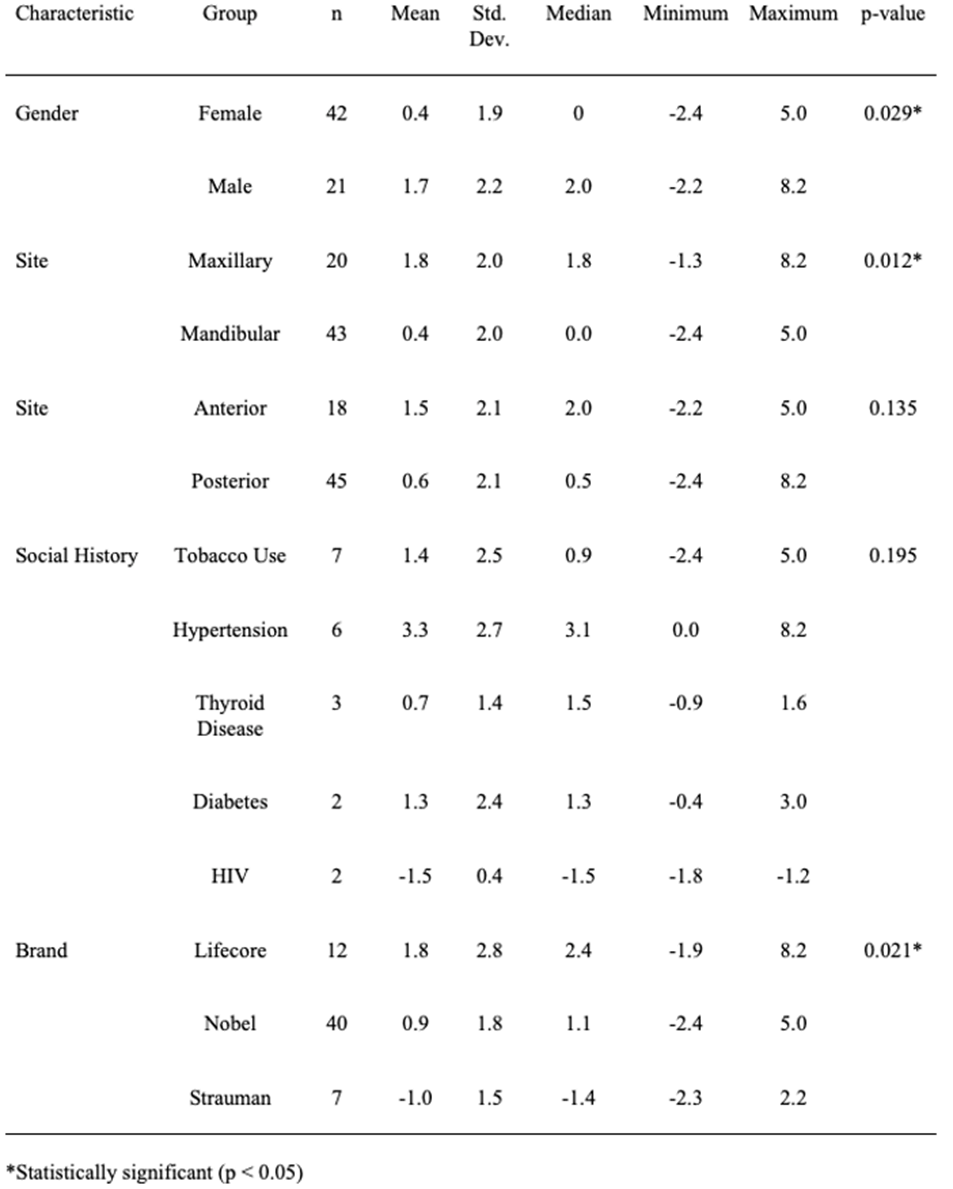
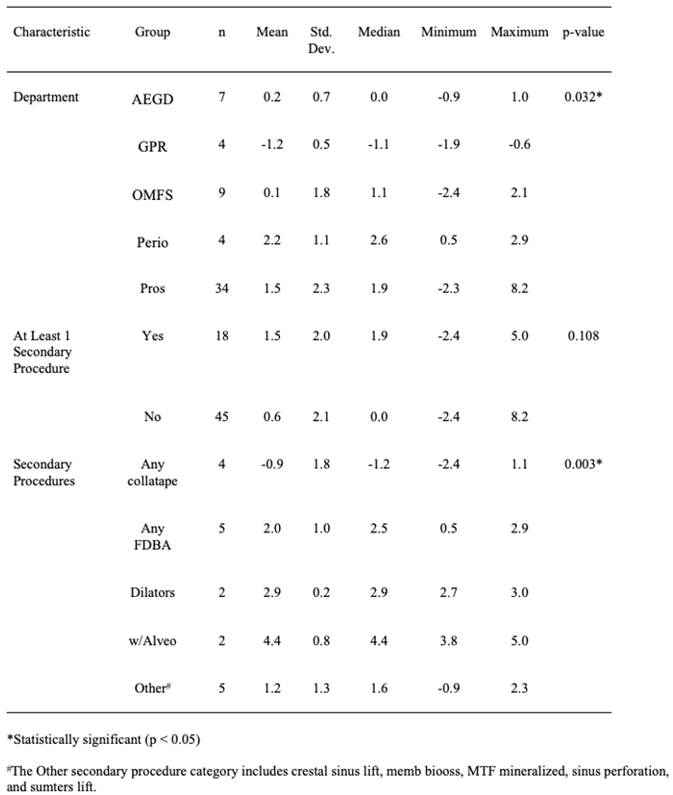
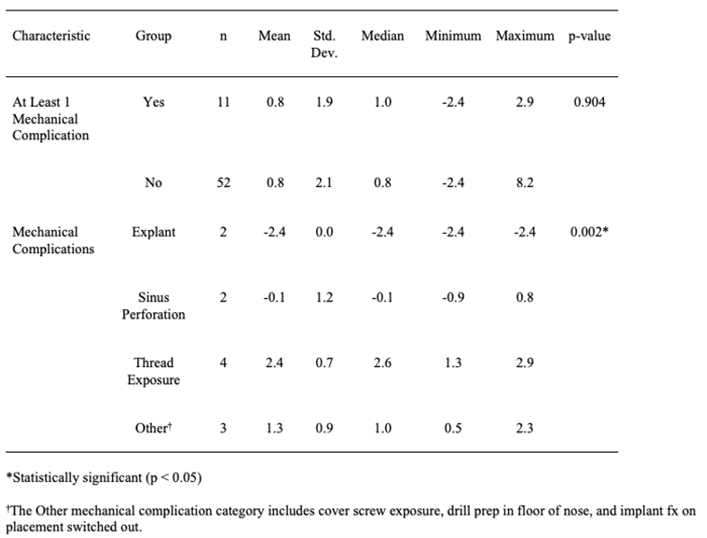
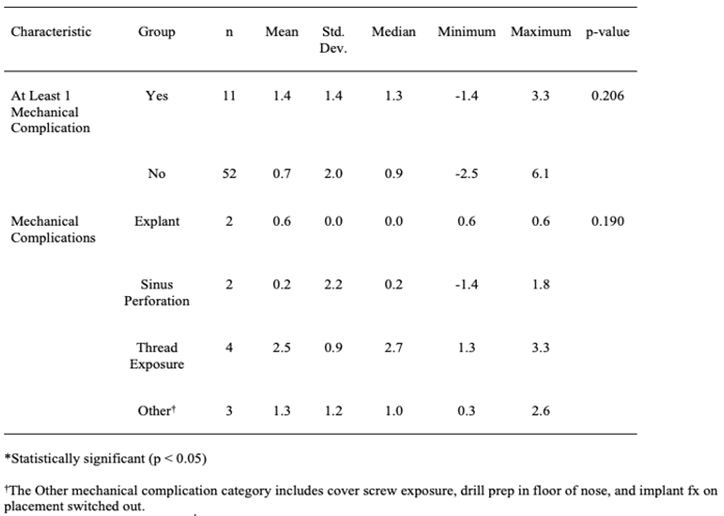
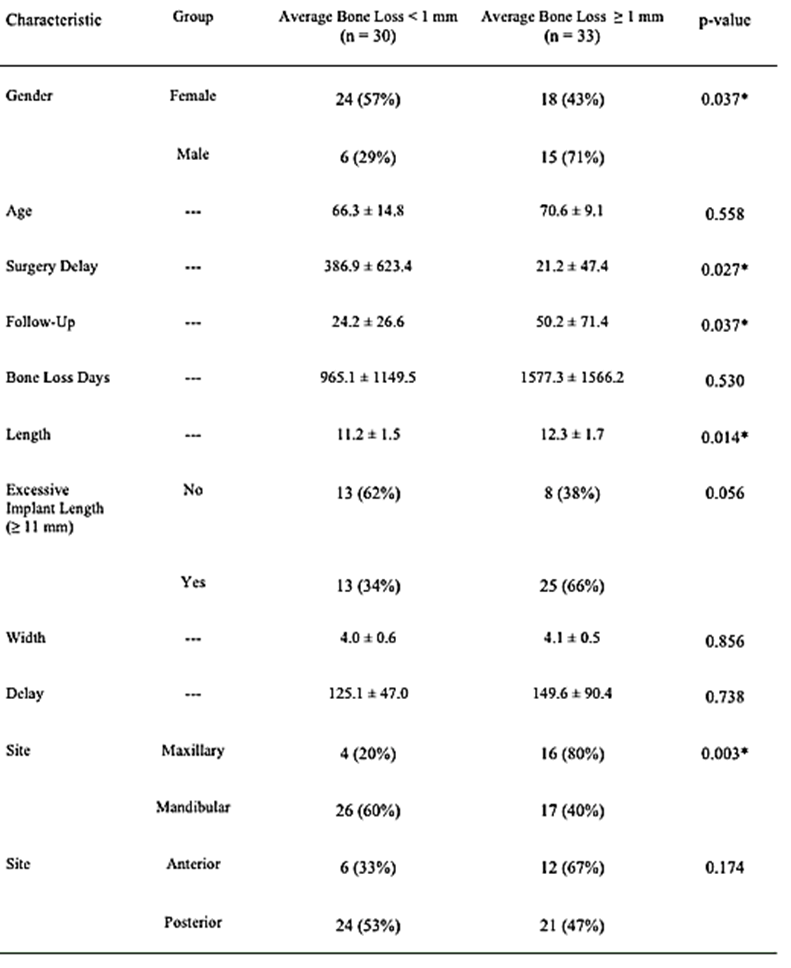
