Journals
Effects of a combined nutraceutical on glucose and lipid metabolism in women with post-menopausal incident metabolic syndrome: a double-blind, placebocontrolled, randomized clinical trial
A B S T R A C T
Background: Metabolic syndrome is characterized by the impairment of several metabolic and haemodynamic parameters. Several natural compounds have just demonstrated to improve glucose and lipid levels in humans.
Aim: To assess the short-term glucose and lipid-lowering effects of a combination of nutraceuticals based on Lagerstroemia speciosa, Berberis aristata, Curcuma longa, alpha-lipoic acid, chrome picolinate and folic acid in patients with post-menopausal incident metabolic syndrome.
Methods: We performed a double-blind, placebo-controlled, parallel-group, randomized clinical trial by enrolling 40 women in primary prevention of cardiovascular disease and affected by metabolic syndrome occurred in menopause. After 2-week run-in period of dietary standardization, enrolled patients were allocated to active treatment or placebo for 8 weeks. Data related to lipid pattern, insulin resistance, liver function and hsCRP were obtained at the beginning and at the end of the study.
Results: No patient experienced any subjective or laboratory adverse event. During the study, there were no significant changes in waist circumference, body mass index, blood pressure and low-density lipoprotein cholesterol in either treatment groups. Subjects randomized to nutraceutical treatment experienced a significant improvement in triglycerides (TG= -32.2%), high-density lipoprotein cholesterol (HDL-C= +5.7%), fasting plasma insulin (FPI= -14.1%), and in homeostasis model assessment of insulin resistance (HOMA-Index= -27.3%) versus the baseline values, as welle as compared to the placebo-treated group.
Conclusions: The tested nutraceutical compound showed to be effective in improving TG, HDL-C, FPI and HOMA-Index, with an optimal tolerability profile in patients with post-menopausal incident metabolic syndrome.
Keywords
Nutraceuticals, insulin-sensitivity, metabolic syndrome, impaired fasting glucose
Background
Menopause is associated with a functional decline in gonadal steroid hormones and in other steroid hormones -such as inhibins-, which corresponds to increased plasma levels of gonadotropins [1]. The decrease in estrogen levels that accompanies menopause causes an increased risk of cardiovascular disease. Typically, women are around 10 years older than men at first presentation of atherosclerotic coronary heart disease and this can be related to decline in ovarian hormone concentrations during the menopausal transition and beyond [2]. In fact, estrogens through their intracellular receptors regulate various aspects of glucose and lipid metabolism, that results in the phenotype of the metabolic syndrome [3]. In particular, a critical and protective role for skeletal muscle estrogen receptor α in the maintenance of metabolic homeostasis and insulin sensitivity has been clearly described [4]. The improvement of life style remains the milestone to prevent and (partially) revert metabolic changes associated to cardiovascular disease risk increase, such as impairment of plasma glucose and lipid values [5, 6].
On the other side, a relatively large number of nutraceutical substances have recently demonstrated to exert lipid-lowering activity, other than to improve glucose metabolism and inflammatory parameters in metabolic syndrome patients [7]. Berberis aristata (tree turmeric) is a shrub containing the quaternary ammonium salt berberine. Berberine has been demonstrated to improve glucose and lipid metabolism disorders, and to reduce atherogenesis and endothelial inflammation in diabetic patients, with clinical effects similar to those of metformin [8, 9]. Its effect on glucose metabolism, in fact, like metformin, does not depend on insulin concentration [10]. Lagerstroemia speciosa, also known as banaba, is a tropical plant found in the Southeast area of Asia. It has been shown to have, among others, hypoglycaemic and antihyperlipidemic effects, due to corosolic acid and ellagitannins, which are two of its main components [11]. The action mechanisms involved consist of enhanced cellular uptake of glucose, impaired hydrolysis of sucrose and starches, decreased gluconeogenesis and the regulation of lipid metabolism. A supplementation with banaba has proved to be safe and well tolerated in clinical trials [12]. In addition, its action on both glucose and lipid metabolism could be useful in the management of metabolic syndrome [13]. Curcuma longa (turmeric) has long been used in Oriental traditional medicine because of its anti-inflammatory properties. Its main component, curcumin, is responsible for anti-inflammatory, anti-neoplastic, antioxidant and antimicrobial effects, with direct therapeutic properties in diabetic subjects [14, 15]. Alpha lipoic acid has an antioxidant effect, with a proven anti-inflammatory and insulin like activity, suggesting a therapeutic role in the management of diabetic and pre diabetic subjects [16]. Chromium picolinate has also proved to be a hypoglycaemic and insulin-resistance reducing substance in patients with T2DM [17]. Folic acid, part of the group B vitamins, has an antioxidant activity. Its supplementation in T2DM patients, together with B12 vitamins, has a positive effect on insulin resistance, fasting plasma glucose level and homocysteinaemia, as well [18]. The association of several nutraceuticals, in particular in patients with two or more risk factors for cardiovascular diseases, has been proved to have a synergistic effect [19]. In particular, the combined effect of the above tested nutraceuticals has been already tested by our group in a pilot trial carried out on both men and women with impaired fasting glucose [20].
