Descending Aorta Finger Clamping to Control Intra-Abdominal Bleeding Due to Rupture of Anterior Superior Pancreaticoduodenal Artery Aneurysm
A B S T R A C T
Background: Open aortic cross-clamping via a resuscitative left thoracotomy is effective in maintaining adequate blood pressure in patients with abdominal bleeding until achieving hemostasis. However, the procedure to encircle the descending aorta to secure cross-clamping is technically demanding for general surgeons, especially in emergency situations.
Case Presentation: We report a case of rupture of the anterior superior pancreaticoduodenal artery aneurysm associated with median arcuate ligament syndrome, which required surgical hemostasis. Because of severe hypotension after laparotomy, open aortic cross-clamping with a left thoracotomy was performed by general surgeons. However, the aortic clamps repeatedly slipped off because the clamping was conducted without encircling the aorta. Then, we attempted finger clamping of the descending aorta, and the blood pressure was quite effectively stabilized.
Conclusion: Descending aorta finger clamping via a resuscitative left thoracotomy is easy and feasible and might be an effective procedure to maintain adequate blood pressure for general surgeons.
Keywords
Descending aorta finger clamping, open aortic cross-clamping via, resuscitative left thoracotomy, median arcuate ligament syndrome, (MALS), abdominal bleeding
Introduction
Abdominal bleeding is a life-threatening condition requiring a quick and adequate approach in order to achieve hemostasis. Open aortic cross-clamping via a resuscitative left thoracotomy (open-ACC) is reported to be remarkably effective in maintaining adequate blood pressure in patients with abdominal bleeding [1, 2]. The aortic occlusion is typically performed by using aortic clamps and taping of the descending aorta is required to avoid slipping of the aortic clamps or insufficient aortic clamping [3]. However, encircling of the descending aorta is technically demanding and sometimes difficult for general surgeons, especially in emergency situations. In this report, we present a case of severe abdominal bleeding due to rupture of anterior superior pancreaticoduodenal artery aneurysm wherein descending aorta finger clamping was quite effective in maintaining adequate blood pressure during surgical hemostasis.
Case Presentation
An 83-year-old-man was delivered to our hospital due to impaired consciousness. Abdominal computed tomography (CT) showed a massive hematoma in the upper abdomen and stenosis of the stem of the celiac artery associated with median arcuate ligament syndrome (MALS) (Figures 1A & 1B) [4]. The radiologists performed interventional radiology (IVR), and active bleeding from Anterior superior pancreaticoduodenal artery (ASPDA) aneurysm was observed (Figure 1C). Although transcatheter arterial embolization was attempted, the approach to the aneurysm was quite difficult because of arteriosclerosis and angiospasm of the ASPDA; as a result, emergency surgical hemostasis was scheduled.
Figures 1: A) Axial CT view in the arterial phase on admission. A massive hematoma in the upper abdomen (*) and an arterial extravasation located at the anterior surface of the pancreatic head (arrow) were observed. B) Sagittal CT view in the arterial phase on admission. Severe stenosis at the root of the celiac artery was observed (arrowhead). *, hematoma. C) Angiographic image during IVR. Active bleeding was observed from an aneurysm on ASPDA (arrowhead). ASPDA: Anterior superior pancreaticoduodenal artery; CT: Computed tomography; IVR: Interventional radiology.
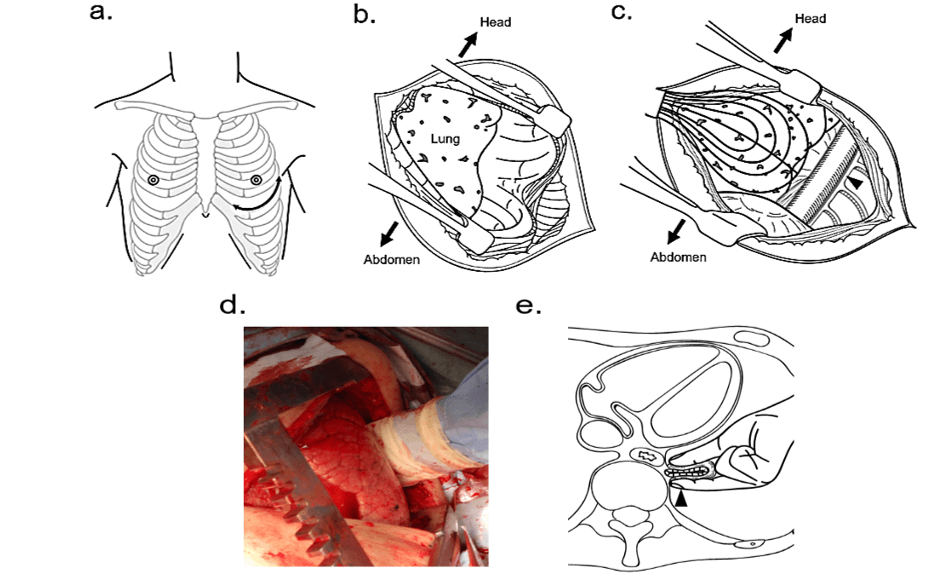
Figures 2: Procedure of open-ACC with finger clamping. A) Skin incision through the left fifth intercostal space. B) Extension of the left thoracotomy using a chest opener. C) Retraction of the left lung to identify the descending aorta (arrowhead). D) Intraoperative photograph of descending aorta finger clamping under a left thoracotomy. E) The schema of descending aorta finger clamping (arrowhead) through gauze under a left thoracotomy. Open-ACC: open aortic cross-clamping via resuscitative left thoracotomy.