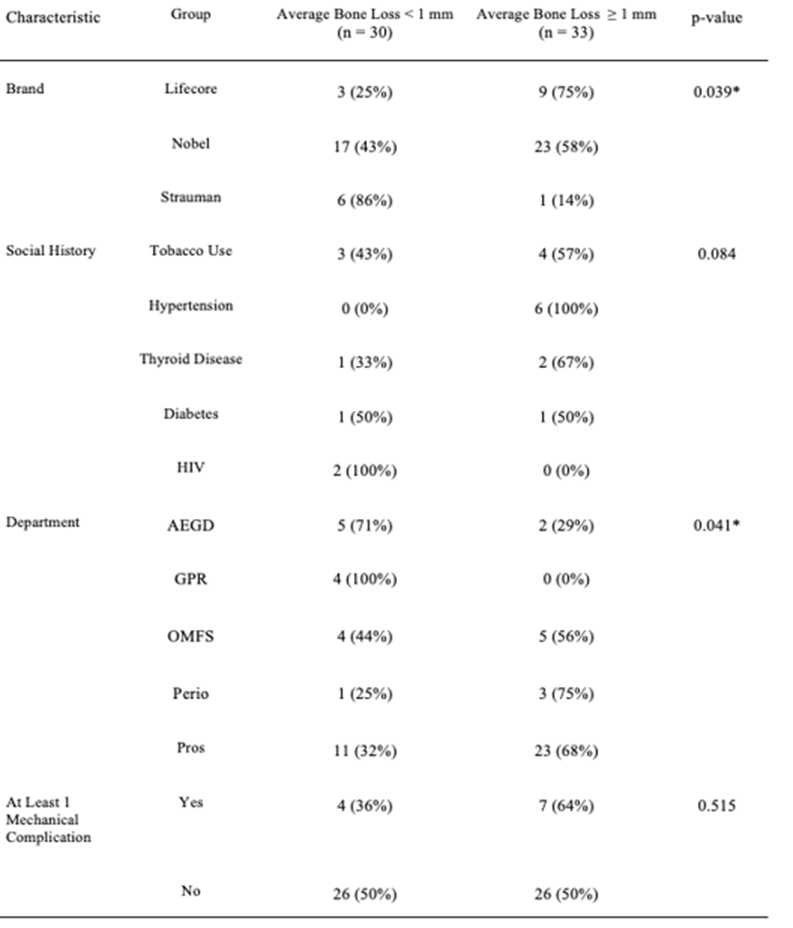
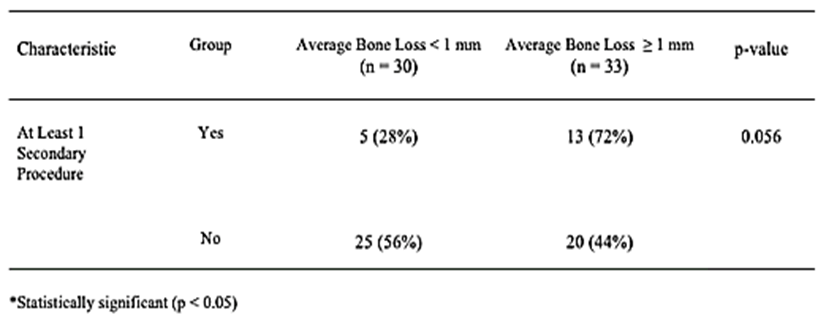
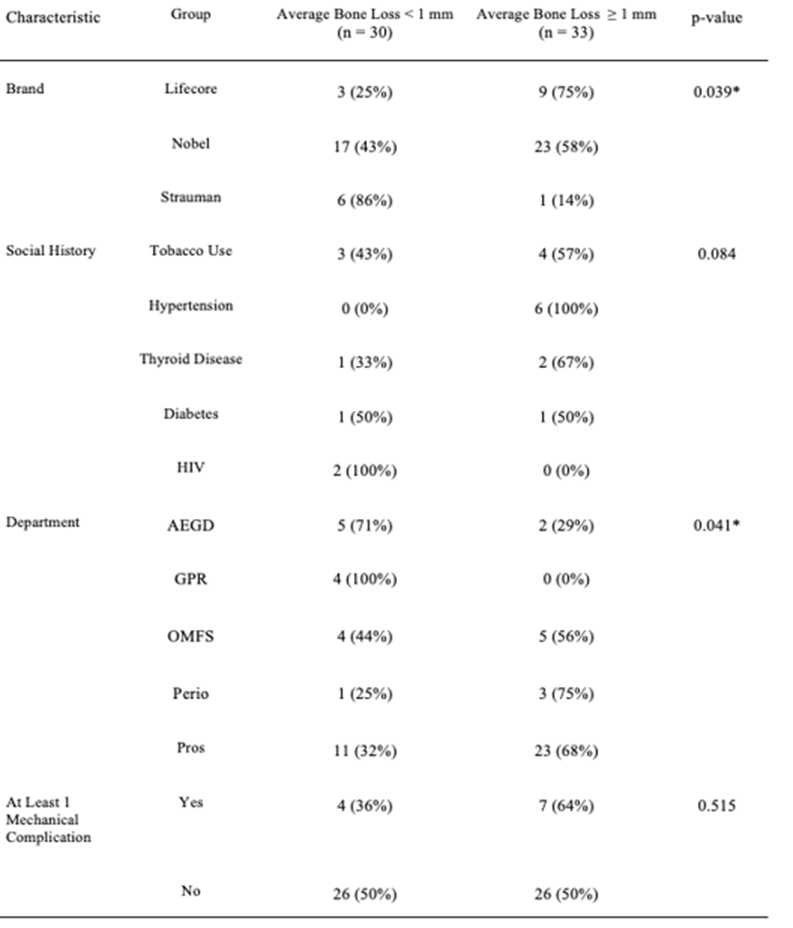
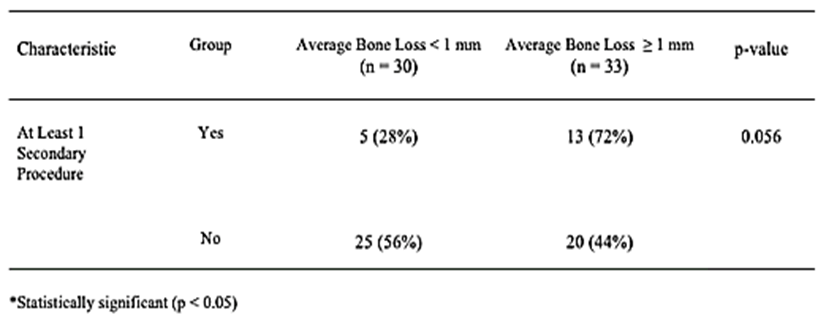
Table 3: Group comparisons for average bone loss.
