Extensive Heterotopic Ossification of Bilateral Hip and Knee Joints in a Patient with Recurrent Traumatic Injuries
A B S T R A C T
Background: Heterotopic ossification (HO) refers to the growth of lamellar bone in soft tissues. Extensive heterotopic ossification is rarely seen. In this case, we illustrate a 35-year-old civilian patient with extensive HO due to recurrent traumatic injuries with no neurological deficit.
Case Presentation: A 35-year-old man, with a history of recurrent trauma episodes in the past year, presented with pain and swellings in bilateral lower limbs. Physical examination showed stiffness and deformities of bilateral hip and knee joints. Plain x-ray showed patchy ossification extending from hip joints to knee joints bilaterally. 3-dimensional Computer Tomography (3D-CT) showed extensive heterotopic ossifications along gluteal muscles, quadratus muscles and the deep fascia beneath, confirming the diagnosis of extensive heterotopic ossifications of bilateral hip and knee joints. Excision of ossified tissues and re-mobilization of iliotibial bands were performed. Early recovery after surgery (ERAS) strategy was used to speed up recovery.
Conclusion: i) Extensive heterotopic ossification in civilian patients is possible. Clinical history should be reviewed to rule out recurrent traumatic injury. Surgery should be considered. ii) Three-dimensional Computer Tomography (3D-CT) is a viable tool for surgical planning to show the extent, site, and anatomical relationship with adjacent tissues. iii) Post-op early recovery after surgery (ERAS) should be considered for better clinical outcomes.
Keywords
Bilateral heterotopic ossification, case report, lamellar bone formation
Introduction
Heterotopic ossification (HO) refers to the growth of lamellar bone in soft tissues. Epidemiologically, it can be divided into 2 broad categories: civilian patients and combat casualties [1]. For civilians, it has been reported in patients with spinal cord injury, spinal cord tumors, and post total hip/joint arthroplasty. We present the diagnosis and management of a civilian patient with extensive HO due to recurrent traumatic injuries with no neurological deficit. Because of the extensive lesions, especially the ossification which was unusual, large incisions were made bilaterally and rehabilitation with early recovery after surgery (ERAS) strategy was adopted for a better clinical outcome.
Case Report
A 35-year-old gentleman presented to the department of orthopaedics and trauma with a history of more than 30 fights with debtors between July 2018 and July 2019. He was hit with bamboo sticks on lower limbs, predominantly pelvis hips and femur. Previous history revealed recurrent soft tissue injuries without major fractures. He did not receive any formal treatment until August 2019, when he was admitted for lower limb deformities and significant movement limitations. The patient complained of pain and swelling on both thigh regions. Past medical history was insignificant.
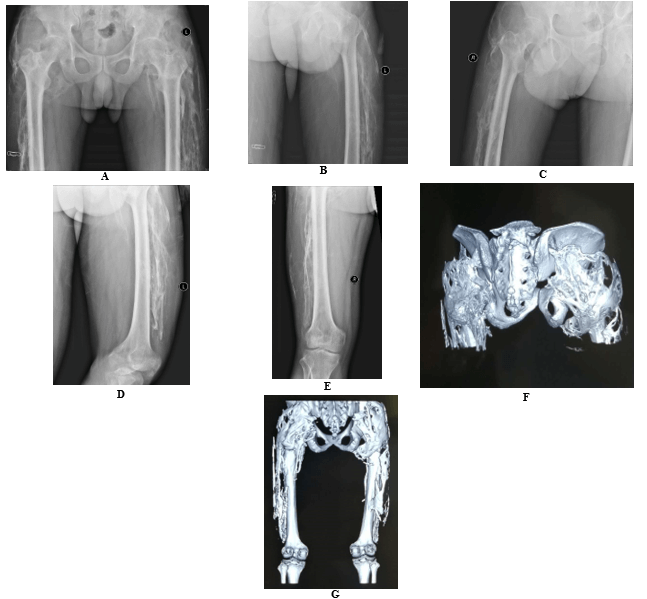
The patient could only walk with walking aids. Physical examination showed stiffness and deformities of bilateral hip and knee joints. There were no hip joint movements on both sides, including flexion, extension, adduction, and abduction. Bilateral knee flexions were 20°, but the knees could not be extended. The lower limbs were of the same length. The sensations were intact. Lower limb pulses were unremarkable. Radiological examination showed extensive ossifications at hip joints and knee joints on both sides (Figure 1). Pre-op 3D-CT reconstruction (Figure 2) further characterizes the extent of ossifications for surgical planning. Table 1 shows the summary of the findings of the patient.