Following the laparotomy, his blood pressure dropped down to 70/40 mmHg, and therefore, we performed abdominal gauze packing and massive blood transfusion. Since the blood pressure remained low, we then switched to perform open-ACC in an attempt to stabilize the patient’s blood pressure. We made an incision through the fifth intercostal space to perform the left thoracotomy (Figure 2A), extended the thoracotomy to the left using a chest opener (Figure 2B), retracted the left lung, and identified the descending aorta (Figure 2C). Initially, we clamped the descending aorta using aortic clamps without incising the pleura or taping the descending aorta. However, the blood pressure was not stabilized because the aortic clamps repeatedly slipped. We switched to finger clamping through gauze (Figures 2D & 2E); following this change, the patient’s blood pressure stabilized.
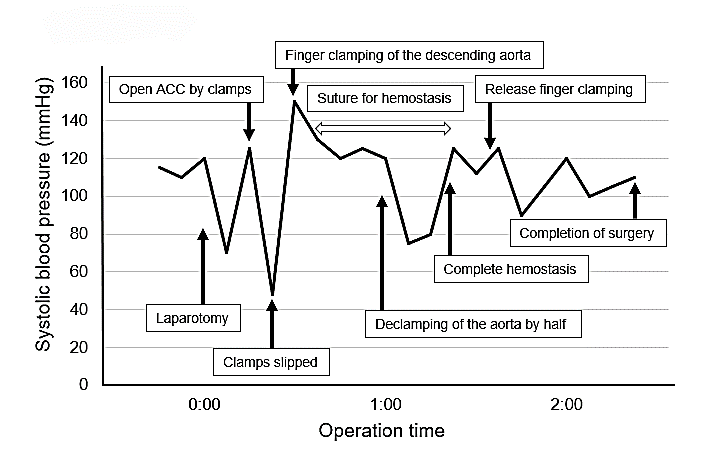
Then, we returned to the abdominal surgery and complete hemostasis was obtained by suturing. The operative time was 2 hours 31 minutes. The transition of systolic blood pressure during surgery was summarized in (Figure 3).
Figures 3: Transition of systolic blood pressure during surgery. Blood pressure dropped sharply after the laparotomy. Although open-ACC with aortic clamps was performed, the clamps repeatedly slipped off. The patient’s blood pressure stabilized after descending aorta finger clamping, and surgical hemostasis for abdominal bleeding was successfully achieved. Open-ACC: open aortic cross-clamping via resuscitative left thoracotomy.
During the postoperative course, the patient developed pneumonia and was treated with antibiotics, temporary tracheotomy, and rehabilitation therapy. Although it took the patients a considerable time to recover, he was discharged on POD 125.
Discussion
In the case of abdominal bleeding, control of blood pressure and rapid hemostasis are important to avoid cardiac arrest and neurological injuries by redistributing the intravascular volume to the coronary and carotid arteries [5]. Open-ACC is reported to be remarkably effective at maintaining adequate blood pressure in patients with abdominal bleeding by blocking the arterial flow to the area below the diaphragm, decreasing blood loss in the abdominal cavity and ensuring that the blood flow is restricted to the upper body [1, 2, 5-7]. However, open-ACC can be highly invasive, and the procedure is reportedly associated with fatal complications such as secondary bleeding, infection, and spinal cord ischemia [8, 9].
Recently, resuscitative endovascular balloon occlusion of the aorta (REBOA) has been used to control blood pressure during abdominal bleeding and some reports revealed that REBOA was associated with lower complications and mortality than open-ACC [10-12]. Although REBOA has recently become the main method of aortic occlusion, open-ACC is still required in cases with a rapid decrease in blood pressure or in cases where there are reduced facilities and human resources for IVR because REBOA requires some knack and pitfalls to prevent complications. Generally, aortic occlusion is achieved more rapidly by open-ACC than REBOA, and open-ACC also has the advantage of open cardiac massage in case of cardiac arrest. For these reasons, open-ACC remains an indispensable procedure for general surgeons in case of abdominal bleeding. However, open-ACC is technically demanding since the adequate procedure to avoid slipping of the aortic clamps includes encircling the descending aorta, so as not to injure the Adamkiewicz artery [3, 13]. Therefore, open-ACC is sometimes difficult for general surgeons who are unfamiliar with the anatomical structure around the descending thoracic aorta.