Methods
To address the research questions, the investigators designed and implemented a retrospective electronic chart review of patients from the Dental College of Georgia (DCG). Due to the retrospective nature of this study, it was granted an exemption in writing by the Augusta University Dental College of Georgia IRB. The study population was composed of all patients who had an implant placed between January 1, 2009, and January 1, 2010. To be included in the study sample, patients had to have any type of dental implant placed at this academic institution, within any of the multiple departments that routinely place implants, to include oral surgery, periodontics, and advanced education in general dentistry. Patients were excluded as study subjects if they had the implant placed outside of the DCG.
Once the patients who had dental implant placement were identified, the following information was extracted from each patient's chart using the electronic medical record:
i. Location of implant
ii. Implant Brand
iii. Extraction date
iv. Implant surgery date
v. Surgery time
vi. Follow-up
vii. Restoration type
viii. Complication-biologic
ix. Complication-mechanical
x. Age
xi. Sex
xii. Specialty
Statistical Analysis
Several correlates of bone loss (mesial and distal) were examined, as well as demographics (gender, age, social history), site of implant (maxillary vs. mandibular and anterior vs. posterior), brand of implant, academic department, or programme in which the implant was performed, length and width of implant, surgery delay (if any), follow-up time, bone loss days, secondary procedures performed, and mechanical complications. We evaluated the same correlates with average bone loss (ABL), defined to be the mean of mesial and distal bone loss. The average bone loss was dichotomized in order to classify each implant as “failed” (ABL ≥ 1 mm) or “successful” (ABL < 1 mm) [7]. This dichotomized outcome was examined for significant associations with each of the correlates mentioned above.
Continuous correlates (age, etc.) were summarized using mean and standard deviation (SD). Categorical risk factors were summarized using frequency and percent. For normally distributed data, the unequal variance t-test and one-way ANOVA with Tukey-Kramer pairwise comparisons were used to compare groups (gender, brand of implant, etc.) in terms of bone loss [3]. The paired t-test was used to compare mesial vs. distal bone loss within patients. If the data were not normally distributed, non-parametric tests were used instead. Pearson correlation was used to examine the association of continuous correlates with bone loss. All statistical analyses were performed using SPSS Version 21 (IBM Corporation, Armonk, NY, 2012). All significance tests were two-tailed, with a significance level of 0.05.
Results
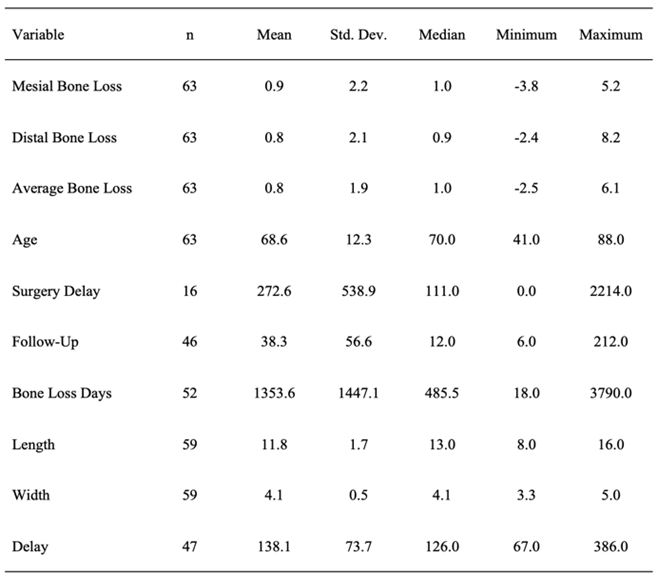
Data was extracted from the dental records of 67 eligible study participants. Of these, 63 (94%) had data on bone loss and all results in this paper are based on these 63 patients. The majority of the participants were female (42/63, 67%) and age ranged from 41 to 88 (mean 68.6, SD 12.3, median 70). Data on bone loss and each of the continuous correlates are summarized for the 63 study participants in (Table 4, Figure 1).
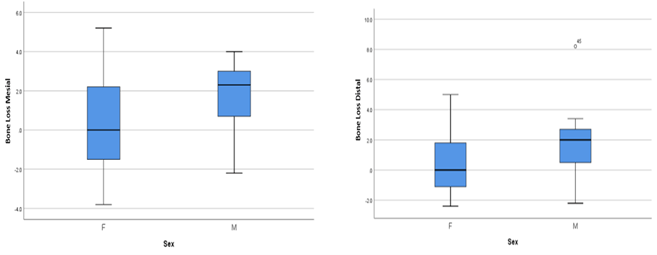
Figure 1: Millimeters of mesial and distal bone loss in implants between Male and Females.
Table 4: Descriptive statistics for continuous correlates and bone loss.