Figure 1: Pre-op radiological findings. A) X-ray AP view of bilateral hip joint. B) X-ray AP view of left hip. C) X-ray AP view of right hip. D) X-ray AP view hip to knee region (left). E) X-ray AP view hip to knee region (right). F) 3D-CT of bilateral hip joints. G) 3D-CT of bilateral hip to knee region.
Table 1: Summary of findings of the patient.
|
A: Clinical and radiological findings of the patient |
||
|
|
Pre-op |
Post-op |
|
a. Clinical finding |
|
|
|
1) Hip joint movement (Active) |
|
|
|
Flexion |
Left: 0° Right: 0° |
Left: 100° Right: 100° |
|
Extension |
Left: 0° Right: 0° |
Left: 15° Right: 20° |
|
Adduction |
Left: 0° Right: 0° |
Left: 20° Right: 20° |
|
Abduction |
Left: 0° Right: 0° |
Left: 30° Right: 30° |
|
2) Knee joint movement (Active) |
|
|
|
Flexion |
Left: 20° Right: 20° |
Left: 90° Right: 130° |
|
Extension |
Left: 0° Right: 0° |
Left: 0° Right: 0° |
|
b. Radiological finding |
|
|
|
1) Right lower limb |
Extra-skeletal ossifications extending from hip region to the knee region. |
- |
|
2) Left lower limb |
Extra-skeletal ossifications extending from hip region to the knee region. |
- |
|
B: Surgical findings of the patient |
||
|
|
Left lower limb |
Right lower limb |
|
Hip region |
Extensive ossification around sciatic nerve, gluteus maximus, gluteus medius and greater trochanter. |
Ossifications around vastus medialis, vastus lateralis, vastus intermedius and rectus femoris extending from the hip joint to the knee joint. |
|
Knee region |
Remarkable ossification was found along iliotibial band, vastus lateralis, vastus medialis, rectus femoris, deep fascia in between quadratus femoris and pre-patellar bursa. |
Ossifications around vastus medialis, vastus lateralis, vastus intermedius and rectus femoris. Deep fascia ossification and stiffness was observed in between the above-mentioned quadriceps. |
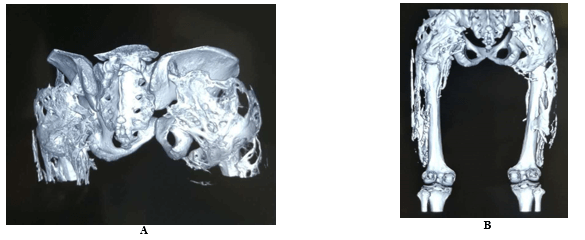
Figure 2: Pre-op 3D CT of A) bilateral hip joints, B) bilateral hip to knee region.
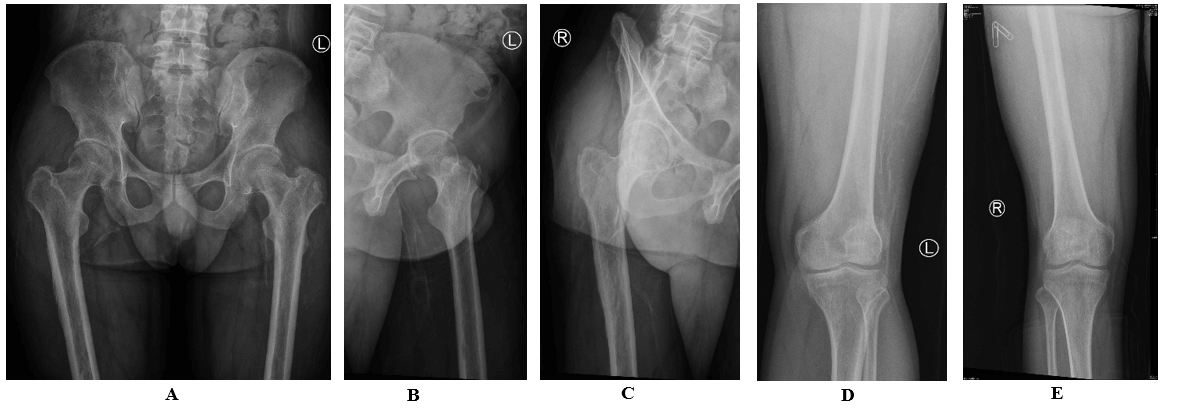
Figure 3: Post-op plain x-ray. A) Post-op bilateral hip. B) AP view of left hip. C) AP view of right hip. D) AP view hip to knee region (left). E) AP view hip to knee region (right).