The aim of this trial is to test the metabolic effect of a combination of Lagerstroemia speciosa, Berberis aristata, Curcuma longa, alpha-lipoic acid, chrome picolinate and folic acid in patients with post-menopausal incident metabolic syndrome.
Materials & Methods
Study design
This double-blind, placebo-controlled, parallel-group, randomized clinical trial involved 40 women affected by post-menopausal incident metabolic syndrome and impaired fasting glucose in primary prevention for cardiovascular disease, consecutively enrolled in the outpatient service of cardiovascular disease prevention in the Medical and Surgical Sciences Department of the University of Bologna. The study consisted of a trial with a total duration of 10 weeks. During the first 2 weeks, patients received standard behavioural and qualitative (not quantitative) dietary suggestions to correct unhealthy habits. In particular, subjects were instructed to follow a general indication of a Mediterranean diet, avoiding excessive intake of dairy products and red meat derived products during the study, and maintaining overall constant dietary habits. Individuals were also generically encouraged to increase their physical activity by walking briskly for 20 to 30 minutes, 3 to 5 times per week, or by cyclinßg. After a period of 2 weeks of dietary habits correction only, patients continued the diet and began a period of 8 weeks of treatment with nutraceutical or placebo. Data related to lipid pattern, insulin resistance, liver function and hsCRP were obtained at the baseline and at the end of the study. The only inclusion criteria were the feature of the metabolic syndrome, appeared after the menopause [21].
Exclusion criteria were:
- Familial Hypercholesterolemia and/or Familial Hypertriglyceridemia and/or treatment with lipid-lowering drugs/nutraceuticalsß
- Type 2 diabetes or assumption of glucose lowering drugs/supplements
- Obesity (BMI>30 kg/m2)
- Secondary prevention for cardiovascular disease
- Endocrinological conditions in a failure state (e.g. hypothyroidism, Cushing Syndrome)
- Occasional, programmed or chronic assumption of corticosteroids
The study was fully conducted in accordance with the Declaration of Helsinki, its protocol was approved by the Ethical Committee of the University of Bologna, and informed consent was obtained from all patients before their inclusion in the study.
Treatments
After 2 weeks of diet and physical activity stabilization, patients were allocated to treatment with indistinguishable pills including either placebo or active product containing Lagerstroemia speciosa extract (1% corosolic acid) 250 mg, Berberis aristata extract (98% berberine) 155 mg, curcuma extract 125 mg, chromium picolinate 1.3 mg, folic acid 0.15 mg, solvent-free alpha lipoic acid 110 mg (kindly provided by Pegaso Srl, Arbizzano di Negrar, VR, Italy), at a dose of 2 pills per day. Clinical and laboratory data were obtained at the baseline and after the end of the treatment period. Randomization was done by assigning an alphabetical code to each batch code (corresponding to treatment or placebo) impressed on the pillbox. Codes were then kept in a sealed envelope, which was not opened until the end of the trial. Pillboxes were then mixed, and the investigators assigned a blinded pillbox to each enrolled patient. Throughout the study, we instructed patients to take the first dose on the day after they were given the study product. At the same time, all unused products were returned to the investigator.