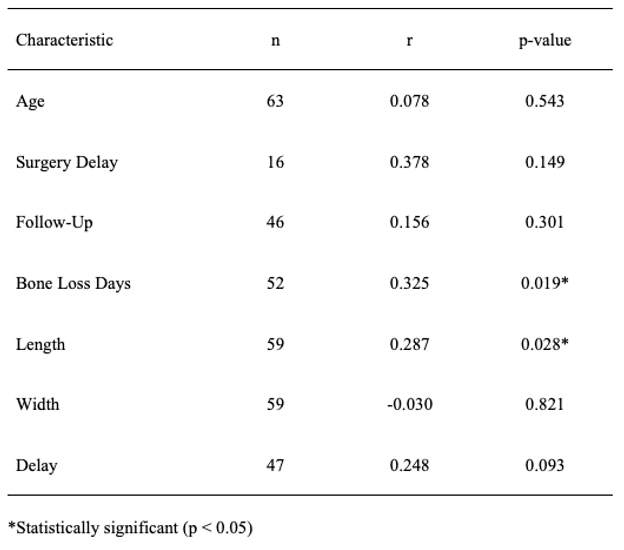
None of the continuous correlates were significantly associated with mesial bone loss (Table 5). However, bone loss by days from placement almost reached statistical significance (r = 0.264, p = 0.058). Bone loss by days from placement and length of the implant were significantly associated with distal bone loss (Table 6, Figure 3). Mesial bone loss and distal bone loss were significantly correlated with each other (r = 0.677, p < 0.001), and there was no significant difference between mesial and distal bone loss (mean difference ± SD, 0.04 ± 1.71, p = 0.843) (Figure 2). Bone loss days and length of the implant were significantly associated with average bone loss (Table 7).
Table 5: Pearson correlations between continuous characteristics and mesial bone loss.
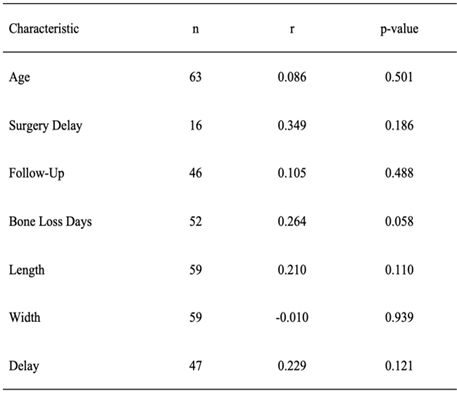
Table 6: Pearson correlations between continuous characteristics and distal bone loss.
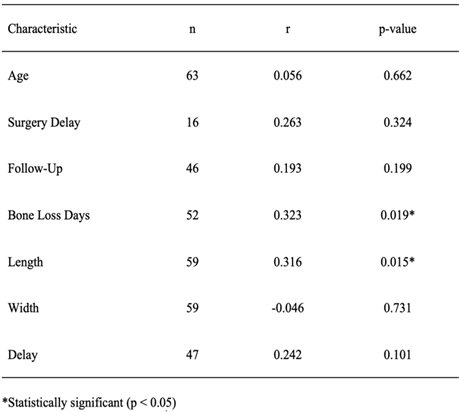
Table 7: Pearson correlations between continuous characteristics and average bone loss.
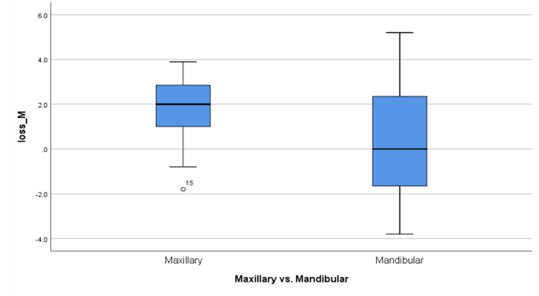
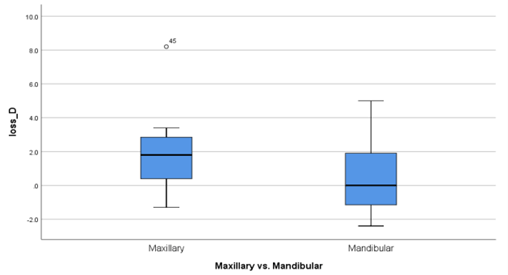
Bone loss differed significantly between males and females, with males showing significantly greater mesial (Table 1), distal (Table 2), and average bone loss (Table 3). With regard to social history, the one-way ANOVA indicated a significant difference among the groups in terms of mesial bone loss (p = 0.028; see Table 1), and the Tukey-Kramer procedure indicated that those patients with hypertension had significantly more bone loss on average than did those who were HIV positive (p = 0.026) [7]. No other significant pairwise differences were found. There was no significant difference among the social history groups with regard to distal bone loss (p = 0.195; see Table 2). The one-way ANOVA did not indicate a significant difference among the groups in terms of average bone loss (p = 0.053; see Table 3); however, the Tukey-Kramer procedure indicated that those patients with hypertension had significantly more average bone loss than did those who were HIV positive (p = 0.037). No other significant pairwise differences were found. Significantly more bone loss was found in maxillary implants than in mandibular. This was true for mesial (p = 0.013, Table 1), distal (p = 0.012, Table 2), and average bone loss (p = 0.006, Table 3). There was no significant difference in mesial, distal, or average bone loss between anterior and posterior implants (Tables 1, 2 & 3; Figures 2 & 3 respectively).
Figure 2: Millimeters of mesial bone loss in implants in the maxilla vs. the mandible.
Figure 3: Millimeters of distal bone loss in implants in the maxilla vs. the mandible.
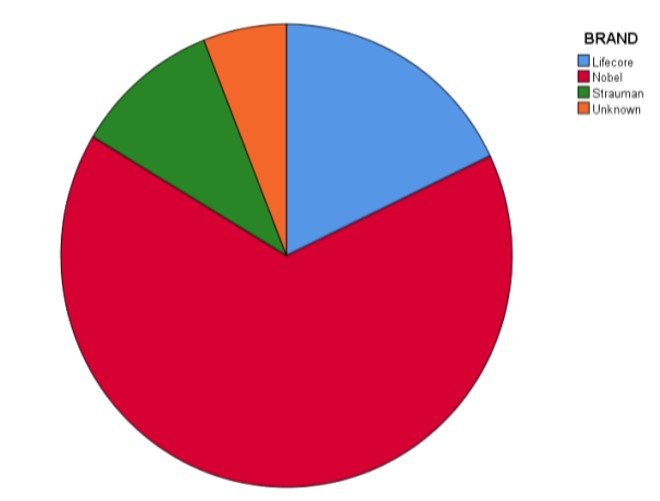
Over half of the implants were manufactured by Nobel (40/59, 68%) (Figure 4). The one-way ANOVA comparing the brands of implants in terms of mesial bone loss was not statistically significant (p = 0.057; see Table 1); however, the Tukey-Kramer method indicated that Nobel implants were associated with significantly more mesial bone loss than Strauman implants (p = 0.049). The one-way ANOVA comparing the brands in terms of distal bone loss was significant (p = 0.021; see Table 2), and the Tukey-Kramer method indicated that Lifecore implants were associated with significantly more distal bone loss than Strauman implants (p = 0.016). The comparison of Nobel implants with Strauman almost reached statistical significance (p = 0.063). The one-way ANOVA comparing the brands in terms of average bone loss was significant (p = 0.022; see Table 3), and the Tukey-Kramer method indicated that Strauman implants were associated with significantly less average bone loss than both Lifecore implants (p = 0.023) and Nobel implants (p = 0.031).
Figure 4: Demonstration of the ration of implant brand used in this study to the failures of the total group.