Surgery was performed with corrective operation of the right lower limb in August 2019, followed by the left lower limb in January 2020. Posterior approach of the hip was adopted as the modality of surgery. A 35cm longitudinal incision was made on the right hip. Surgical exploration of the right lower limb showed remarkable ossifications around vastus medialis, vastus lateralis, vastus intermedius and rectus femoris muscles. Deep fascia ossification and stiffness were observed in the quadricep muscles. All the ossified tissues were excised, and the iliotibial band was remobilized (Figure 3). Post-op hip and knee joint movements subsequently improved, with range of motion of hip flexion 100°, hip extension 20°, and knee flexion 130°.
On the left, a longitudinal left hip incision of 35cm was made similarly as the right hip. Surgical exploration of the left lower limb showed extensive ossification around the sciatic nerve, gluteus maximus, gluteus medius and greater trochanter in the hip region. In the knee region, remarkable ossification was found along iliotibial band, vastus lateralis, vastus medialis, rectus femoris, and the deep fascia between the quadratus femoris and the pre-patellar bursa. The ossified tissues were excised, and the iliotibial band was mobilized. Post-op hip and knee joint movements improved, with range of motion of hip flexion 100°, extension 15°, and knee flexion 90°.
The patient was put on glucosamine indomethacin 50mg twice daily for 6 weeks and drainage tube was removed 2 days after surgery. Early recovery after surgery (ERAS) was incorporated in the post-operation recovery for early mobilization of the joints. He was able to walk without walking aids 9 months after the first surgery.
Discussion
Unlike previous reports of heterotopic ossifications in the literature, this patient with extensive heterotopic ossifications neither have neurological deficits, prolonged immobilization, fibrodysplasia ossificans progressiva nor burns [2-8]. This patient had multiple episodes of traumatic injury due to fights. There were also delays in getting proper treatment. However, the patient refused to disclose the details of fights until x-ray findings aroused suspicion of trauma. We advise surgeons to pay extra attention to take thorough clinical history to rule out recurrent trauma in case of extensive heterotopic ossifications. Stage-by-stage surgery can be suggested since positive clinical outcomes has been illustrated from this case.
The involved areas of ossification were very extensive, including quadriceps muscles, gluteal muscles and the deep fascia of both lower limbs. This led to the ‘frozen’ phenomenon of the hip and knee joints because the ossified muscle fibers and deep fascia failed to provide mechanical movements. Both the active and passive ranges of motion of hip joints and knee joints were significantly reduced. The management strategy was excision of the ossified tissues and re-mobilization of the iliotibial band to allow movements. The use of indomethacin for prophylaxis of novel heterotopic ossification was recommended to patients since studies have shown that the use of NSAIDs peri-operatively could significantly reduce the future risk of heterotopic ossifications [9, 10].
Choice of imaging should be based on clinical condition, availability of resources, and communications between surgeons and patients. Magnetic resonance imaging has been recommended for diagnosing early heterotopic ossification of knee joint in intensive care units [11]. However, 3-Dimensional Computer Tomography (3D-CT) was used for the pre-operational assessment of extensive heterotopic ossifications in this patient due to cost consideration by the patient. Plain x-ray showed patchy bilateral ossification in hip and knee regions which was sufficient to diagnose heterotopic ossifications. 3D-CT further showed the fine details of the heterotopic ossifications on soft tissues, including their sites, extent of involvement, functional and anatomical relationships with surrounding tissues. This was vital in formulating surgical plans because it provided important information on the extent of excision of the involved tissues, and the degree of mobilization of iliotibial band for reconstruction surgery.
Conclusion
This case illustrates that unusual extensive HO is possible in recurrent traumatic injures with delayed treatment, requiring large incisions. 3D-CT reconstruction imaging is essential for surgical planning. Post-op ERAS should be considered for a better clinical outcome.
Author Contributions
Figures, data collection, data analysis, data interpretation and manuscript writing were done by Zhipeng Yan, Kai-Wen Wang, Janice Wing-Tung Kwong, Professor Ching-Lung Lai, and Xin-Bao Wu.
Acknowledgment
None.
Ethical Approval and Consent to Participate
Not applicable.
Consent for Publication
Consent was obtained.
Availability of Data and Material
All data generated or analysed during this study are included in this published article.