Assessments
Personal data, cardiovascular disease history and pharmaceutical anamnesis of each patient were collected at the beginning of the trial. Anthropometrical parameters, such as body weight, waist circumference (WC) and Body Mass Index (BMI) were collected both at the beginning and during the trial, together with haemodynamic and biochemical parameters. BMI was calculated as weight in kilograms divided by the square of height in metres. Haemodynamic parameters were collected measuring orthostatic and clinostatic systolic and diastolic blood pressure (mean value of 3 interval measures). Also, orthostatic and clinostatic wrist blood pressure (mean value of 3 interval measures) and cardiac frequency were collected. All biochemical parameters were obtained after a 12-hour overnight fast and the following parameters were obtained or calculated through appropriate formulae: total cholesterol (TC), high-density lipoprotein-cholesterol (HDL-C), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), non-HDL cholesterol (non HDL-C), fasting plasma glucose (FPG), fasting plasma insulin (FPI), serum uric acid (SUA), and high-sensitivity C-reactive protein (hsCRP) [22]. All measurements were centrally performed in the laboratory of our department with standardized methods by trained biologists [23]. Homeostasis model assessment of insulin resistance (HOMA-IR) is the simplest and most commonly used method to estimate insulin resistance. It was calculated as the product of basal glucose (mmol/l) and fasting insulin (U/ml) divided by 22.5 [24]. Adherence to behavioural counselling and to treatment/placebo, tolerability, acceptability and compliance were also assessed.
Figure 1: CONSORT flow diagram.
Table 1: Pre- and post-treatment values.
|
Parameters |
Active treatment |
Placebo treatment |
||||||
|
Pre-treatment |
Post-treatment |
Pre-treatment |
Post-treatment |
|||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Waist circumference (cm) |
89.9 |
8.4 |
87.1 |
8.1 |
88.1 |
8.1 |
87.9 |
8.3 |
|
Body mass index (Kg/m2) |
26.9 |
1.4 |
26.8 |
1.2 |
26.8 |
1.3 |
26.8 |
1.3 |
|
Systolic blood pressure (mmHg) |
133.1 |
7.2 |
130.5 |
9.8 |
129.5 |
9.8 |
127.9 |
9.4 |
|
Diastolic blood pressure (mmHg) |
81.4 |
3.3 |
79.8 |
4.0 |
79.2 |
3.0 |
79.4 |
3.9 |
|
Total cholesterol (mg/dl) |
222.8 |
15.3 |
216.8* |
12.0 |
224.9 |
13.8 |
221.3 |
12.8 |
|
Triglycerides (mg/dl) |
206.9 |
25.3 |
141.1*° |
23.5 |
194.8 |
24.9 |
169.9* |
29.6 |
|
HDL-cholesterol (mg/dl) |
45.7 |
3.1 |
48.3*° |
3.4 |
44.1 |
3.5 |
45.6 |
3.3 |
|
LDL-cholesterol (mg/dl) |
137.8 |
12.3 |
141.3 |
12.1 |
142.3 |
10.1 |
142.6 |
13.5 |
|
Non-HDL-cholesterol (mg/dL) |
177.9 |
13.3 |
170.1* |
14.4 |
181.1 |
11.4 |
176.9 |
15.3 |
|
Fasting plasma glucose (mg/dl) |
114.6 |
4.6 |
98.3* |
3.8 |
115.1 |
3.9 |
108.9* |
4.1 |
|
Fasting plasma insulin (mcL/mL) |
19.9 |
3.1 |
17.1*° |
2.5 |
18.8 |
3.4 |
18.2 |
2.9 |
|
HOMA Index |
5.61 |
0.64 |
4.08*° |
0.73 |
5.44 |
0.63 |
5.23 |
0.87 |
|
High sensitivity C-reactive protein (mg/L) |
3.08 |
0.14 |
2.71* |
0.18 |
3.12 |
0.15 |
2.87 |
0.17 |
*P<0.05 vs baseline; °P<0.05 vs placebo
HDL= High-density lipoprotein; HOMA= Homeostasis model assessment of insulin resistance; LDL= Low-density lipoprotein; SD= Standard deviation.
Table 2: Row effect of the active treatment and of the placebo on glico-metabolic parameters.
|
Parameters |
Delta after treatment group |
Delta after placebo group |
||
|
Triglycerides (mg/dl) |
-66.6*° |
8.7 |
-25.3* |
4.8 |
|
HDL-cholesterol (mg/dl) |
+2.6*° |
0.8 |
+1.5 |
0.5 |
|
Non-HDL-cholesterol (mg/dL) |
-7.8* |
2.3 |
-4.1 |
1.4 |
|
Fasting plasma glucose (mg/dl) |
-16.2* |
3.9 |
-6.2* |
2.8 |
|
Fasting plasma insulin (mcL/mL) |
-2.8*° |
0.9 |
-0,6 |
0.4 |
|
HOMA Index |
-1.53*° |
0.25 |
-0.21 |
0.11 |
*P<0.05 vs baseline; °P<0.05 vs placebo
HDL= High-density lipoprotein ; HOMA= Homeostasis model assessment of insulin resistance.