Eleven patients out of the 63 (17%) had at least one mechanical complication. The different types of mechanical complications did not differ significantly in terms of mean mesial bone loss (p = 0.292; see Table 1). However, those patients who had at least one mechanical complication had significantly more mesial bone loss than those who had none (Table 1, p = 0.036). There was a significant difference among the types of mechanical complications in terms of distal bone loss (p = 0.002; see Table 2), and the Tukey-Kramer method indicated that those patients with an explant had significantly less distal bone loss than those who had a thread exposure (p = 0.001) or a mechanical complication classified as Other (p = 0.007). In addition, those patients with a thread exposure had more distal bone loss, on average, than did those patients with a sinus perforation (p = 0.046). However, those patients who had at least one mechanical complication did not have significantly different distal bone loss than those who had none (Table 2, p = 0.904). The different types of mechanical complications did not differ significantly in terms of mean average bone loss (p = 0.190, see Table 3), and those patients who had at least one mechanical complication did not have significantly different average bone loss than those who had none (Table 3, p = 0.206).
Eighteen patients out of the 63 (29%) had at least one secondary procedure performed [8]. The different types of secondary procedures did not differ significantly in terms of mean mesial bone loss (p = 0.547; see Table 1). However, those patients who had at least one secondary procedure performed had significantly higher mesial bone loss than those who had none (Table 1, p = 0.002). There was a significant difference among the types of secondary procedures in terms of distal bone loss (p = 0.003; see Table 2). The Tukey-Kramer procedure indicated that those patients who underwent any secondary procedure involving collatape had significantly less distal bone loss than those who had any procedure involving FDBA (p = 0.033), any procedure involving dilators (p = 0.032), or any procedure with alveoloplasty (p = 0.003). In addition, the comparison of those patients who underwent any procedure with alveoloplasty with those procedures classified as Other almost reached statistical significance (p = 0.066). However, those patients who had at least one secondary procedure performed did not differ from those who had none in terms of distal bone loss (Table 2, p = 0.108). Average bone loss differed significantly among the different types of secondary procedures (Table 3, p = 0.027). The Tukey-Kramer procedure indicated that those patients who underwent any secondary procedure involving alveoloplasty had significantly more average bone loss than those who had any procedure involving collatape (p = 0.020). In addition, the comparison of those patients who underwent any procedure with alveoloplasty with those procedures classified as Other almost reached statistical significance (p = 0.065). Those patients who had at least one secondary procedure performed had significantly higher average bone loss than those who had none (Table 3, p = 0.007).
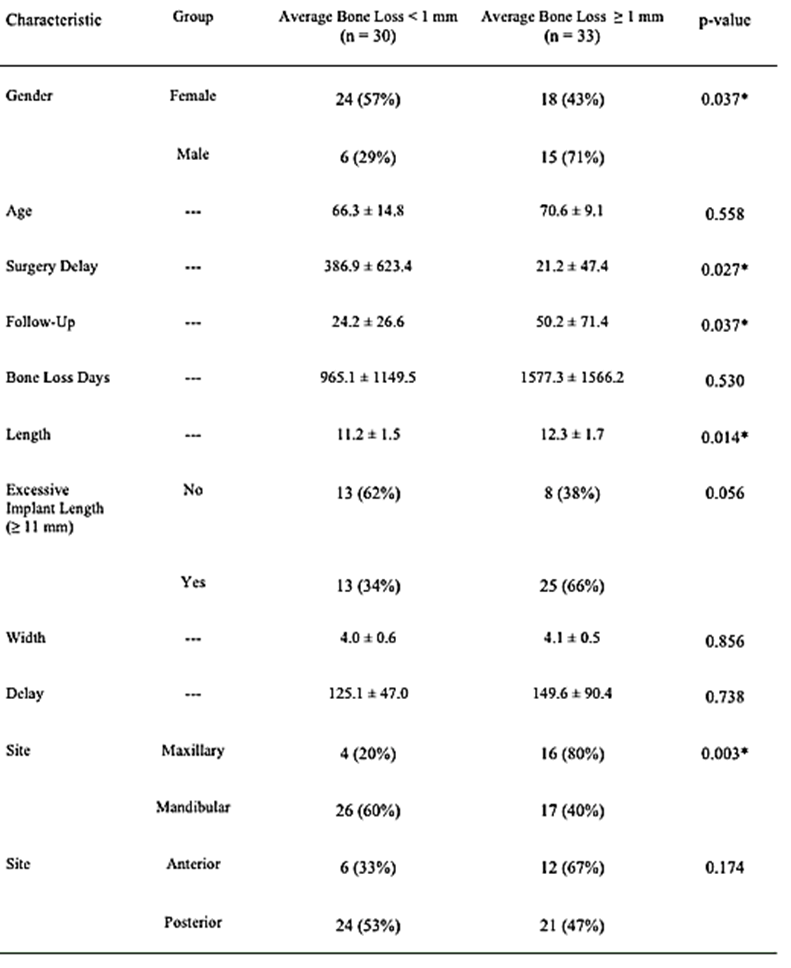
In our final analysis, we dichotomized average bone loss in order to classify each implant as “failed” (ABL ≥ 1 mm) or “successful” (ABL < 1 mm). Over half (33/63, 52%) of the implants were classified as failed using this criterion. We examined associations of each of the characteristics mentioned above with this outcome and the results are summarized in (Table 8). Gender was significantly associated with “failure” (p = 0.037), with a higher percentage of implants failing in males (71%) than in females (43%). There was a significantly shorter surgery delay (p = 0.027) and significantly longer follow-up time (p = 0.037) in the failed implants. The failed implants also were longer, on average, than those that were successful (p = 0.014). There was a significantly higher percentage of failed implants in the maxillary region (80%) than in the mandibular region (40%), p = 0.003. There were significantly fewer failures among Strauman implants than either Lifecore or Nobel (p = 0.039). Statistical significance was almost achieved when comparing failed and successful implants with regard to excessive implant length (p = 0.056), social history (p = 0.084), and those who had at least one secondary procedure performed (p = 0.056). None of the other characteristics were statistically significant when comparing failed vs. successful implants.
Table 8:Group comparisons for failed vs. successful implant (average bone loss ≥ 1 mm vs. average bone loss < 1 mm).
Discussion
This study was designed to determine the contributing factors and causes of crestal bone loss in dental implants and to evaluate the factors which cause the greatest impact on implant cervical bone health. We hypothesized that there was no difference in implant success based on location, brand, or length of the implant. Several areas of interest appeared when looking at sex predilection, comorbidities, and adjunct procedures. Bone loss differed significantly between males and females, with males showing a significantly greater mesial and average bone loss. Related to medical history, those patients with hypertension had significantly more bone loss on average. Lastly, patients who had at least one secondary procedure performed had significantly higher bone loss than those who had none.
We found that significantly more bone loss was found in maxillary implants than in mandibular. This result correlates well with Goiato et al. findings showing 97.6% survival in type I mandibular bone, and 88.8% survival in maxillary type IV bone. Alsheri also associated the poor quality/density of specific areas of bone to be associated with the overloading of an implant. This crestal bone loss, which we found as a result of secondary procedures, might cause one to alter clinical techniques to limit the number of additional procedures done at the time of implant placement. The findings of lower numbers of Strauman failures perhaps correlated to the findings of Niu et al. showing mechanical roughened crestal portions, micro threading, played a role in decreasing marginal bone loss.
The weaknesses of this study were the single location of data collection, the multitude of providers who placed the implants, and the incomplete data on follow-up and restoration timing. With a multicentered study, we could possibly eliminate institutional nuances learned or passed down that ignore newer data and techniques. Having several different levels of training, specialty and guidance, all affect the techniques, experience, and management of complications. If a study were to be designed between multiple practitioners of the same specialty with equal experience, it would allow for a more standardized procedure. When evaluating the implants and their timing for follow-up and restoration, it is important to understand patient motivation and pressures often influence ability to proceed. Standardized follow-up times and required intervals from placement to restoration would possibly allow more consistent results.