Competing Interests
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Sat 11, Jul 2020Accepted: Mon 15, Mar 2021
Published: Tue 30, Mar 2021
Copyright
© 2023 Qi-Yong Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.03.19
Author Info
Zhipeng Yan Kai-Wen Wang Janice Wing-Tung Kwong Ching-Lung Lai Qi-Yong Cao
Corresponding Author
Qi-Yong CaoDepartment of Trauma and Orthopaedics Surgery, Beijing Jishuitan Hospital, Beijing, China
Figures & Tables
Table 1: Summary of findings of the patient.
|
A: Clinical and radiological findings of the patient |
||
|
|
Pre-op |
Post-op |
|
a. Clinical finding |
|
|
|
1) Hip joint movement (Active) |
|
|
|
Flexion |
Left: 0° Right: 0° |
Left: 100° Right: 100° |
|
Extension |
Left: 0° Right: 0° |
Left: 15° Right: 20° |
|
Adduction |
Left: 0° Right: 0° |
Left: 20° Right: 20° |
|
Abduction |
Left: 0° Right: 0° |
Left: 30° Right: 30° |
|
2) Knee joint movement (Active) |
|
|
|
Flexion |
Left: 20° Right: 20° |
Left: 90° Right: 130° |
|
Extension |
Left: 0° Right: 0° |
Left: 0° Right: 0° |
|
b. Radiological finding |
|
|
|
1) Right lower limb |
Extra-skeletal ossifications extending from hip region to the knee region. |
- |
|
2) Left lower limb |
Extra-skeletal ossifications extending from hip region to the knee region. |
- |
|
B: Surgical findings of the patient |
||
|
|
Left lower limb |
Right lower limb |
|
Hip region |
Extensive ossification around sciatic nerve, gluteus maximus, gluteus medius and greater trochanter. |
Ossifications around vastus medialis, vastus lateralis, vastus intermedius and rectus femoris extending from the hip joint to the knee joint. |
|
Knee region |
Remarkable ossification was found along iliotibial band, vastus lateralis, vastus medialis, rectus femoris, deep fascia in between quadratus femoris and pre-patellar bursa. |
Ossifications around vastus medialis, vastus lateralis, vastus intermedius and rectus femoris. Deep fascia ossification and stiffness was observed in between the above-mentioned quadriceps. |
References
1. Dey D, Wheatley BM, Cholok D, Agarwal S, Yu PB. (2017) The traumatic bone: trauma-induced heterotopic ossification. Transl Res 186: 95-111. [Crossref]
2. Kougias V, Hatziagorou E, Laliotis N, Kyrvasillis F, Georgopoulou V et al. (2019) Two cases of myositis ossificans in children, after prolonged immobilization. J Musculoskelet Neuronal Interact 19: 118-122. [Crossref]
3. Kartal Kaess M, Shore EM, Xu M, Schwering L, Uhl M et al. (2010) Fibrodysplasia ossificans progressiva (FOP): watch the great toes! Eur J Pediatr 169: 1417-1421. [Crossref]
4. Zhang X, Jie S, Liu T, Zhang X (2014) Acquired heterotopic ossification in hips and knees following encephalitis: case report and literature review. BMC Surg 14: 74. [Crossref]
5. Sharma VP, Yadav G, Gupta AK, Kumar D (2014) Extensive heterotopic ossification in patient with tubercular meningitis. J Neurosci Rural Pract 5: S71-S74. [Crossref]
6. Espandar R, Haghpanah B (2010) Acceptable outcome following resection of bilateral large popliteal space heterotopic ossification masses in a spinal cord injured patient: a case report. J Orthop Surg Res 5: 39. [Crossref]
7. Yoon BH, Park IK, Sung YB (2018) Ankylosing Neurogenic Myositis Ossificans of the Hip: A Case Series and Review of Literature. Hip Pelvis 30: 86-91. [Crossref]
8. Kornhaber R, Foster N, Edgar D, Visentin D, Ofir E et al. (2017) The development and impact of heterotopic ossification in burns: a review of four decades of research. Scars Burn Heal 3: 2059513117695659. [Crossref]
9. Fransen M, Neal B (2004) Non-steroidal anti-inflammatory drugs for preventing heterotopic bone formation after hip arthroplasty. Cochrane Database Syst Rev 2004: CD001160. [Crossref]
10. Neal BC, Rodgers A, Clark T, Gray H, Reid IR et al. (2000) A systematic survey of 13 randomized trials of non-steroidal anti-inflammatory drugs for the prevention of heterotopic bone formation after major hip surgery. Acta Orthop Scand 71: 122-128. [Crossref]
11. Argyropoulou MI, Kostandi E, Kosta P, Zikou AK, Kastani D et al. (2006) Heterotopic ossification of the knee joint in intensive care unit patients: early diagnosis with magnetic resonance imaging. Crit Care 10: R152. [Crossref]
