Draping for Minimally-Invasive Hypopharyngeal Sleep Surgery using a Nasotracheal Tube: Surgical Technique
A B S T R A C T
Nasotracheal intubation is widely used for elective maxillofacial and ENT surgery and allows a superior visual field during sleep surgery. Traditional draping methods can result in nasal injury. We describe an alternative method of draping during nasotracheal intubation which avoids this risk.
Keywords
Intubation, obstructive sleep apnea, nasal cartilages, minimally invasive surgical procedures
Introduction
Minimally-invasive sleep surgery encompasses a variety of techniques to reduce the burden of sleep-disordered breathing and obstructive sleep apnea. The aim is to increase the dimensions of the upper airway thus allowing reduced obstruction during muscular hypotonia associated with sleep. There is no clear definition for the minimally-invasive aspect to sleep surgery, but the principle is to reduce the surgical morbidity and allow for a quicker recovery. The procedures are variable but include palatoplasty, pharyngoplasty, epiglottoplasty and radiofrequency treatment to the nose, palate and the base of tongue [1].
Minimally-invasive sleep surgery requires an optimal view of the oropharynx, but more importantly of the tongue base and epiglottis. Although it is possible to perform the procedure with an orotracheal tube, using a nasotracheal tube allows for a superior visual field and improved access to the hypopharynx [2]. This is particularly important when operating on the tongue base and epiglottis. It also reduces the need to move the tube side to side during surgery. Using a nasotracheal tube can therefore enhance the ease and timing of the overall procedure. Nasotracheal intubation is widely used for maxillofacial surgery and ENT surgery and is within the skill set for the majority of anaesthetists [2, 3].
Although oral surgery is not sterile due to natural intraoral bacterial colonization, we aim to keep the surrounding area as clean as possible [4]. This involves using a body-drape to cover the body and a head-drape to cover the nasotracheal tube. We have discussed our draping preference when using the head-drape to cover the nasotracheal tube.
Technical Description
Traditionally, the head-drape is used to cover the nose and nasotracheal tube completely. The distinct advantage of this method is a reduced area of exposed tube and nasal tip. However, the drape in this position compresses the tube and exaggerates the cranial bend. Although in principle this could affect ventilation, we have not found this to be an issue. We have found that the exaggerated bend exerts increased pressure on the alar rim and this can result in a soft tissue injury (Figure 1). In the short-term, we have seen this to cause alar erythema and deformity which can take hours to resolve. There are several reports in the literature of nasal intubation resulting in alar necrosis [5-7].
Since visualizing this injury, we recommend an alternative method of using the head-drape in the presence of a nasotracheal tube. The drape is placed superior to the nasal tip, approximately overlying the nasal bridge and a wet swab is placed between the nasal skin and the nasotracheal tube (Figure 2). The nasotracheal tube is thus secured at the nasal bridge under the tension of the head drape. This allows the nasotracheal tube to place little, if any, tension on the alar cartilage. In our experience this has resulted in no soft tissue nasal injury.
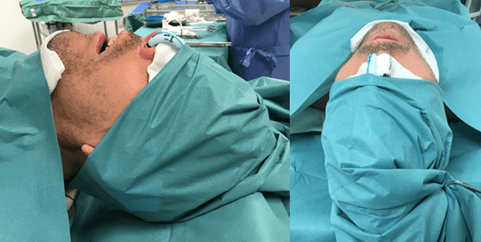
Figure 1: Traditional draping covering nasotracheal tube, resulting in alar erythema within minutes.
Figure 2: Proposed draping method to prevent alar injury.
Discussion
The clear disadvantage is an increased area of skin and nasotracheal tube which is exposed during the surgery. Our argument follows that the procedure is clean, not sterile, and therefore matches the draping in other common ENT procedures such as adenotonsillectomy, where the tube is completely exposed in the oral cavity and the nasal tip is exposed to assist with the adenoidectomy. In adenotonsillectomy this has been shown to result in no increased risk of infection [4].
It is widely accepted that the need to drape is important for two additional reasons. Firstly, this allows a reduction of foreign material such as hair disturbing the operative field and secondly, it prevents inadvertent injury to the patient by creating a barrier between any instruments and the skin. Other methods have been described in the literature for reducing the risk of alar soft tissue injury, including the use of Merocel sponge, modifying the position of the nasotracheal tube and placing a hydrocolloid dressing [5-7]. Our preference is to use the described method as it’s the simplest and doesn’t require additional materials.
We propose draping patients undergoing procedures with nasotracheal intubation with the nasal tip exposed to prevent alar injury. This method protects the alar skin, enhances the visual field and does not appear to decrease the cleanliness of the field.
Summary
i. Nasotracheal intubation can be used for any surgery within the oral cavity.
ii. Nasotracheal intubation is particularly preferable for minimally invasive sleep surgery as it provides optimal access.
iii. Care should be taken when draping to prevent inadvertent injury to the external nose.
Acknowledgement
Not applicable.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Technical NotePublication history
Received: Fri 29, Apr 2022Accepted: Mon 04, Jul 2022
Published: Fri 15, Jul 2022
Copyright
© 2023 Ankit Patel . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2022.07.03
Author Info
Ankit Patel Amro Hassan Thusith Wickrama Bhik Kotecha
Corresponding Author
Ankit PatelQueen’s Hospital, Romford, UK
Figures & Tables

References
1. Kotecha B (2017)
Updated Minimally Invasive Surgery for Sleep-Related Breathing Disorders. Adv
Otorhinolaryngol 80: 90-98. [Crossref]
2. Folino TB, Mckean
G, Parks LJ (2021) Nasotracheal Intubation. StatPearls Publishing, Treasure
Island (FL). [Crossref]
3. Yamamoto T, Flenner
M, Schindler E (2019) Complications associated with nasotracheal intubation and
proposal of simple countermeasure. Anaesthesiol Intensive Ther 51:
72-73. [Crossref]
4. Emko P, Sullivan RL
(1978) Clean technique versus sterile technique for tonsillectomy and
adenoidectomy. N Y State J Med 78: 756-757. [Crossref]
5. Anand R, Turner M,
Sharma S, Mourouzis C, Mellor TK et al. (2007) Use of a polyvinyl acetyl sponge
(Merocel) nasal pack to prevent alar necrosis during prolonged nasal
intubation. Br J Oral Maxillofac Surg 45: 601. [Crossref]
6. Cherng CH, Chen YW (2010) Using a modified nasotracheal tube to prevent nasal ala pressure sore during prolonged nasotracheal intubation. J Anesth 24: 959-961. [Crossref]
7. Iwai T, Goto T, Maegawa J, Tohnai I (2011) Use of a hydrocolloid dressing to prevent nasal pressure sores after nasotracheal intubation. Br J Oral Maxillofac Surg 49: e65-e66. [Crossref]