Conclusion
This study began with intentions of answering our null hypothesis but inspired more questions to be asked with a broader purpose of directing further research and questions relating to improving our process of implant placement, stability, and overall success. One feature which created interest was the relationship between implant length and bone loss. At this time, the effect size will be determined to evaluate a possible relationship between preparation time and crestal bone destruction. One other potential direction is to develop a measure of total implant bone loss to represent implant success or failure more accurately. Once these two evaluation directions are explored, we will re-analyse our data and continue to improve our clinical methods.
Article Info
Article Type
Review ArticlePublication history
Received: Fri 21, Jan 2022Accepted: Tue 08, Feb 2022
Published: Sat 05, Mar 2022
Copyright
© 2023 Alexander Faigen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2022.01.02
Author Info
Alexander Faigen J James M Stevens S Looney A Jenzer T Johnson
Corresponding Author
Alexander FaigenPGY-2 Resident, Department of Oral & Maxillofacial Surgery, Augusta University, Augusta, Georgia, USA
Figures & Tables
Table 1: Group comparisons for mesial bone loss.
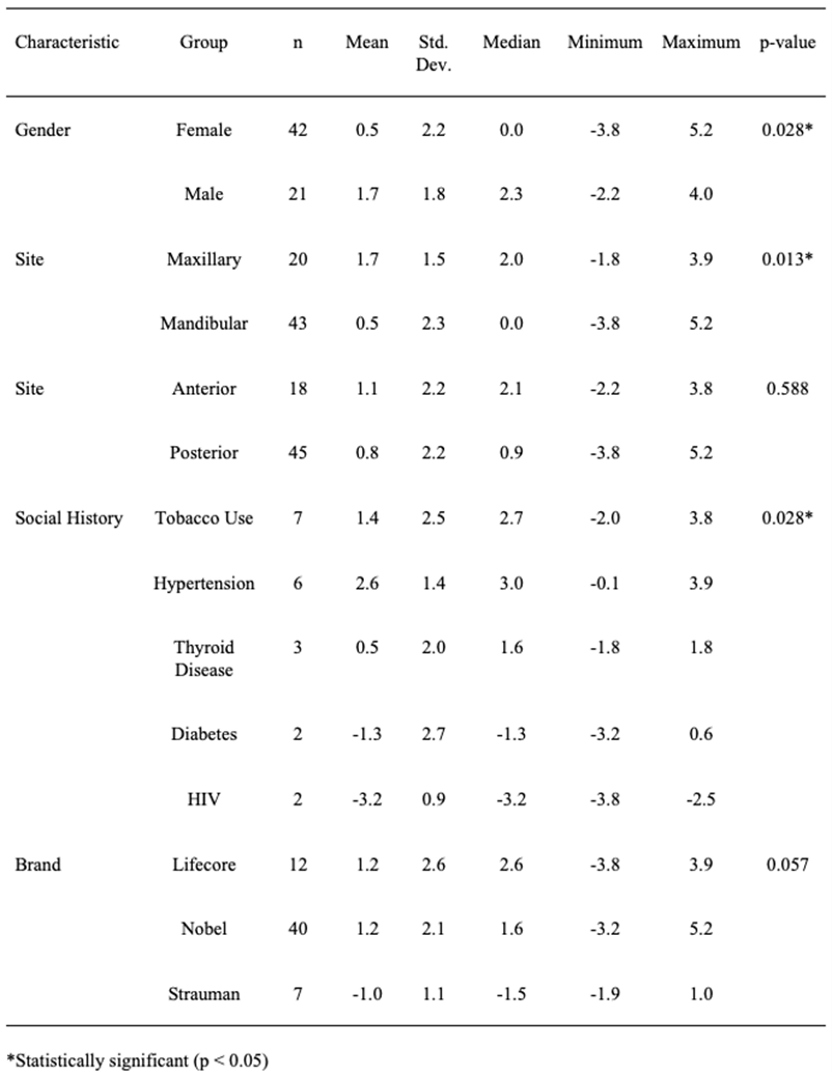
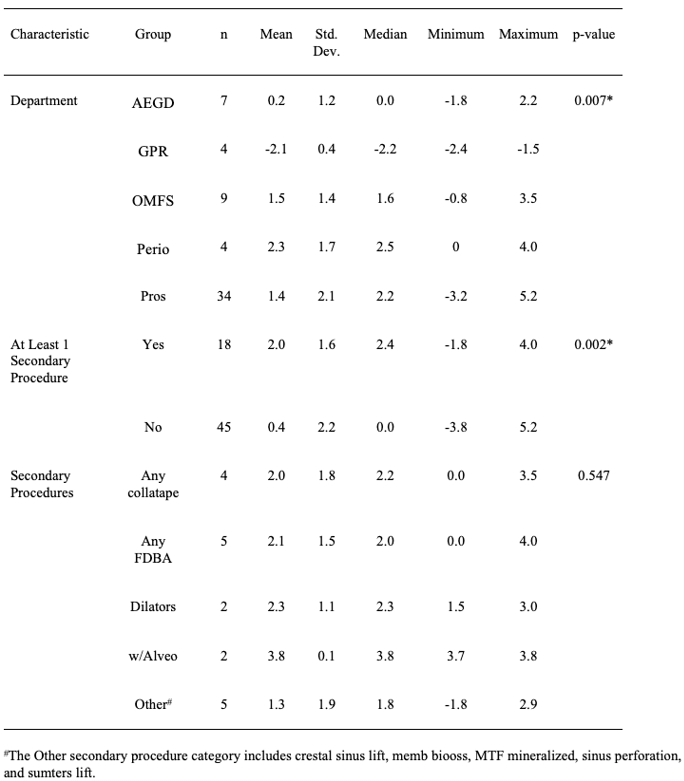
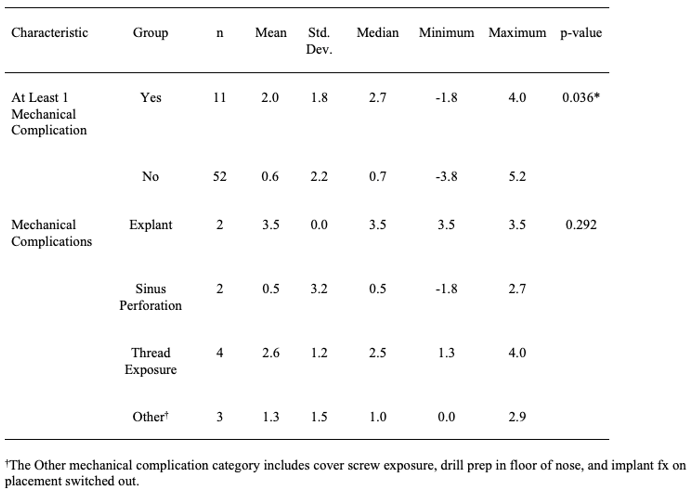
Table 2: Group comparisons for distal bone loss.