Statistical Analyses
Data were analysed using intention to treat by means of the Statistical Package for Social Science (SPSS) 23.0, version for Windows. Normally distributed baseline characteristics of the population were compared using Student’s t test, non-normally distributed parameters using Mann-Whitney-U test for paired and unpaired samples. All data are expressed as means and standard deviation (SD). A p level less than 0.05 was set as statistically significant for all tests.
nutraceutical treated group (p<0.05) but did not significantly changed in comparison with placebo group (p>0.05). Serum TG levels were reduced in both groups (p<0.05), but more in the active treated one (p<0.05). On the other hand, HDL-C, FPI and HOMA-index improved only in the nutraceutical treated group (p<0.05), when compared both to baseline and the control group (Table 1, Table 2). At the end of the treatment, 8 (40%) subjects in the nutraceuticals treated group and 3 (15%) in the placebo treated one were no more classified as metabolic syndrome patients.
Results
Forty patients were consecutively enrolled and randomized to receive the active (n= 20; age= 55.6±3.3 years) or placebo (n= 20; age= 55.9±3.5 years) treatment. All participants completed the trial according to the study design and no patient experienced any subjective or laboratory adverse event (dropout rate= 0). The CONSORT flow diagram is shown in (Figure 1). The compliance to the treatment was near to 100% in both groups. Baseline clinical features and investigated laboratory parameters were similar between groups (Table 1). Compared to baseline values, no change was detected in either group as regards WC, BMI, systolic and diastolic blood pressure, and LDL-cholesterol (Table 1). However, both groups experienced a significant improvement in FPG (p<0.05). Serum concentrations of TC, Non-HDL-C and hsCRP improved only in the nutraceutical treated group (p<0.05) but did not significantly changed in comparison with placebo group (p>0.05). Serum TG levels were reduced in both groups (p<0.05), but more in the active treated one (p<0.05). On the other hand, HDL-C, FPI and HOMA-index improved only in the nutraceutical treated group (p<0.05), when compared both to baseline and the control group (Table 1, Table 2). At the end of the treatment, 8 (40%) subjects in the nutraceuticals treated group and 3 (15%) in the placebo treated one were no more classified as metabolic syndrome patients.
Discussion
In the present trial carried out on post-menopausal women with impaired fasting glucose, we observed that a nutraceutical compound was able to improve on the short-term the serum level of TG (-32.2%), HDL-C (+5.7%), FPI (-14.1%), and HOMA-Index (-27.3%) versus baseline. All these parameters are related to insulin-resistance and metabolic syndrome. Considering that metabolic syndrome is a highly prevalent and incident condition associated with an increased risk of developing type 2 diabetes and cardiovascular disease, the improvement of parameters related to the use of the tested product made it a possible interesting therapeutic tool, when associated with a balanced diet [25-27]. Moreover, the observed results were at least partly expected, because the components of the tested mixture have all been supported by an acceptable level of clinical evidence of efficacy [28]. In particular, chlorogenic acid, berberine, curcumin and chromium picolinate have clearly demonstrated that they exert an insulin-sensitizing effect in humans [29-32]. On the other hand, the lack of efficacy of the combined nutraceutical on the systemic inflammation evaluated by the measurement of the serum hsCRP is slightly in contrast with what was previously observed with berberine and curcumin this is probably related to the low doses used of the single nutraceutical components and to the short duration of the treatment [30, 31]. Blood pressure also did not improve beyond the observed improvement of insulin-resistance related parameter; however, this could be related to the short duration of the trial and the small improvement on HOMA-index observed. Then, the tested product was associated with a high tolerability profile that is important to guarantee long-term compliance of the treatment. Of course, our trial also has some important limitations. First of all, the sample size was relatively small, but sufficient to detect the mean FPG difference supposed for the sample size calculation. Then the study was short: its duration was adequate to test the short-term effect, but we are not able to infer our results on the middle-long term. Finally, we did not evaluate an eventual rebound effect on stopping the treatment. In conclusion, the tested combined nutraceutical was able to improve mildly but significantly several parameters related to metabolic syndrome in post-menopausal, both when compared to the baseline and to the control group. Further studies are needed to confirm the effectiveness of this approach on the long-term.