In the present case, we performed surgical hemostasis for a patient with ASPDA aneurysm rupture associated with MALS. Because his blood pressure was stable after IVR, REBOA was not conducted before the surgery. However, his blood pressure dropped sharply after the laparotomy, and thus, open-ACC was performed by general surgeons, resulting in insufficient clamping because the descending aorta was not taped. We subsequently performed descending aorta finger clamping and obtained adequate blood pressure control and rapid surgical hemostasis. Open-ACC with finger clamping is an easy and feasible procedure to provide stabilization of blood pressure and would be useful, especially for general surgeons in emergency situations.
Conclusion
We experienced a case of severe abdominal bleeding wherein descending aorta finger clamping under left thoracotomy was quite effective at maintaining adequate blood pressure during surgical hemostasis. Open-ACC with finger clamping would be an easy and feasible procedure for general surgeons in emergency situations.
Acknowledgment
None.
Ethical Approval
This article satisfied the consensus of the National Center for Global Health and Medicine Research Ethics Committee/Institutional Review Board.
Consent
Informed consent was obtained from the patient presented in this article.
Availability of Data and Materials
The datasets analyzed during the current study are not publicly available due to their containing information that could compromise the privacy of research participants but are available from the corresponding author on reasonable request.
Competing Interests
None.
Author Contributions
KY, KI and NT contributed to the conception and design of the study. All authors contributed to the acquisition and analysis of data. KY, KI, and NT were a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Abbreviation
ASPDA: Anterior superior pancreaticoduodenal artery
CT: Computed tomography
IVR: Interventional radiology
MALS: Median arcuate ligament syndrome
Open-ACC: Open aortic cross-clamping via resuscitative left thoracotomy
REBOA: Resuscitative endovascular balloon occlusion of the aorta
Article Info
Article Type
Case ReportPublication history
Received: Fri 17, Apr 2020Accepted: Mon 04, May 2020
Published: Tue 12, May 2020
Copyright
© 2023 Nobuyuki Takemura. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.05.03
Author Info
Fuminori Mihara Hayato Ono Hitomi Wake Kaito Yano Kyoji Ito Nobuyuki Takemura Norihiro Kokudo
Corresponding Author
Nobuyuki TakemuraHepato-Biliary-Pancreatic Surgery Division, Department of Surgery, National Center for Global Health and Medicine, Tokyo, Japan
Figures & Tables

References
- Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons Committee on Trauma (2001) Practice management guidelines for emergency department thoracotomy. Working Group, Ad Hoc Subcommittee on Outcomes, American College of Surgeons-Committee on Trauma. J Am Coll Surg 193: 303-309. [Crossref]
- Dunn EL, Moore EE, Moore JB (1982) Hemodynamic effects of aortic occlusion during hemorrhagic shock. Ann Emerg Med 11: 238-241. [Crossref]
- Desai CS, Girlanda R, Hawksworth J, Fishbein TM (2014) Modified technique for aortic cross‐clamping during liver donor procurement. Clin Transplant 28: 611-615. [Crossref]
- Horton KM, Talamini MA, Fishman EK (2005) Median arcuate ligament syndrome: evaluation with CT angiography. Radiographics 25: 1177-1182. [Crossref]
- Millikan JS, Moore EE (1984) Outcome of resuscitative thoracotomy and descending aortic occlusion performed in the operating room. J Trauma 24: 387-392. [Crossref]
- Moore LJ, Brenner M, Kozar RA, Pasley J, Wade CE et al. (2015) Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg 79: 523-532. [Crossref]
- Spence PA, Lust RM, Chitwood WR Jr, Iida H, Sun YS et al. (1990) Transfemoral balloon aortic occlusion during open cardiopulmonary resuscitation improves myocardial and cerebral blood flow. J Surg Res 49: 217-221. [Crossref]
- Connery C, Geller E, Dulchavsky S, Kreis DJ Jr. (1990) Paraparesis following emergency room thoracotomy: case report. J Trauma 30: 362-363. [Crossref]
- Cothren CC, Moore EE (2006) Emergency department thoracotomy for the critically injured patient: Objectives, indications, and outcomes. World J Emerg Surg 1: 4. [Crossref]
- Brenner ML, Moore LJ, DuBose JJ, Tyson GH, McNutt MK et al. (2013) A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg 75: 506-511. [Crossref]
- Martinelli T, Thony F, Decléty P, Sengel C, Broux C et al. (2010) Intra-aortic balloon occlusion to salvage patients with life-threatening hemorrhagic shocks from pelvic fractures. J Trauma 68: 942-948. [Crossref]
- White JM, Cannon JW, Stannard A, Markov NP, Spencer JR et al. (2011) Endovascular balloon occlusion of the aorta is superior to resuscitative thoracotomy with aortic clamping in a porcine model of hemorrhagic shock. Surgery 150: 400-409. [Crossref]
- Tanaka H, Ogino H, Minatoya K, Matsui Y, Higami T et al. (2016) The impact of preoperative identification of the Adamkiewicz artery on descending and thoracoabdominal aortic repair. J Thorac Cardiovasc Surg 151: 122-128. [Crossref]