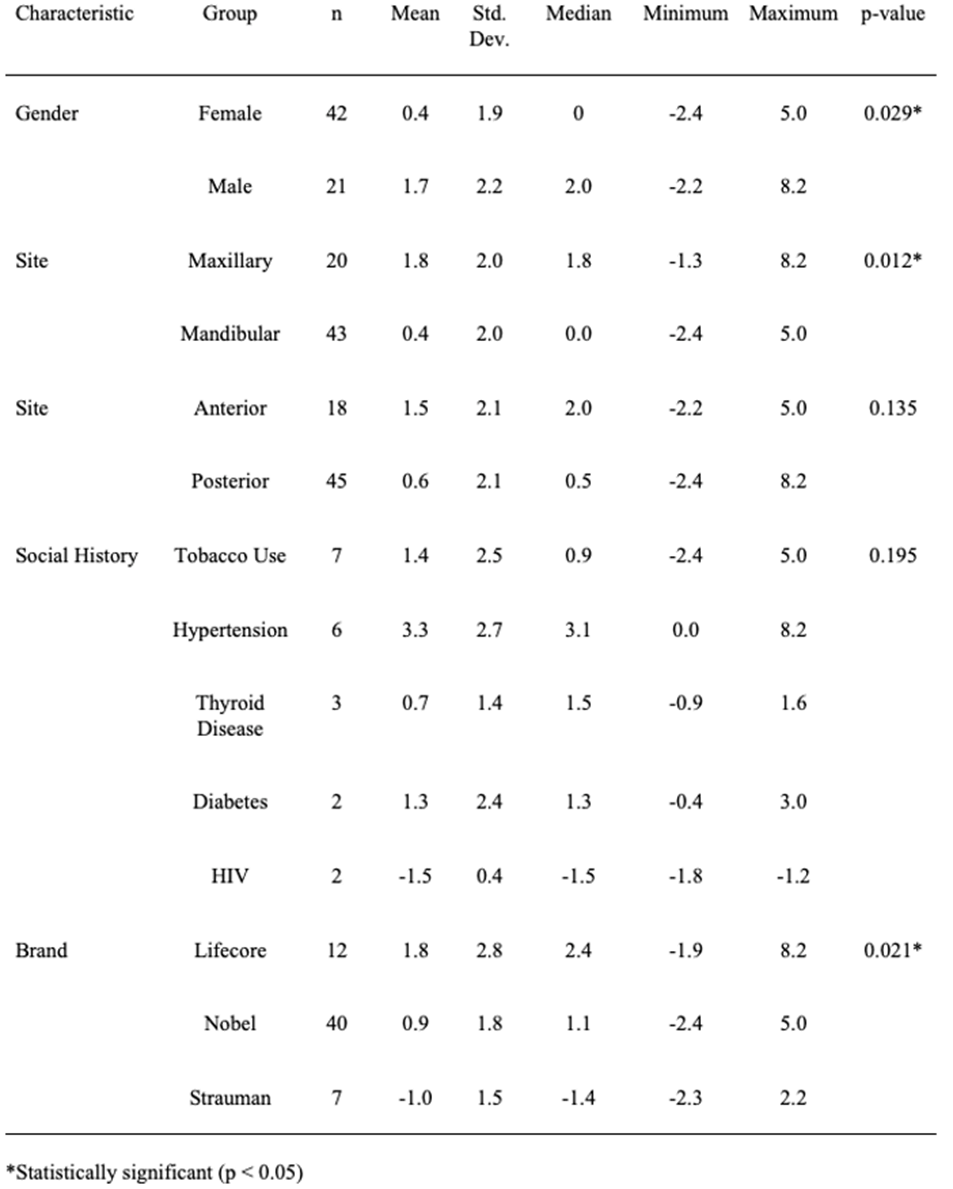
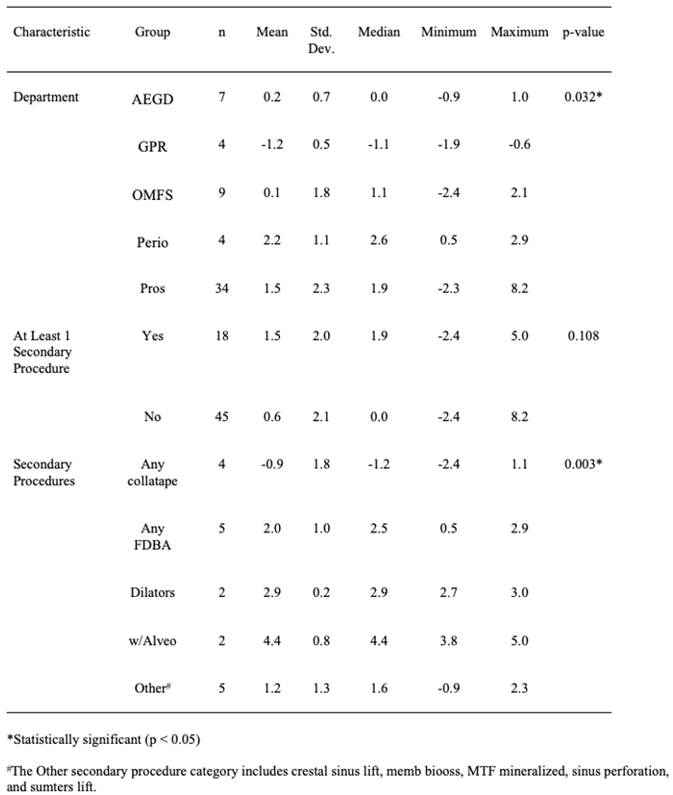
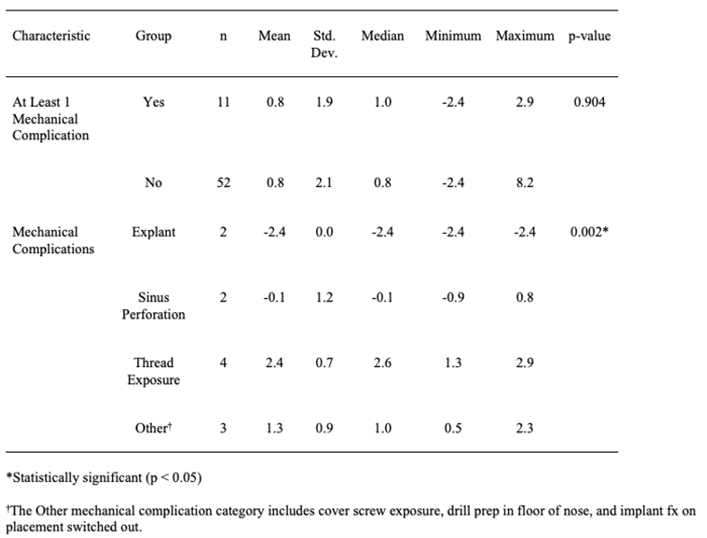
Table 3: Group comparisons for average bone loss.