Acknowledgements
The tested product and the related placebo were kindly furnished by Pegaso Srl, Arbizzano di Negrar, VR, Italy. The authors are sincerely grateful to all the subjects who agreed to participate in this trial.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 22, Apr 2019Accepted: Thu 09, May 2019
Published: Tue 11, Jun 2019
Copyright
© 2023 Arrigo F.G. Cicero. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JFNM.2019.02.01
Author Info
Federica Fogacci Alessandro Colletti Arrigo F.G. Cicero Claudio Borghi Maddalena Veronesi Marilisa Bove Marina Giovannini
Corresponding Author
Arrigo F.G. CiceroDepartment of Medicine and Surgery Sciences, University of Bologna, Bologna, Italy
Figures & Tables
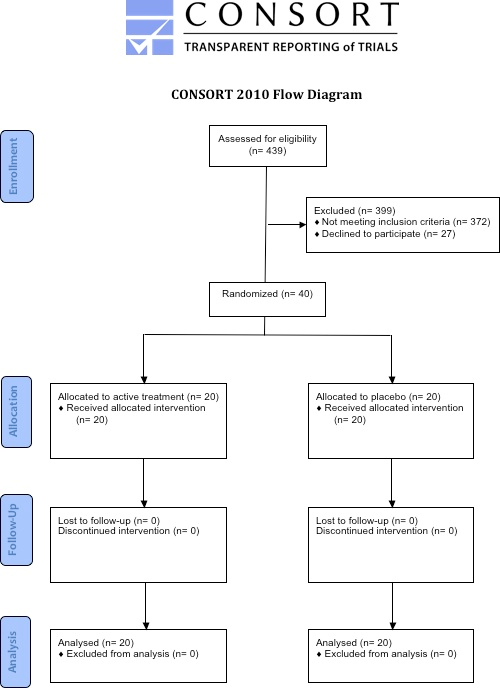
Table 1: Pre- and post-treatment values.
|
Parameters |
Active treatment |
Placebo treatment |
||||||
|
Pre-treatment |
Post-treatment |
Pre-treatment |
Post-treatment |
|||||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Waist circumference (cm) |
89.9 |
8.4 |
87.1 |
8.1 |
88.1 |
8.1 |
87.9 |
8.3 |
|
Body mass index (Kg/m2) |
26.9 |
1.4 |
26.8 |
1.2 |
26.8 |
1.3 |
26.8 |
1.3 |
|
Systolic blood pressure (mmHg) |
133.1 |
7.2 |
130.5 |
9.8 |
129.5 |
9.8 |
127.9 |
9.4 |
|
Diastolic blood pressure (mmHg) |
81.4 |
3.3 |
79.8 |
4.0 |
79.2 |
3.0 |
79.4 |
3.9 |
|
Total cholesterol (mg/dl) |
222.8 |
15.3 |
216.8* |
12.0 |
224.9 |
13.8 |
221.3 |
12.8 |
|
Triglycerides (mg/dl) |
206.9 |
25.3 |
141.1*° |
23.5 |
194.8 |
24.9 |
169.9* |
29.6 |
|
HDL-cholesterol (mg/dl) |
45.7 |
3.1 |
48.3*° |
3.4 |
44.1 |
3.5 |
45.6 |
3.3 |
|
LDL-cholesterol (mg/dl) |
137.8 |
12.3 |
141.3 |
12.1 |
142.3 |
10.1 |
142.6 |
13.5 |
|
Non-HDL-cholesterol (mg/dL) |
177.9 |
13.3 |
170.1* |
14.4 |
181.1 |
11.4 |
176.9 |
15.3 |
|
Fasting plasma glucose (mg/dl) |
114.6 |
4.6 |
98.3* |
3.8 |
115.1 |
3.9 |
108.9* |
4.1 |
|
Fasting plasma insulin (mcL/mL) |
19.9 |
3.1 |
17.1*° |
2.5 |
18.8 |
3.4 |
18.2 |
2.9 |
|
HOMA Index |
5.61 |
0.64 |
4.08*° |
0.73 |
5.44 |
0.63 |
5.23 |
0.87 |
|
High sensitivity C-reactive protein (mg/L) |
3.08 |
0.14 |
2.71* |
0.18 |
3.12 |
0.15 |
2.87 |
0.17 |
*P<0.05 vs baseline; °P<0.05 vs placebo
HDL= High-density lipoprotein; HOMA= Homeostasis model assessment of insulin resistance; LDL= Low-density lipoprotein; SD= Standard deviation.