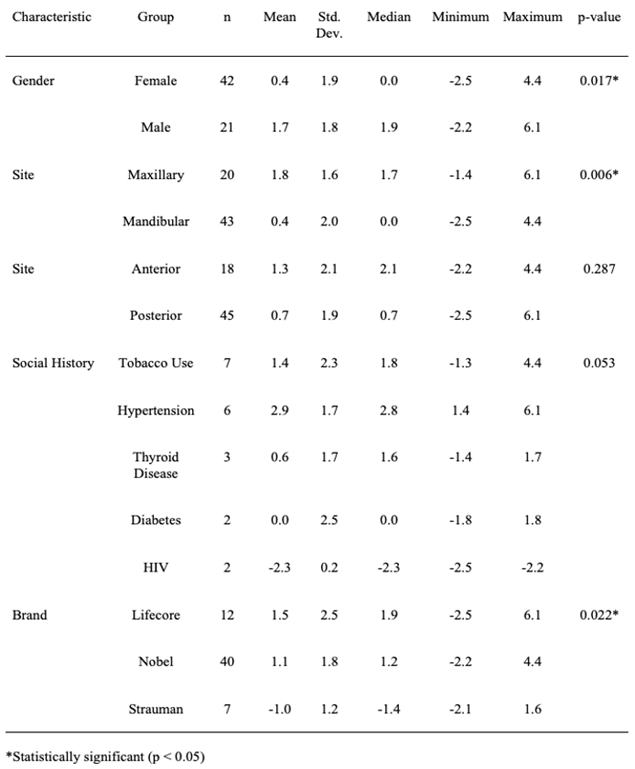
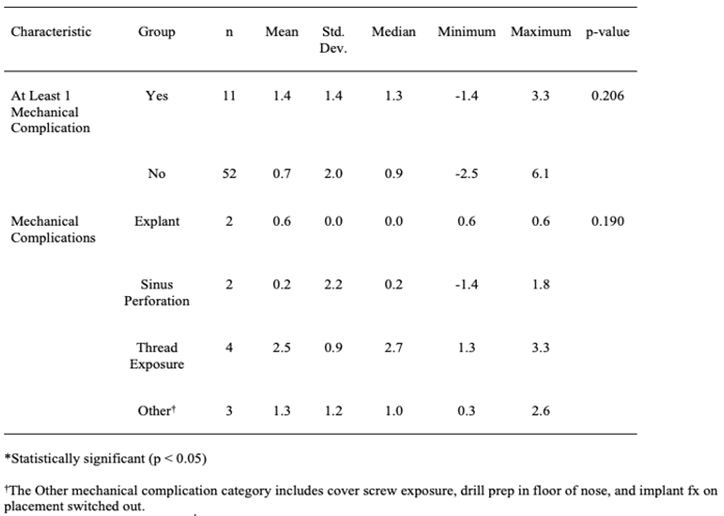
Table 4: Descriptive statistics for continuous correlates and bone loss.
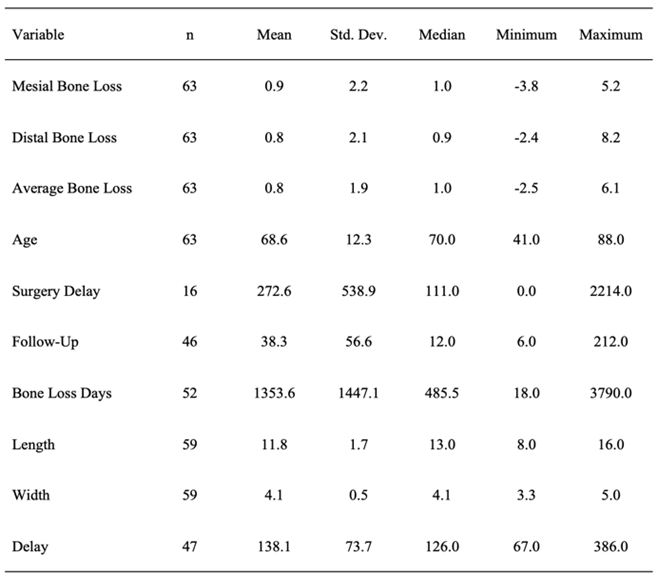
Table 5: Pearson correlations between continuous characteristics and mesial bone loss.
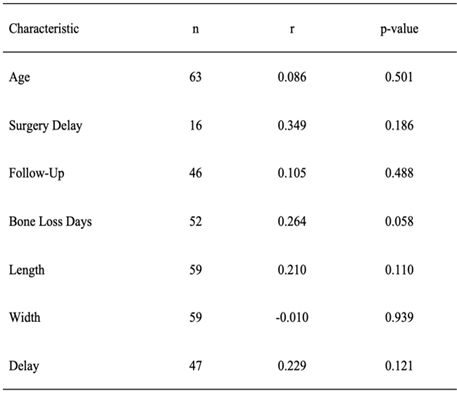
Table 6: Pearson correlations between continuous characteristics and distal bone loss.
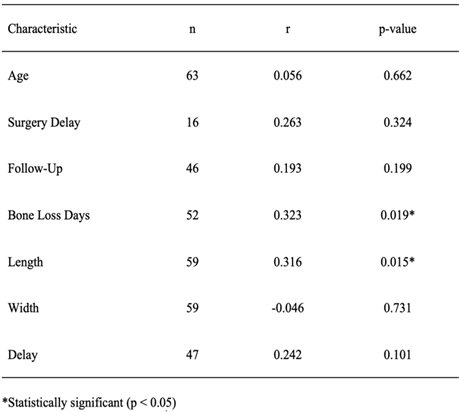
Table 7: Pearson correlations between continuous characteristics and average bone loss.
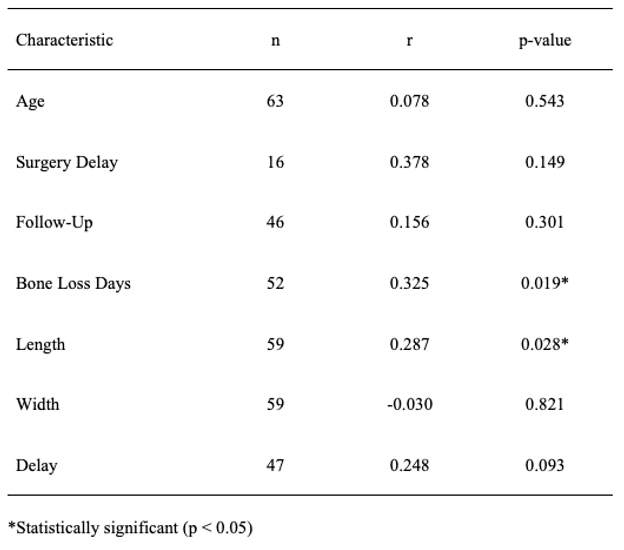
Table 8:Group comparisons for failed vs. successful implant (average bone loss ≥ 1 mm vs. average bone loss < 1 mm).
References
1. Goiato MC, dos
Santos DM, Jr Santiago JF, Moreno A, Pellizzer EP (2014) Longevity of dental
implants in type IV bone: a systematic review. Int J Oral Maxillofac Surg
43: 1108-1116. [Crossref]
2. Puisys A, Auzbikaviciute V, Minkauskaite A, Simkunaite Rizgeliene R,
Razukevicius D et al. (2019)
Early Crestal Bone Loss: Is it really loss? Clin Case Rep 7: 1913-1915. [Crossref]
3. Anupama Pujar K,
Ashok AC, Rudresh HK, Srikantaiah HC, Girish KS et al. (2013) Mortality in
typhoid intestinal perforation-a declining trend. J Clin Diagn Res 7:
1946-1948. [Crossref]
4. Nagarajan B, Murthy
V, Livingstone D, Surendra MP, Jayaraman S (2015) Evaluation of Crestal Bone
Loss Around Implants Placed at Equicrestal and Subcrestal Levels Before
Loading: A Prospective Clinical Study. J Clin Diagn Res 9: ZC47-ZC50. [Crossref]
5. Alsheri
M (2011) The maintenance of crestal bone around dental implants. Implants
Clin Technique 2: 20-24.
6. Niu W, Wang P, Zhu
S, Liu Z, Ji P (2017) Marginal bone loss around dental implants with and
without microthreads in the neck: A systematic review and meta-analysis. J
Prosthet Dent 117: 34-40. [Crossref]
7. Klimecs V, Grishulonoks A, Salma I, Neimane L, Locs J et al. (2018) Bone Loss around Dental Implants 5 Years after Implantation of Biphasic Calcium Phosphate (HAp/ β TCP) Granules. J Healthc Eng 2018: 4804902. [Crossref]
8. Schwartz Arad D, Yaniv Y, Levin L, Kaffe I (2004) A radiographic evaluation of cervical bone loss associated with immediate and delayed implants placed for fixed restorations in Edentulous jaws. J Periodontol 75: 652-657. [Crossref]