Table 2: Row effect of the active treatment and of the placebo on glico-metabolic parameters.
|
Parameters |
Delta after treatment group |
Delta after placebo group |
||
|
Triglycerides (mg/dl) |
-66.6*° |
8.7 |
-25.3* |
4.8 |
|
HDL-cholesterol (mg/dl) |
+2.6*° |
0.8 |
+1.5 |
0.5 |
|
Non-HDL-cholesterol (mg/dL) |
-7.8* |
2.3 |
-4.1 |
1.4 |
|
Fasting plasma glucose (mg/dl) |
-16.2* |
3.9 |
-6.2* |
2.8 |
|
Fasting plasma insulin (mcL/mL) |
-2.8*° |
0.9 |
-0,6 |
0.4 |
|
HOMA Index |
-1.53*° |
0.25 |
-0.21 |
0.11 |
*P<0.05 vs baseline; °P<0.05 vs placebo
HDL= High-density lipoprotein ; HOMA= Homeostasis model assessment of insulin resistance.
References
- Honour JW (2018) Biochemistry of the menopause. Ann Clin Biochem 55: 18-33. [Crossref]
- Newson L (2018) Menopause and cardiovascular disease. Post Reprod Health 24: 44-49. [Crossref]
- Coyoy A, Guerra-Araiza C, Camacho-Arroyo I (2016) Metabolism Regulation by Estrogens and Their Receptors in the Central Nervous System Before and After Menopause. Horm Metab Res 48: 489-496. [Crossref]
- Hevener AL, Zhou Z, Drew BG, Ribas V (2017) The Role of Skeletal Muscle Estrogen Receptors in Metabolic Homeostasis and Insulin Sensitivity. Adv Exp Med Biol 1043: 257-284. [Crossref]
- Mendoza N, De Teresa C, Cano A, Godoy D, Hita-Contreras F et al. (2016) Benefits of physical exercise in postmenopausal women. Maturitas 93: 83-88. [Crossref]
- Jull J, Stacey D, Beach S, Dumas A, Strychar I et al. (2014) Lifestyle interventions targeting body weight changes during the menopause transition: a systematic review. J Obes 2014: 824310. [Crossref]
- Cicero AFG, Colletti A, Bellentani S (2018) Nutraceutical Approach to Non-Alcoholic Fatty Liver Disease (NAFLD): The Available Clinical Evidence. Nutrients 10. [Crossref]
- Caliceti C, Franco P, Spinozzi S, Roda A, Cicero AF (2016) Berberine: New Insights from Pharmacological Aspects to Clinical Evidences in the Management of Metabolic Disorders. Curr Med Chem 23: 1460-1476. [Crossref]
- Lan J, Zhao Y, Dong F, Yan Z, Zheng W et al. (2015) Meta-analysis of the effect and safety of berberine in the treatment of type 2 diabetes mellitus, hyperlipemia and hypertension. J Ethnopharmacol 161: 69-81. [Crossref]
- Yin J, Hu R, Chen M, Tang J, Li F et al. (2002) Effects of berberine on glucose metabolism in vitro. Metabolism 51: 1439-1443. [Crossref]
- Klein G, Kim J, Himmeldirk K, Cao Y, Chen X (2007) Antidiabetes and Anti-obesity Activity of Lagerstroemia speciosa. Evid Based Complement Alternat Med 4: 401-407. [Crossref]
- Stohs SJ, Miller H, Kaats GR (2012) A review of the efficacy and safety of banaba (Lagerstroemia speciosa L.) and corosolic acid. Phytother Res 26: 317-324. [Crossref]
- Cicero AF, Colletti A (2016) Role of phytochemicals in the management of metabolic syndrome. Phytomedicine 23: 1134-1144. [Crossref]
- Jurenka JS (2009) Anti-inflammatory properties of curcumin, a major constituent of Curcuma longa: a review of preclinical and clinical research. Altern Med Rev 14: 141-153. [Crossref]
- Meng B, Li J, Cao H (2013) Antioxidant and antiinflammatory activities of curcumin on diabetes mellitus and its complications. Curr Pharm Des 19: 2101-2113. [Crossref]
- Rochette L, Ghibu S, Muresan A, Vergely C (2015) Alpha-lipoic acid: molecular mechanisms and therapeutic potential in diabetes. Can J Physiol Pharmacol 93: 1021-1027. [Crossref]
- Vladeva SV, Terzieva DD, Arabadjiiska DT (2005) Effect of chromium on the insulin resistance in patients with type II diabetes mellitus. FoliaMed (Plovdiv) 47: 59-62. [Crossref]
- Valdés-Ramos R, Guadarrama-López AL, Martínez-Carrillo BE, Benítez-Arciniega AD (2015) Vitamins and type 2 diabetes mellitus. Endocr Metab Immune Disord Drug Targets 15: 54-63. [Crossref]
- Cicero AF, Colletti A (2016) Combinations of phytomedicines with different lipid lowering activity for dyslipidemia management: The available clinical data. Phytomedicine 23: 1113-1118. [Crossref]
- Cicero AFG, Fogacci F, Morbini M, Colletti A, Bove M et al. (2017) Nutraceutical Effects on Glucose and Lipid Metabolism in Patients with Impaired Fasting Glucose: A Pilot, Double-Blind, Placebo-Controlled, Randomized Clinical Trial on a Combined Product. High Blood Press Cardiovasc Prev 24: 283-288. [Crossref]
- Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI et al. (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Circulation 120: 1640-1645. [Crossref]
- Cicero AF, Rosticci M, Reggi A, Derosa G, Parini A et al. (2015) Relationship between serum uric acid and electrocardiographic alterations in a large sample of general population: data from the Brisighella Heart Study. High Blood Press Cardiovasc Prev 22: 129-134. [Crossref]
- Fogacci F, Cicero AF, D'Addato S, D'Agostini L, Rosticci M et al. (2017) Serum lipoprotein(a) level as long-term predictor of cardiovascular mortality in a large sample of subjects in primary cardiovascular prevention: data from the Brisighella Heart Study. Eur J Intern Med 37: 49-55. [Crossref]
- Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28: 412-419. [Crossref]
- Cicero AFG, Fogacci F, Giovannini M, Grandi E, Rosticci M et al. (2018) Serum uric acid predicts incident metabolic syndrome in the elderly in an analysis of the Brisighella Heart Study. Sci Rep 8: 11529. [Crossref]
- Cicero AF, Derosa G (2014) Are there mild and serious metabolic syndromes? The need for a graded diagnosis. J Cardiovasc Med 15: 759-760. [Crossref]
- Ambrosioni E, Cicero AF, Parretti D, Filippi A, Rossi A et al. (2008) Global cardiovascular disease risk management in Italian patients with metabolic syndrome in the clinical practice setting. High Blood Press Cardiovasc Prev 15: 37-45. [Crossref]
- Cicero AF, Tartagni E, Ertek S. Nutraceuticals for metabolic syndrome management: from laboratory to bench side. Curr Vasc Pharmacol 12: 565-571. [Crossref]
- Santana-Gálvez J, Cisneros-Zevallos L, Jacobo-Velázquez DA. Chlorogenic Acid: Recent Advances on Its Dual Role as a Food Additive and a Nutraceutical against Metabolic Syndrome. Molecules 22. [Crossref]
- Cicero AF, Baggioni A (2016) Berberine and Its Role in Chronic Disease. Adv Exp Med Biol 928: 27-45. [Crossref]
- Chuengsamarn S, Rattanamongkolgul S, Luechapudiporn R, Phisalaphong C, Jirawatnotai S (2012) Curcumin extract for prevention of type 2 diabetes. Diabetes Care 35: 2121-2127. [Crossref]
- Ali A, Ma Y, Reynolds J, Wise JP Sr, Inzucchi SE et al. (2011) Chromium effects on glucose tolerance and insulin sensitivity in persons at risk for diabetes mellitus. Endocr Pract 17: 16-25. [Crossref]
